Abstract
Introduction
The validated Knee Osteoarthritis Grading System (KOGS) was implemented and clinical results were compared with patient satisfaction data and implant survivorship in a multi-centre study with surgeons familiar with unicompartmental knee arthroplasty (UKA), patellofemoral arthroplasty (PFA) and total knee arthroplasty (TKA).
This is also the first study to evaluate the prevalence of UKA and TKA in consecutive osteoarthritis (OA) knee arthroplasties assessed by this system..
Method
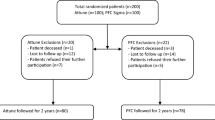
A consecutive cohort of knees was gathered at three different institutions as categorized by KOGS and surgically treated with the recommended implant unless clinical reasons or patient preference precluded such an option.
One thousand one hundred seventy-seven consecutive knees were evaluated including 311 TKA (26%), 695 medial UKA (59%), 154 lateral UKA (13%) and 17 PFA (2%) and the results of the categories evaluated with the Oxford Knee Score (OKS) and the complications reflected in the different categories.
Results
The failure rate of the UKA (3.5%) or TKA (1.6%) is not higher than accepted results in the literature and the difference in complications is negligible between the UKA (72%) and TKA (26%) cohorts.
Revision of a UKA to a TKA as an endpoint was 0.58% with ipsilateral progression at 0.8% over a period of five to 84 months (mean follow-up of 36 months) despite the ‘excessive’ proportion of UKA in this cohort.
The Oxford Score improvement is significant in TKA and UKA and contributes to the acceptable outcomes (The OKS for TKA improved from 20 pre-operatively to 36 post-operatively and the UKA improved from 22 pre-operatively to 39 post-operatively).
Conclusion
KOGS achieves acceptable early survival and functional results when implemented and is a suitable tool for identifying the preferred implant as was validated.



Similar content being viewed by others
References
Kazarian GS, Lonner JH, Maltenfort MG et al (2018) Cost-effectiveness of surgical and nonsurgical treatments for unicompartmental knee arthritis: a Markov model. J Bone Joint Surg Am 100:1653–1660
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Murray DW, Parkinson RW (2018) Usage of unicompartmental knee arthroplasty. Bone Joint J 100-B:432–435
Adelani MA, Mall NA, Brophy RH et al (2016) The use of MRI in evaluating knee pain in patients aged 40 years and older. J Am Acad Orthop Surg 24:653–659
Ritter MA, Keating EM, Sueyoshi T et al (2016) Twenty-five-years and greater, results after nonmodular cemented total knee arthroplasty. J Arthroplast 31:2199–2202
Escobar A, Quintana JM, Aróstegui I et al (2003) Development of explicit criteria for total knee replacement. Int J Technol Assess Health Care 19:57–70
Riddle DL, Perera RA, Jiranek WA, Dumenci L (2015) Using surgical appropriateness criteria to examine outcomes of total knee arthroplasty in a United States sample. Arthritis Care Res (Hoboken) 67:349–357
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445
D’Amato M, Ensini A, Leardini A et al (2018) Conventional versus computer-assisted surgery in total knee arthroplasty: comparison at ten years follow-up. Int Orthop 43:1355–1363
Wylde V, Beswick A, Bruce J et al (2018) Chronic pain after total knee arthroplasty. EFORT Open Rev 3:461–470
Migliorini F, Tingart M, Niewiera M et al (2019) Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur J Orthop Surg Traumatol 29:947–955
Lons A, Putman S, Pasquier G et al (2017) Metallic ion release after knee prosthesis implantation: a prospective study. Int Orthop 41:2503–2508
Peersman G, Verhaegen J, Favier B (2019) The forgotten joint score in total and unicompartmental knee arthroplasty: a prospective cohort study. Int Orthop (Online). https://doi.org/10.1007/s00264-019-04342-w
Pandit H, Hamilton TW, Jenkins C et al (2015) The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J 97-B:1493–1500
Willis-Owen CA, Brust K, Alsop H et al (2009) Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee 16:473–478
National Joint Registry for England, Wales, Northern Ireland and the Isle of Man 15th Annual Report (2018). In: http://www.njrreports.org.uk/Portals/0/PDFdownloads/NJR%2015th%20Annual%20Report%202018.pdf. Accessed 11 Mar 2019
Goodfellow JW, O’Connor JJ, Murray DW (2010) A critique of revision rate as an outcome measure: re-interpretation of knee joint registry data. J Bone Joint Surg Br 92-B:1628–1631
Rodríguez-Merchán CE, Gómez-Cardero P (2018) Unicompartmental knee arthroplasty: current indications, technical issues and results. EFORT Open Rev 3:363–373
Cho WJ, Kim JM, Kim WK et al (2018) Mobile-bearing unicompartmental knee arthroplasty in old-aged patients demonstrates superior short-term clinical outcomes to open-wedge high tibial osteotomy in middle-aged patients with advanced isolated medial osteoarthritis. Int Orthop 42:2357–2363
Kim MS, Koh IJ, Sohn S et al (2019) Unicompartmental knee arthroplasty is superior to high tibial osteotomy in post-operative recovery and participation in recreational and sport activities. Int Orthop (Online). https://doi.org/10.1007/s00264-018-4272-5
Saragaglia D, Bevand A, Refaie R et al (2018) Results with nine years mean follow up on one hundred and three KAPS® uni knee arthroplasties: eighty six medial and seventeen lateral. Int Orthop 42:1061–1066
Oosthuizen CR, Takahashi T, Rogan M et al (2019) The knee osteoarthritis grading system for arthroplasty. J Arthroplast 34:450–455
Liebensteiner M, Wurm A, Gamper D et al (2019) Patient satisfaction after total knee arthroplasty is better in patients with pre-operative complete joint space collapse. Int Orthop 43:1841–1847
Oosthuizen C, Burger S, Vermaak D et al (2015) The X-ray knee instability and degenerative score (X-KIDS) to determine the preference for a partial or a total knee arthroplasty (PKA/TKA). South African Orthop J 14:61–69
Hamilton TW, Pandit HG, Lombardi AV et al (2016) Radiological decision aid to determine suitability for medial unicompartmental knee arthroplasty: development and preliminary validation. Bone Joint J 98-B:3–10
Beard DJ, Pandit H, Gill HS et al (2007) The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg Br 89-B:1597–1601
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14 076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 97-B:793–801
Zha GC, Feng S, Chen XY, Guo KJ (2018) Does the grading of chondromalacia patellae influence anterior knee pain following total knee arthroplasty without patellar resurfacing? Int Orthop 42:513–518
Pisanu G, Rosso F, Bertolo C et al (2017) Patellofemoral arthroplasty: current concepts and review of the literature. Joints 05:237–245
Knifsund J, Hatakka J, Keemu H et al (2017) Unicompartmental knee arthroplasties are performed on the patients with radiologically too mild osteoarthritis. Scand J Surg 106:338–341
Tecame A, Savica R, Rosa MA, Adravanti P (2019) Anterior cruciate ligament reconstruction in association with medial unicompartmental knee replacement: a retrospective study comparing clinical and radiological outcomes of two different implant design. Int Ortop (Online). https://doi.org/10.1007/s00264-019-04341-x
Wilson HA, Middleton R, Abram SGF et al (2019) Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ 364:l352
Liddle AD, Pandit H, Judge A, Murray DW (2016) Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Joint Surg Am 98:1–8
Ernstbrunner L, Imam MA, Andronic O et al (2018) Lateral unicompartmental knee replacement: a systematic review of reasons for failure. Int Orthop 42:1827–1833
Acknowledgements
The authors would like to thank Margaret Houman (Research Manager) and Andricha Viljoen (Researcher).
Author declarations
We, the authors declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere.
We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. All authors have participated in the research. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
We understand that the Corresponding Author, CR Oosthuizen, is the sole contact for the Editorial process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they received no research grants from funding agencies for this research.
Author 1 is an ad hoc paid consultant for Zimmer Biomet and Amplitude. Author 2 has received a speaker honorarium for a presentation on general aspects of Research and Innovation from Smith & Nephew.
No other interests required declaration as no benefits in any form have been received from a commercial party related directly or indirectly to the subject of this article.
Ethical approval
Ethical approval was obtained from the Human Research Ethics Committee at the University of the Witwatersrand (WITS) to study the data and X-rays of the individual orthopaedic practices with Clearance Certificate Nos. M1704111 and M1704112. All procedures performed in studies involving human participants were in accordance with the ethical standards of the above named institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Copyright and license term
The appendix containing the synopsis of KOGS and the KOGS flowchart with radiographs was published as an open access article under the Creative Commons Attribution License CC BY-NC-ND. [Oosthuizen CR, Takahashi T, Rogan M, et al. (2019) The Knee Osteoarthritis Grading System for Arthroplasty. J Arthroplasty 34:450–455. https://doi.org/10.1016/j.arth.2018.11.011], which permits unrestricted use, distribution and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. Synopsis of KOGS [22]
Appendix. Synopsis of KOGS [22]
The grading system consists of four grades with treatment options to be implemented. Despite the specific grading achieved, there are clinical reasons which can influence the final decision for a particular prosthesis e.g. rheumatoid arthritis, clinically assessed disruption of ligaments, excessive deformities or patient-specific considerations or preferences. KOGS cannot be the only deciding factor.
Grade 1
Single TF or PF joint OA
Degeneration affects any one of the three compartments, with K&L grade 4 degeneration.
Grade 2
Single TF OA and ‘pseudolaxity’
AP view subluxation, isolated K&L grade 4 wear defects cause AP translation without ligament instability (stress X-ray restoration of JLCA < 2°).
On average, above this line would be UKA and below TKA
Grade 3
A: Single TF OA with K&L grade 4 and concomitant ACL instability with sagittal translation.
B: Single TF OA with K&L grade 4 and severe PF joint pathology or patellectomy.
Grade 4
4 A: Both TF joints are K&L grade 3 or 4 (< 5 mm space) with ligament stability.
4 B: Both TF joints
Rights and permissions
About this article
Cite this article
Oosthuizen, C.R., Van Der Straeten, C., Maposa, I. et al. The patient results and satisfaction of knee arthroplasty in a validated grading system. International Orthopaedics (SICOT) 43, 2747–2755 (2019). https://doi.org/10.1007/s00264-019-04412-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04412-z