Abstract
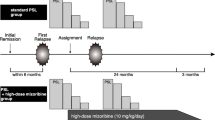
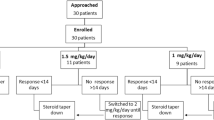
The use of steroids in idiopathic nephrotic syndrome is the major discovery of the twentieth century in the field of pediatric nephrology. At onset of the twenty-first century, steroids remain the first line of treatment at first flare. All the protocols to treat the first flare are similar by a common sequence including a first phase of daily prednisolone/prednisone at a dose of 60 mg/m2/day for at least 4 weeks followed by an alternate-day regimen for several weeks. It appears that a cumulated dose of 2240 mg/m2 given in 8 weeks at the first flare without tapering sequence is not inferior to increased dose and duration in terms of prevalence of frequent relapsers and the subsequent cumulated dose of steroids at 24 months of follow-up. A higher cumulated dose might only be interesting in patients aged below 4 years although a formal demonstration is still missing. Several retrospective studies are concordant to suggest that intravenous methylprednisolone pulses are useful to reach a full urinary remission in case of oral resistance to 4 weeks of oral prednisone/prednisolone. A majority of patients have multiple relapses after the treatment of the first flare and half meet the definition of steroid dependency. In those patients, long-lasting alternate-day prednisone/prednisolone therapy does not lead to long-lasting remission, opening the question of the best strategy of immunosuppression.

Similar content being viewed by others
References
Riley CM (1950) The effect of adrenocorticotrophic hormone on salt and water excretion in children with the nephrotic syndrome. Am J Dis Child 80:520–521
Barnett HL, Mc NH, Mc CW, Forman C, Rapoport M, Michie A, Barbero G (1950) The effects of ACTH and cortisone on the nephrotic syndrome. Am J Dis Child 80:519–520
Luetscher JA Jr, Deming QB (1950) Treatment of nephrosis with cortisone. J Clin Invest 29:1576–1587
Drummond KN, Michael AF, Good RA, Vernier RL (1966) The nephrotic syndrome of childhood: immunologic, clinical, and pathologic correlations. J Clin Invest 45:620–360
Deschenes G, Vivarelli M, Peruzzi L (2017) Variability of diagnostic criteria and treatment of idiopathic nephrotic syndrome across European countries. Eur J Pediatr 176:647–654
KDIGO (2012) KDIGO Clinical Practice Guideline for Glomerulonephritis. Kidney Int 2:139–274
Spencer RL, Chun LE, Hartsock MJ, Woodruff ER (2017) Glucocorticoid hormones are both a major circadian signal and major stress signal: How this shared signal contributes to a dynamic relationship between the circadian and stress systems. Front Neuroendocrinol S0091-3022(17)30103–30106. https://doi.org/10.1016/j.yfrne
Vacchio MS, Ashwell JD (1997) Thymus-derived glucocorticoids regulate antigen-specific positive selection. J Exp Med 185:2033–2038
Purton JF, Monk JA, Liddicoat DR, Kyparissoudis K, Sakkal S, Richardson SJ, Godfrey DI, Cole TJ (2004) Expression of the glucocorticoid receptor from the 1A promoter correlates with T lymphocyte sensitivity to glucocorticoid-induced cell death. J Immunol 173:3816–3824
Andreau K, Lemaire C, Souvannavong V, Adam A (1998) Induction of apoptosis by dexamethasone in the B cell lineage. Immunopharmacology 40:67–76
Cain DW, Cidlowski JA (2017) Immune regulation by glucocorticoids. Nat Rev Immunol 17:233–247
Zen M, Canova M, Campana C, Bettio S, Nalotto L, Rampudda M, Ramonda R, Iaccarino L, Doria A (2011) The kaleidoscope of glucorticoid effects on immune system. Autoimmun Rev 10:305–310
Pasini A, Aceto G, Ammenti A, Ardissino G, Azzolina V, Bettinelli A, Cama E, Cantatore S, Crisafi A, Conti G, D’Agostino M, Dozza A, Edefonti A, Fede C, Groppali E, Gualeni C, Lavacchini A, Lepore M, Maringhini S, Mariotti P, Materassi M, Mencarelli F, Messina G, Negri A, Piepoli M, Ravaglia F, Simoni S, Spagnoletta L, Montini G, (2015) Best practice guidelines for idiopathic nephrotic syndrome: recommendations versus reality. Pediatr Nephrol 30:91–101
Sinha A, Saha A, Kumar M, Sharma S, Afzal K, Mehta A, Kalaivani M, Hari P, Bagga A (2015) Extending initial prednisolone treatment in a randomized control trial from 3 to 6 months did not significantly influence the course of illness in children with steroid-sensitive nephrotic syndrome. Kidney Int 87:217–224
Teeninga N, Kist-van Holthe JE, van Rijswijk N, de Mos NI, Hop WC, Wetzels JF, van der Heijden AJ, Nauta J (2013) Extending prednisolone treatment does not reduce relapses in childhood nephrotic syndrome. J Am Soc Nephrol 24:149–519
Yoshikawa N, Nakanishi K, Sako M, Oba MS, Mori R, Ota E, Ishikura K, Hataya H, Honda M, Ito S, Shima Y, Kaito H, Nozu K, Nakamura H, Igarashi T, Ohashi Y, Iijima K (2015) A multicenter randomized trial indicates initial prednisolone treatment for childhood nephrotic syndrome for two months is not inferior to six-month treatment. Kidney Int 87:225–232
Webb N, Wooley R, Bretell E, Cummins C, Trompeter R, Barsoum E, Ives N, investigators P (2017) Standard vs. extended course prednisolone therapy for the presenting episode of steroid sensitive nephrotic syndrome: the PREDNOS study. Pediatr Nephrol 32:1647–1648
Teeninga N, Guan Z, Stevens J, Kist-van Holthe JE, Ackermans MT, van der Heijden AJ, van Schaik RH, van Gelder T, Nauta J (2016) Population pharmacokinetics of prednisolone in relation to clinical outcome in children with nephrotic syndrome. Ther Drug Monit 38:534–545
Ekka BK, Bagga A, Srivastava RN (1997) Single- versus divided-dose prednisolone therapy for relapses of nephrotic syndrome. Pediatr Nephrol 11:597–599
Hahn D, Hodson EM, Willis NS, Craig JC (2015) Corticosteroid therapy for nephrotic syndrome in children. Cochrane Database Syst Rev, Issue3, Art N° CD001533, 1–130. https://doi.org/10.1002/14651858.CD001533.pub5
Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS (1985) Long-term outcome for children with minimal-change nephrotic syndrome. Lancet 1:368–370
Hiraoka M, Tsukahara H, Matsubara K, Tsurusawa M, Takeda N, Haruki S, Hayashi S, Ohta K, Momoi T, Ohshima Y, Suganuma N, Mayumi M (2003) A randomized study of two long-course prednisolone regimens for nephrotic syndrome in children. Am J Kidney Dis 41:1155–1562
Hoyer PF, Brodeh J (2006) Initial treatment of idiopathic nephrotic syndrome in children: prednisone versus prednisone plus cyclosporine A: a prospective, randomized trial. J Am Soc Nephrol 17:1151–1157
Schijvens AM, Dorresteijn EM, Roeleveld N, Ter Heine R, van Wijk JAE, Bouts AHM, Keijzer-Veen MG, van de Kar N, van den Heuvel L, Schreuder MF (2017) REducing STEroids in relapsing nephrotic syndrome: the RESTERN study—protocol of a national, double-blind, randomised, placebo-controlled, non-inferiority intervention study. BMJ Open 7:e018148
APN (1982) Effect of cytotoxic drugs in frequently relapsing nephrotic syndrome with and without steroid dependence. N Engl J Med 306:451–454
Vivarelli M, Massella L, Ruggiero B, Emma F (2017) Minimal change disease. Clin J Am Soc Nephrol 12:332–345
Broyer M, Kleinknecht C (1978) Traitement des néphroses corticosensibles par la corticothérapie discontinue prolongée. In: Mathieu H (ed) Journée Parisienne de Pédiatrie. Flammarion Médecine Science, Paris, pp 158–710
Srivastava RN, Vasudev AS, Bagga A, Sunderam KR (1992) Long-term, low-dose prednisolone therapy in frequently relapsing nephrotic syndrome. Pediatr Nephrol 6:247–250
Gulati A, Sinha A, Sreenivas V, Math A, Hari P, Bagga A (2011) Daily corticosteroids reduce infection-associated relapses in frequently relapsing nephrotic syndrome: a randomized controlled trial. Clin J Am Soc Nephrol 6:63–69
Abeyagunawardena AS, Trompeter RS (2008) Increasing the dose of prednisolone during viral infections reduces the risk of relapse in nephrotic syndrome: a randomised controlled trial. Arch Dis Child 93:226–228
Abeyagunawardena AS, Thalgahagoda RS, Dissanayake PV, Abeyagunawardena S, Illangasekera YA, Karunadasa UI, Trompeter RS (2017) Short courses of daily prednisolone during upper respiratory tract infections reduce relapse frequency in childhood nephrotic syndrome. Pediatr Nephrol 32:1377–1382
Broyer M, Terzi F, Lehnert A, Gagnadoux MF, Guest G, Niaudet P (1997) A controlled study of deflazacort in the treatment of idiopathic nephrotic syndrome. Pediatr Nephrol 11:418–422
Singhal R, Pandit S, Dhawan N (2015) Deflazacort versus prednisolone: randomized controlled trial in treatment of children with idiopathic nephrotic syndrome. Iran J Pediatr 25:e510
Gennari C, Imbimbo B, Montagnani M, Bernini M, Nardi P, Avioli LV (1984) Effects of prednisone and deflazacort on mineral metabolism and parathyroid hormone activity in humans. Calcif Tissue Int 36:245–252
Foster BJ, Shults J, Zemel BS, Leonard MB (2006) Risk factors for glucocorticoid-induced obesity in children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 21:973–980
Leroy V, Baudouin V, Alberti C, Guest G, Niaudet P, Loirat C, Deschenes G, Czernichow P, Simon D (2009) Growth in boys with idiopathic nephrotic syndrome on long-term cyclosporin and steroid treatment. Pediatr Nephrol 24:2393–2400
Motoyama O, Iitaka K (2007) Final height in children with steroid-sensitive nephrotic syndrome. Pediatr Int 49:623–625
Simmonds J, Grundy N, Trompeter R, Tullus K (2010) Long-term steroid treatment and growth: a study in steroid-dependent nephrotic syndrome. Arch Dis Child 95:146–149
Kaye LD, Kalenak JW, Price RL, Cunningham R (1993) Ocular implications of long-term prednisone therapy in children. J Pediatr Ophthalmol Strabismus 30:142–144
Gulati S, Gulati K (2005) Bone disease in nephrotic syndrome—prevention is better than cure. Pediatr Nephrol 20:111–112
Ksiazek J, Niemirska A, Lipka M, Grenda R (2006) Evaluation of arterial intima-media thickness (IMT) in children with idiopathic nephrotic syndrome—preliminary report. Przegl Lek 63(Suppl 3):205–207
Zajaczkowska M, Papierkowski A, Szczepanowska A, Zinkiewicz Z, Borzecka H, Zbaranska S (2001) Influence of glucocorticoid steroid therapy on gastric and duodenal mucosa and helicobacter pylori infection in children with nephrotic syndrome. Pol Merkur Lekarski 10:165–167
Upadhyay A, Mishra OP, Prasad R, Upadhyay SK, Schaefer F (2016) Behavioural abnormalities in children with new-onset nephrotic syndrome receiving corticosteroid therapy: results of a prospective longitudinal study. Pediatr Nephrol 31:233–238
Ulinski T, Carlier-Legris A, Schlecht D, Ranchin B, Cochat P (2005) Triamcinolone acetonide: a new management of noncompliance in nephrotic children. Pediatr Nephrol 20:759–762
Dehoux L, Hogan J, Dossier C, Fila M, Niel O, Maisin A, Macher MA, Kwon T, Baudouin V, Deschênes G (2016) Mycophenolate mofetil in steroid-dependent idiopathic nephrotic syndrome. Pediatr Nephrol 31:2095–2101
Gruppen MP, Bouts AH, Jansen-van der Weide MC, Merkus MP, Zurowska A, Maternik M, Massella L, Emma F, Niaudet P, Cornelissen EAM, Schurmans T, Raes A, van de Walle J, van Dyck M, Gulati A, Bagga A, Davin JC (2018) A randomized clinical trial indicates that levamisole increases the time to relapse in children with steroid-sensitive idiopathic nephrotic syndrome. Kidney Int 93:510–518
Kuzma-Mroczkowska E, Skrzypczyk P, Panczyk-Tomaszewska M (2016) Levamisole therapy in children with frequently relapsing and steroid-dependent nephrotic syndrome: a single-center experience. Cent Eur J Immunol 41:243–247
Baudouin V, Alberti C, Lapeyraque AL, Bensman A, Andre JL, Broux F, Cailliez M, Decramer S, Niaudet P, Deschenes G, Jacqz-Aigrain E, Loirat C (2012) Mycophenolate mofetil for steroid-dependent nephrotic syndrome: a phase II Bayesian trial. Pediatr Nephrol 27:389–396
Mahmoud I, Basuni F, Sabry A, El-Husseini A, Hassan N, Ahmad NS, Elbaz M, Moustafa F, Sobh M (2005) Single-centre experience with cyclosporin in 106 children with idiopathic focal segmental glomerulosclerosis. Nephrol Dial Transplant 20:735–472
Kengne-Wafo S, Massella L, Diomedi-Camassei F, Gianviti A, Vivarelli M, Greco M, Stringini GR, Emma F (2009) Risk factors for cyclosporin a nephrotoxicity in children with steroid-dependant nephrotic syndrome. Clin J Am Soc Nephrol 4:1409–1416
Azib S, Macher MA, Kwon T, Dechartres A, Alberti C, Loirat C, Deschenes G, Baudouin V (2011) Cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26:927–932
Zagury A, de Oliveira AL, de Moraes CA, de Araujo Montalvao JA, Novaes RH, de Sa VM, Monteiro de Carvalho DB, Matuck T (2011) Long-term follow-up after cyclophosphamide therapy in steroid-dependent nephrotic syndrome. Pediatr Nephrol 26:915–920
Kamei K, Ishikura K, Sako M, Aya K, Tanaka R, Nozu K, Kaito H, Nakanishi K, Ohtomo Y, Miura K, Takahashi S, Morimoto T, Kubota W, Ito S, Nakamura H, Iijima K (2017) Long-term outcome of childhood-onset complicated nephrotic syndrome after a multicenter, double-blind, randomized, placebo-controlled trial of rituximab. Pediatr Nephrol 32:2071–2078
Sellier-Leclerc AL, Baudouin V, Kwon T, Macher MA, Guerin V, Lapillonne H, Deschenes G, Ulinski T (2012) Rituximab in steroid-dependent idiopathic nephrotic syndrome in childhood—follow-up after CD19 recovery. Nephrol Dial Transplant 27:1083–1089
Hari P, Bagga A, Mantan M (2004) Short term efficacy of intravenous dexamethasone and methylprednisolone therapy in steroid resistant nephrotic syndrome. Indian Pediatr 41:993–1000
Shenoy M, Plant ND, Lewis MA, Bradbury MG, Lennon R, Webb NJ (2010) Intravenous methylprednisolone in idiopathic childhood nephrotic syndrome. Pediatr Nephrol 25:899–903
Zhang H, Wang Z, Dong LQ, Guo YN (2016) Children with steroid-resistant nephrotic syndrome: long-term outcomes of sequential steroid therapy. Biomed Environ Sci 29:650–655
Ehrich JH, Geerlings C, Zivicnjak M, Franke D, Geerlings H, Gellermann J (2007) Steroid-resistant idiopathic childhood nephrosis: overdiagnosed and undertreated. Nephrol Dial Transplant 22:2183–2193
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Georges Deschênes declares that he has no conflict of interest in the field of the paper. Claire Dossier and Julien Hogan received a grant from Délégation de la Recherche Clinique for randomized control trials in patients with Idiopathic Nephrotic Syndrome (PHRCI-15-015 and PHRCN-16-0547, respectively).
Additional information
Answers
1. b; 2. c; 3. b, c, d, e; 4. a, d; 5. d
Rights and permissions
About this article
Cite this article
Deschênes, G., Dossier, C. & Hogan, J. Treating the idiopathic nephrotic syndrome: are steroids the answer?. Pediatr Nephrol 34, 777–785 (2019). https://doi.org/10.1007/s00467-018-3963-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-3963-x