Abstract
Background
While patients with frequently relapsing nephrotic syndrome (FRNS) are initially treated with long-term alternate-day prednisolone, relapses and adverse effects are common. In an open-label randomized controlled trial, we compared the efficacy of therapy with low-dose daily to standard alternate-day prednisolone in reducing relapse rates over 12-month follow-up.
Methods
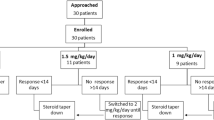
Consecutive patients, aged 2–18 years, with FRNS were included. Following therapy of relapse, prednisolone was tapered to 0.75 mg/kg on alternate days. Stratifying for steroid dependence, patients were randomly assigned to prednisolone at 0.2–0.3 mg/kg daily or 0.5–0.7 mg/kg alternate day for 12 months. Relapses were treated with daily prednisolone, followed by return to intervention. Primary outcome was the incidence of relapses. Proportion with therapy failure (≥ 2 relapses in any 6 months or significant steroid toxicity) and sustained remission, cumulative prednisolone intake and adverse events were evaluated.
Results
Patients receiving daily prednisolone (n = 30) showed significantly fewer relapses than those on alternate-day therapy (n = 31) (0.55 relapses/person-year versus 1.94 relapses/person-year; incidence rate ratio 0.28; 95% CI 0.15, 0.52). Daily therapy was associated with higher rates of sustained remission at 6 months (73.3 versus 48.4%) and 1 year (60 versus 31.6%; log rank p = 0.013), lower rates of treatment failure at 6 months (3.3 versus 32.8%) and 1 year (6.7 versus 57.4%; p < 0.0001), and lower prednisolone use (0.27 ± 0.07 versus 0.39 ± 0.19 mg/kg/day; p = 0.003). Three and two patients need to receive the study intervention to enable sustained remission and prevent treatment failure, respectively.
Conclusions
In patients with FRNS, daily administration of low-dose prednisolone is more effective than standard-dose alternate day therapy in lowering relapse rates, sustaining remission, and enabling steroid sparing.


Similar content being viewed by others
References
International Study of Kidney Disease in Children (1979) Nephrotic syndrome in children: a randomized trial comparing two prednisone regimens in steroid-responsive patients who relapse early. Report of the international study of kidney disease in children. J Pediatr 95:239–243
Emma F, Sesto A, Rizzoni G (2003) Long-term linear growth of children with severe steroid-responsive nephrotic syndrome. Pediatr Nephrol 18:783–788
Kyrieleis HA, Lowik MM, Pronk I, Cruysberg HR, Kremer JA, Oyen WJ, van den Heuvel BL, Wetzels JF, Levtchenko EN (2009) Long-term outcome of biopsy-proven, frequently relapsing minimal-change nephrotic syndrome in children. Clin J Am Soc Nephrol 4:1593–1600
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group (2012) Steroid-sensitive nephrotic syndrome in children. Kidney Int Suppl 2(2011):163–171
Indian Pediatric Nephrology Group, Indian Academy of Pediatrics, Bagga A, Ali U, Banerjee S, Kanitkar M, Phadke KD, Senguttuvan P, Sethi S, Shah M (2008) Management of steroid sensitive nephrotic syndrome: revised guidelines. Indian Pediatr 45:203–214
Consensus statement on management and audit potential for steroid responsive nephrotic syndrome (1994) Workshop by the British Association for Paediatric Nephrology and Research Unit, Royal College of Physicians. Arch Dis Child 70:151–157
Hahn D, Hodson EM, Willis NS, Craig JC (2015) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev: CD001533
Sinha A, Hari P, Sharma PK, Gulati A, Kalaivani M, Mantan M, Dinda AK, Srivastava RN, Bagga A (2012) Disease course in steroid sensitive nephrotic syndrome. Indian Pediatr 49:881–887
Uwaezuoke SN (2015) Steroid-sensitive nephrotic syndrome in children: triggers of relapse and evolving hypotheses on pathogenesis. Ital J Pediatr 41:19
Gulati A, Sinha A, Sreenivas V, Math A, Hari P, Bagga A (2011) Daily corticosteroids reduce infection-associated relapses in frequently relapsing nephrotic syndrome: a randomized controlled trial. Clin J Am Soc Nephrol 6:63–69
Abeyagunawardena AS, Trompeter RS (2008) Increasing the dose of prednisolone during viral infections reduces the risk of relapse in nephrotic syndrome: a randomised controlled trial. Arch Dis Child 93:226–228
Mattoo TK, Mahmoud MA (2000) Increased maintenance corticosteroids during upper respiratory infection decrease the risk of relapse in nephrotic syndrome. Nephron 85:343–345
Leisti S, Hallman N, Koskimies O, Perheentupa J, Rapola J, Vilska J (1977) Association of postmedication hypocortisolism with early first relapse of idiopathic nephrotic syndrome. Lancet 2:795–796
Leisti S, Koskimies O (1983) Risk of relapse in steroid-sensitive nephrotic syndrome: effect of stage of post-prednisone adrenocortical suppression. J Pediatr 103:553–557
Leisti S, Vilska J, Hallman N (1977) Adrenocortical insufficiency and relapsing in the idiopathic nephrotic syndrome of childhood. Pediatrics 60:334–342
Leisti S, Koskimies O, Perheentupa J, Vilska J, Hallman N (1978) Idiopathic nephrotic syndrome: prevention of early relapse. Br Med J 1:892
Srivastava RN, Vasudev AS, Bagga A, Sunderam KR (1992) Long-term, low-dose prednisolone therapy in frequently relapsing nephrotic syndrome. Pediatr Nephrol 6:247–250
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85:660–667
Schoeneman MJ (1983) Minimal change nephrotic syndrome: treatment with low doses of hydrocortisone. J Pediatr 102:791–793
Wingen AM, Muller-Wiefel DE, Scharer K (1990) Comparison of different regimens of prednisone therapy in frequently relapsing nephrotic syndrome. Acta Paediatr Scand 79:305–310
Elzouki AY, Jaiswal OP (1988) Long-term, small dose prednisone therapy in frequently relapsing nephrotic syndrome of childhood. Effect on remission, statural growth, obesity, and infection rate. Clin Pediatr (Phila) 27:387–392
Arbeitsgemeinschaft fur Padiatrische Nephrologie (1981) Alternate day prednisone is more effective than intermittent prednisone in frequently relapsing nephrotic syndrome. Eur J Pediatr 135:229–237
Moel DI, Kwun YA, Teitcher J (1980) Hypothalamic-pituitary-adrenal function in adrenocortical steroid treated minimal change nephrotic syndrome. Clin Nephrol 14:36–41
Abeyagunawardena AS, Hindmarsh P, Trompeter RS (2007) Adrenocortical suppression increases the risk of relapse in nephrotic syndrome. Arch Dis Child 92:585–588
Ribeiro D, Zawadynski S, Pittet LF, Chevalley T, Girardin E, Parvex P (2015) Effect of glucocorticoids on growth and bone mineral density in children with nephrotic syndrome. Eur J Pediatr 174:911–917
Acknowledgments
Dr. M. Jeeva Sankar is acknowledged for the advice with statistical analysis.
Funding
Support for research on nephrotic syndrome has been possible through funding by the Indian Council of Medical Research (No. 5/7/1090/2013-RHN).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval was by the Institute Ethics Committee and informed written consent was obtained from either parent or patient before enrollment.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Yadav, M., Sinha, A., Khandelwal, P. et al. Efficacy of low-dose daily versus alternate-day prednisolone in frequently relapsing nephrotic syndrome: an open-label randomized controlled trial. Pediatr Nephrol 34, 829–835 (2019). https://doi.org/10.1007/s00467-018-4071-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-4071-7