Abstract
Summary
Perfusion of the pelvic bone marrow is reduced in the postmenopausal group and with age. Quantitative dynamic contrast-enhanced MRI could reflect the blood supply characteristics and hemodynamic changes of the pelvic bone marrow. These results contribute to the description of osteoporosis in the postmenopausal females and the elderly.
Introduction
To investigate the effect of menstrual status and age on the perfusion of pelvic bone marrow in adult females using quantitative dynamic contrast-enhanced MRI (DCE-MRI).
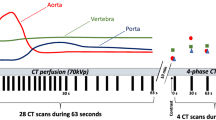
Methods
In total, 96 adult females who underwent DCE-MRI between September 2017 and December 2017 were included. All the subjects’ quantitative DCE-MRI parameters of pelvic bone marrow were measured and retrospectively analyzed, including Ktrans (volume transfer constant), Kep (efflux rate constant), and Ve (interstitial volume). According to their menstrual status, the subjects were divided into a premenopausal group (n = 39) and a postmenopausal group (n = 57), and the two groups were then divided into four subgroups according to age. The intraobserver reliability was assessed by the intraclass correlation coefficient (ICC). The parameters were compared between different menstrual status groups and age subgroups by Mann-Whitney test, and Spearman correlation analysis was used to evaluate the correlation between the age and the quantitative parameters.
Results
The ICCs of the Ktrans, Kep, and Ve values were 0.989, 0.974, and 0.920, respectively. Ktrans, Kep, and Ve of the premenopausal group were significantly higher than those of the postmenopausal group (P < 0.05). The overall age was negatively correlated with Ktrans, Kep, and Ve (r = − 0.590, − 0.357, and − 0.381, respectively, P < 0.05). In the premenopausal group, Ktrans and Ve were significantly higher in subgroup 1 (≤ 40 years) compared with subgroup 2 (> 40 years) (P < 0.05), and age showed a negative correlation with Ktrans and Ve (r = − 0.344 and − 0.334, respectively, P < 0.05). In the postmenopausal group, Ktrans and Kep were significantly higher in subgroup 3 (≤ 60 years) compared with subgroup 4 (> 60 years) (P < 0.05), and age showed a negative correlation with Ktrans and Kep (r = − 0.460 and − 0.303, respectively, P < 0.05).
Conclusion
Menstrual status and age have significant effects on the perfusion of the pelvic bone marrow microenvironment in adult females and that the microenvironment of the pelvic bone marrow displays different changes at different age stages. Quantitative DCE-MRI has contributed to the interpretation of the pelvic bone marrow perfusion status.




Similar content being viewed by others
References
Collin-Osdoby P (1994) Role of vascular endothelial cells in bone biology. J Cell Biochem 55(3):304–309
Nouh MR, Eid AF (2015) Magnetic resonance imaging of the spinal marrow: basic understanding of the normal marrow pattern and its variant. World J Radiol 7(12):448–458
Chen WT, Shih TT, Chen RC et al (2001) Vertebral bone marrow perfusion evaluated with dynamic contrast-enhanced MR imaging: significance of aging and sex. Radiology 220(1):213–218
Griffith JF, Yeung DK, Antonio GE et al (2006) Vertebral marrow fat content and diffusion and perfusion indexes in women with varying bone density: MR evaluation. Radiology 241(3):831–838
Griffith JF, Wang YX, Zhou H, Kwong WH, Wong WT, Sun YL et al (2010) Reduced bone perfusion in osteoporosis: likely causes in an ovariectomy rat model. Radiology 254(3):739–746
Wáng YXJ, Griffith JF, Deng M, Yeung DKW, Yuan J (2015) Rapid increase in marrow fat content and decrease in marrow perfusion in lumbar vertebra following bilateral oophorectomy: an MR imaging-based prospective longitudinal study. Korean J Radiol 16(1):154–159
Biffar A, Dietrich O, Sourbron S, Duerr HR, Reiser MF, Baur-Melnyk A (2010) Diffusion and perfusion imaging of bone marrow. Eur J Radiol 76(3):323–328
Biffar A, Sourbron S, Dietrich O, Schmidt G, Ingrisch M, Reiser MF, Baur-Melnyk A (2010) Combined diffusion-weighted and dynamic contrast-enhanced imaging of patients with acute osteoporotic vertebral fractures. Eur J Radiol 76(3):298–303
Zhu J, Xiong Z, Zhang J, Qiu Y, Hua T, Tang G (2017) Comparison of semi-quantitative and quantitative dynamic contrast-enhanced MRI evaluations of vertebral marrow perfusion in a rat osteoporosis model. BMC Musculoskelet Disord 18(1):446
Breault SR, Heye T, Bashir MR et al (2013) Quantitative dynamic contrast-enhanced MRI of pelvic and lumbar bone marrow: effect of age and marrow fat content on pharmacokinetic parameter values. AJR Am J Roentgenol 200(3):297–303
Sourbron SP, Buckley DL (2013) Classic models for dynamic contrast-enhanced MRI. NMR Biomed 26(8):1004–1027
Karampinos DC, Ruschke S, Dieckmeyer M et al (2018) Quantitative MRI and spectroscopy of bone marrow. J Magn Reson Imaging 47(2):332–353
Tofts PS (1997) Modeling tracer kinetics in dynamic Gd-DTPA MR imaging. J Magn Reson Imaging 7(1):91–101
Le Y, Dale B, Akisik F et al (2016) Improved T1, contrast concentration, and pharmacokinetic parameter quantification in the presence of fat with two-point Dixon for dynamic contrast-enhanced magnetic resonance imaging. Magn Resone Med 75(4):1677–1684
Zhu J, Zhang L, Wu X, Xiong Z, Qiu Y, Hua T, Tang G (2017) Reduction of longitudinal vertebral blood perfusion and its likely causes: a quantitative dynamic contrast-enhanced MR imaging study of a rat osteoporosis model. Radiology 282(2):369–380
Bourque SL, Davidge ST, Adams MA (2011) The interaction between endothelin-1 and nitric oxide in the vasculature: new perspectives. Am J Physiol Regul Integr Comp Physiol 300(6):1288–1295
Lekontseva O, Chakrabarti S, Davidge ST (2010) Endothelin in the female vasculature: a role in aging? Am J Physiol Regul Integr Comp Physiol 298(3):509–516
Basu S, Houseni M, Bural G, Chamroonat W, Udupa J, Mishra S et al (2007) Magnetic resonance imaging based bone marrow segmentation for quantitative calculation of pure red marrow metabolism using 2-deoxy-2-[F-18]fluoro-D-glucose-positron emission tomography: a novel application with significant implications for combined structure-function approach. Mol Imaging Biol 9(6):361–365
Duque G (2008) Bone and fat connection in aging bone. Curr Opin Rheumatol 20(4):429–434
Limonard EJ, Veldhuis-Vlug AG, Van DL et al (2015) Short-term effect of estrogen on human bone marrow fat. J Bone Miner Res 30(11):2058–2066
Ito H (2014) Clinical considerations of regenerative medicine in osteoporosis. Curr Osteoporos Rep 12(2):230–234
Hardouin P, Rharass T, Lucas S (2016) Bone marrow adipose tissue: to be or not to be a typical adipose tissue? Front Endocrinol (Lausanne) 7:85
Schwartz AV, Sigurdsson S, Hue TF, Lang TF, Harris TB, Rosen CJ, Vittinghoff E, Siggeirsdottir K, Sigurdsson G, Oskarsdottir D, Shet K, Palermo L, Gudnason V, Li X (2013) Vertebral bone marrow fat associated with lower trabecular BMD and prevalent vertebral fracture in older adults. J Clin Endocrinol Metab 98(6):2294–2300
Adams JE (2013) Advances in bone imaging for osteoporosis. Nat Rev Endocrinol 9(1):28–42
Hillengass J, Stieltjes B, Bauerle T et al (2011) Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) and diffusion-weighted imaging of bone marrow in healthy individuals. Acta Radiol 52:324–330
Roldan-Valadez E, Piña-Jimenez C, Favila R et al (2013) Gender and age groups interactions in the quantification of bone marrow fat content in lumbar spine using 3T MR spectroscopy: a multivariate analysis of covariance (Mancova). Eur J Radiol 82(11):697–702
Baum T, Rohrmeier A, Syväri J, Diefenbach MN, Franz D, Dieckmeyer M, Scharr A, Hauner H, Ruschke S, Kirschke JS, Karampinos DC (2018) Anatomical variation of age-related changes in vertebral bone marrow composition using chemical shift encoding-based water-fat magnetic resonance imaging. Front Endocrinol (Lausanne) 9:141
Liu Y, Cao L, Hillengass J, Delorme S, Schlewitz G, Govindarajan P, Schnettler R, Heiß C, Bäuerle T (2013) Quantitative assessment of microcirculation and diffusion in the bone marrow of osteoporotic rats using VCT, DCE-MRI, DW-MRI, and histology. Acta Radiol 54:205–213
Justesen J, Stenderup K, Ebbesen EN, Mosekilde L, Steiniche T, Kassem M (2001) Adipocyte tissue volume in bone marrow is increased with aging and in patients with osteoporosis. Biogerontology 2(3):165–171
Chen WT, Ting-Fang ST, Hu CJ et al (2004) Relationship between vertebral bone marrow blood perfusion and common carotid intima-media thickness in aging adults. J Magn Reson Imaging 20(5):811–816
Prisby RD (2014) Bone marrow blood vessel ossification and “microvascular dead space” in rat and human long bone. Bone 64:195–203
Laroche M (1996) Arteriosclerosis and osteoporosis. Presse Med 25(2):52–54
Valentinitsch A, Trebeschi S, Alarcon E, Baum T, Kaesmacher J, Zimmer C et al (2017) Regional analysis of age-related local bone loss in the spine of a healthy population using 3D voxel-based modeling. Bone 103:233–240
Maciel JG, de Araújo IM, Carvalho AL, Simão MN, Bastos CM, Troncon LEA, Salmon CEG, de Paula FJA, Nogueira-Barbosa MH (2017) Marrow fat quality differences by sex in healthy adults. J Clin Densitom 20(1):106–113
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 537 kb)
Rights and permissions
About this article
Cite this article
Zhang, X., Pang, H., Dong, Y. et al. A study of dynamic contrast-enhanced MR imaging features and influence factors of pelvic bone marrow in adult females. Osteoporos Int 30, 2469–2476 (2019). https://doi.org/10.1007/s00198-019-05145-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05145-w