Abstract
Purpose
To compare theoretical values from the small incision lenticule extraction (SMILE) lenticule thickness readout with change in axial length measurements taken with the IOLMaster.
Methods
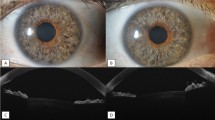
We prospectively studied 214 eyes from 107 patients undergoing bilateral SMILE surgery for myopia or myopic astigmatism between December 2014 and May 2017 at an ophthalmological practice in Singapore. All eyes were examined pre-operatively and 1 and 3 months post-operatively with the IOLMaster following SMILE surgery. Achieved lenticule thickness was taken as the change in axial length after surgery. A linear mixed-effects model was used to examine changes in axial length, spherical equivalent and acuity over time. The relationships between change in axial length and theoretical lenticule thickness and spherical equivalent were examined with multiple linear regression analyses, and model prediction was assessed with adjusted R2 statistics.
Results
Mean (95% confidence interval [CI]) spherical equivalent pre-operatively was − 5.25 (95% CI − 5.38 to − 5.12) diopters (D), at 1 month was 0.04 (95% CI − 0.09 to 0.17) D (p < 0.001), and at 3 months was − 0.02 (95% CI − 0.15 to 0.11) D (p < 0.001). Mean (95% CI) pre-operative axial length was 27,726 (95% CI 25,595 to 25,857) μm. Post-operative axial length at 1 month was significantly shorter at 25,595 (95% CI 25,464 to 25,726) μm (p < 0.001) with no change thereafter (p = 0.647). Pre-operative mean ± standard deviation (SD) refractive target was 0.24 (± 0.3) D, and mean difference between target and post-operative spherical equivalent at 1 month was 0.20 D (95% CI 0.16 to 0.25 D, p < 0.001). Multiple regression analysis showed that change in axial length at 1 month was, on average, 5% lower than theoretical lenticule thickness, indicating an average difference of 5.4 μm (95% CI 5.2 to 5.6 μm). Preoperative spherical equivalent predicted negative association with change in axial length at 1 month (β = − 14.8, 95% CI − 18.2 to − 11.3, adjusted R2 = 0.457, p < 0.001).
Conclusions
Calculated lenticule thickness values were less than expected, and post-operative refractive outcomes at 1 month showed a slight under-correction. Further research in this area is needed to validate these findings.


Similar content being viewed by others
References
Stulting RD, Lahners WJ, Carr JD (2000) Advances in refractive surgery: 1975 to present. Cornea 19:741–753
SMILE—laser vision correction. Carl Zeiss Meditec AG website. https://www.zeiss.com/meditec/int/c/smile/laser-vision-correction.html. Accessed December 10, 2018.
Shah R, Shah S, Sengupta S (2011) Results of small incision lenticule extraction: all-in-one femtosecond laser refractive surgery. J Cataract Refract Surg 37:127–137. https://doi.org/10.1016/j.jcrs.2010.07.033
Sekundo W, Kunert KS, Blum M (2011) Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol 95:335–339. https://doi.org/10.1136/bjo.2009.174284
Liu M, Chen Y, Wang D et al (2016) Clinical outcomes after SMILE and femtosecond laser-assisted LASIK for myopia and myopic astigmatism: a prospective randomized comparative study. Cornea 35:210–216
Zhang Y, Shen Q, Jia Y, Zhou D, Zhou J (2016) Clinical outcomes of SMILE and FS-LASIK used to treat myopia: a meta-analysis. J Refract Surg 32:256–265. https://doi.org/10.3928/1081597X-20151111-06
Mohamed-Noriega K, Riau AK, Lwin NC, Chaurasia SS, Tan DT, Mehta JS (2014) Early corneal nerve damage and recovery following small incision lenticule extraction (SMILE) and laser in situ keratomileusis (LASIK). Invest Ophthalmol Vis Sci 55:1823–1834
Wu D, Wang Y, Zhang L, Wei SS, Tang X (2014) Corneal biomechanical effects: Small incision lenticule extraction versus femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg 40:954–962. https://doi.org/10.1016/j.jcrs.2013.07.056
Reinstein DZ, Archer TJ, Randleman JB (2013) Mathematical model to compare the relative tensile strength of the cornea after PRK, Lasik and small incision lenticule extraction. J Refract Surg 29:454–460. https://doi.org/10.3928/1081597X-20130617-03
Sinha Roy A, Dupps WJ Jr, Roberts CJ (2014) Comparison of biomechanical effects of small incision lenticule extraction and laser in situ keratomileusis: finite element analysis. J Cataract Refract Surg 40:971–980. https://doi.org/10.1016/j.jcrs.2013.08.065
Seven I, Vahdati A, Pedersen IB et al (2017) Contralateral eye comparison of SMILE and flap-based corneal refractive surgery: computational analysis of biomechanical impact. J Refract Surg 33:444–453. https://doi.org/10.3928/1081597X-20170504-01
Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD (2003) Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology 110:267–275. https://doi.org/10.1016/S0161-6420(02)01727-X
Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB (2013) Designing clinical research. Lippincott Williams & Wilkins, Philadelphia
Armstrong RA (2013) Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol Opt 33:7–14. https://doi.org/10.1111/opo.12009
Kim WS, Jo JM (2001) Corneal hydration affects ablation during laser in situ keratomileusis surgery. Cornea 20:394–397
Ju WK, Lee JH, Chung TY, Chung ES (2011) Reproducibility of LASIK flap thickness using the Zeiss femtosecond laser measured postoperatively by optical coherence tomography. J Refract Surg 27:106–110. https://doi.org/10.3928/1081597X-20100428-04
Lim DH, Keum JE, Ju WK, Lee JH, Chung TY, Chung ES (2013) Prospective contralateral eye study to compare 80- and 120-μm flap LASIK using the VisuMax femtosecond laser. J Refract Surg 29:462–468. https://doi.org/10.3928/1081597X-20130617-04
Reinstein DZ, Archer TJ, Gobbe M, Johnson N (2010) Accuracy and reproducibility of artemis central flap thickness and visual outcomes of LASIK with the Carl Zeiss Meditec VisuMax femtosecond laser and MEL 80 excimer laser platforms. J Refract Surg 26:107–119. https://doi.org/10.3928/1081597X-20100121-06
Reinstein DZ, Archer TJ, Gobbe M (2013) Accuracy and reproducibility of cap thickness in small incision lenticule extraction. J Refract Surg 29:810–805. https://doi.org/10.3928/1081597X-20131023-02
Tay E, Li X, Chan C, Tan DT, Mehta JS (2012) Refractive lenticule extraction flap and stromal bed morphology assessment with anterior segment optical coherence tomography. J Cataract Refract Surg 38:1544–1551. https://doi.org/10.1016/j.jcrs.2012.05.030
Tay E, Li X, Gimbel HV, Kaye G (2013) Assessment of axial length before and after myopic LASIK with the IOLMaster. J Refract Surg 29:838–841. https://doi.org/10.3928/1081597X-20130924-01
Reinstein DZ, Archer TJ, Gobbe M (2010) Corneal ablation depth readout of the MEL 80 excimer laser compared to Artemis three-dimensional very high-frequency digital ultrasound stromal measurements. J Refract Surg 26:949–959. https://doi.org/10.3928/1081597X-20100114-02
Reinstein DZ, Archer TJ, Gobbe M (2014) Lenticule thickness readout for small incision lenticule extraction compared to Artemis three-dimensional very high-frequency digital ultrasound stromal measurements. J Refract Surg 30:304–309. https://doi.org/10.3928/1081597X-20140416-01
Luft N, Priglinger SG, Ring MH et al (2017) Stromal remodeling and lenticule thickness accuracy in small-incision lenticule extraction: one-year results. J Cataract Refract Surg 43:812–818. https://doi.org/10.1016/j.jcrs.2017.03.038
Zhou J, Zhang Y, Li M, Sun L, Zhou X (2018) Predictability of the achieved lenticule thickness in small incision lenticule extraction for myopia correction. Eye Contact Lens 44(Suppl 2):S410–S413
Kielhorn I, Rajan MS, Tesha PM, Subryan VR, Bell JA (2003) Clinical assessment of the Zeiss IOLMaster. J Cataract Refract Surg 29:518–522. https://doi.org/10.1016/S0886-3350(02)01819-9
Findl O, Drexler W, Menapace R, Hitzenberger CK, Fercher AF (1998) High precision biometry of pseudophakic eyes using partial coherence interferometry. J Cataract Refract Surg 24:1087–1093
Hussin HM, Spry PG, Majid MA, Gouws P (2006) Reliability and validity of the partial coherence interferometry for measurement of ocular axial length in children. Eye 20:1021–1024. https://doi.org/10.1038/sj.eye.6702069
Bailey MD, Twa MD, Mitchell GL, Dhaliwal DK, Jones LA, McMahon TT (2005) Repeatability of autorefraction and axial length measurements after laser in situ keratomileusis. J Cataract Refract Surg 31:1025–1034. https://doi.org/10.1016/j.jcrs.2004.12.040
Vestergaard AH, Grauslund J, Ivarsen AR, Hjortdal JO (2014) Central corneal sublayer pachymetry and biomechanical properties after refractive femtosecond lenticule extraction. J Refract Surg 30:102–108. https://doi.org/10.3928/1081597X-20140120-05
Luft N, Ring MH, Dirisamer M, Mursch-Edlmayr AS, Kreutzer TC, Pretzl J, Bolz M, Priglinger SG (2016) Corneal epithelial remodeling induced by small incision lenticule extraction (SMILE). Invest Ophthalmol Vis Sci 57:OCT176–OCT183. https://doi.org/10.1167/iovs.15-18879
Mukaka MM (2012) Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J 24:69–71
Vestergaard A, Ivarsen AR, Asp S, Hjortdal JØ (2012) Small-incision lenticule extraction for moderate to high myopia: predictability, safety, and patient satisfaction. J Cataract Refract Surg 38:2003–2010. https://doi.org/10.1016/j.jcrs.2012.07.021
Vestergaard A, Ivarsen A, Asp S, Hjortdal JØ (2013) Femtosecond (FS) laser vision correction procedure for moderate to high myopia: a prospective study of ReLEx(®) flex and comparison with a retrospective study of FS-laser in situ keratomileusis. Acta Ophthalmol 91:355–362. https://doi.org/10.1111/j.1755-3768.2012.02406.x
Shah R, Shah S (2011) Effect of scanning patterns on the results of femtosecond laser lenticule extraction refractive surgery. J Cataract Refract Surg 37:1636–1647. https://doi.org/10.1016/j.jcrs.2011.03.056
Donate D, Thaëron R (2016) Lower energy levels improve visual recovery in small incision lenticule extraction (SMILE). J Refract Surg 32:636–642. https://doi.org/10.3928/1081597X-20160602-01
Shetty R, Shroff R, Kaweri L, Jayadev C, Kummelil MK, Sinha Roy A (2016) Intra-operative cap repositioning in small incision lenticule extraction (SMILE) for enhanced visual recovery. Curr Eye Res 41:1532–1538. https://doi.org/10.3109/02713683.2016.1168848
Agca A, Ozgurhan EB, Yildirim Y, Cankaya KI, Guleryuz NB, Alkin Z, Ozkaya A, Demirok A, Yilmaz OF (2014) Corneal backscatter analysis by in vivo confocal microscopy: fellow eye comparison of small incision lenticule extraction and femtosecond laser-assisted LASIK. J Ophthalmol 2014:265012. https://doi.org/10.1155/2014/265012
Uçakhan OO, Ozkan M, Kanpolat A (2006) Corneal thickness measurements in normal and keratoconic eyes: Pentacam comprehensive eye scanner versus noncontact specular microscopy and ultrasound pachymetry. J Cataract Refract Surg 32:970–977. https://doi.org/10.1016/j.jcrs.2006.02.037
Lee JH, Kim JH, Kim SW (2018) Repeatability of central corneal thickness measurement using rotating Scheimpflug camera in dry and normal eyes. Eye Contact Lens 44(Suppl 2):S29–S32. https://doi.org/10.1097/ICL.0000000000000373
Rozema JJ, Wouters K, Mathysen DG, Tassignon MJ (2014) Overview of the repeatability, reproducibility, and agreement of the biometry values provided by various ophthalmic devices. Am J Ophthalmol 158:1111–1120. https://doi.org/10.1016/j.ajo.2014.08.014
Reinstein DZ, Yap TE, Archer TJ, Gobbe M, Silverman RH (2015) Comparison of corneal epithelial thickness measurement between Fourier-domain OCT and very high-frequency digital ultrasound. J Refract Surg 31:438–445. https://doi.org/10.3928/1081597X-20150623-01
Ursea R, Feng M, Urs R, RoyChoudhury A, Silverman RH (2013) Comparison of Artemis 2 ultrasound and Visante optical coherence tomography corneal thickness profiles. J Refract Surg 29:36–41. https://doi.org/10.3928/1081597X-20121126-01
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the local institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights and informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 218 kb)
Rights and permissions
About this article
Cite this article
Tay, E., Bajpai, R. Small incision lenticule extraction (SMILE) lenticule thickness readout compared to change in axial length measurements with the IOLMaster. Graefes Arch Clin Exp Ophthalmol 258, 917–924 (2020). https://doi.org/10.1007/s00417-019-04529-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04529-2