Abstract
After analyzing treatment patterns in chronic lymphocytic leukemia (CLL) (objective 1), we investigated the relative effectiveness of ibrutinib versus other commonly used treatments (objective 2) in patients with treatment-naïve and relapsed/refractory CLL, comparing patient-level data from two randomized registration trials with two real-world databases. Hazard ratios (HR) and 95% confidence intervals (CIs) were estimated using a multivariate Cox proportional hazards model, adjusted for differences in baseline characteristics. Rituximab-containing regimens were often prescribed in clinical practice. The most frequently prescribed regimens were fludarabine + cyclophosphamide + rituximab (FCR, 29.3%), bendamustine + rituximab (BR, 17.7%), and other rituximab-containing regimens (22.0%) in the treatment-naïve setting (n = 604), other non-FCR/BR rituximab-containing regimens (38.7%) and non-rituximab–containing regimens (28.5%) in the relapsed/refractory setting (n = 945). Adjusted HRs (95% CI) for progression-free survival (PFS) and overall survival (OS), respectively, with ibrutinib versus real-world regimens were 0.23 (0.14–0.37; p < 0.0001) and 0.40 (0.22–0.76; p = 0.0048) in the treatment-naïve setting, and 0.21 (0.16–0.27; p < 0.0001) and 0.29 (0.21–0.41; p < 0.0001) in the relapsed/refractory setting. When comparing real-world use of ibrutinib (n = 53) versus other real-world regimens in relapsed/refractory CLL (objective 3), adjusted HRs (95% CI) were 0.37 (0.22–0.63; p = 0.0003) for PFS and 0.53 (0.27–1.03; p < 0.0624) for OS. This adjusted analysis, based on nonrandomized patient data, suggests ibrutinib to be more effective than other commonly used regimens for CLL.
Similar content being viewed by others
Introduction
Chronic lymphocytic leukemia (CLL) is the most common type of leukemia in adults [1, 2]. CLL primarily affects the elderly, with median age of onset of approximately 70 years [3]. Therapy for CLL has evolved from monotherapy with alkylating agents to chemoimmunotherapy [4, 5], often including an anti-CD20 antibody (e.g., rituximab, ofatumumab, or obinutuzumab) and combinations of fludarabine, cyclophosphamide, bendamustine, or chlorambucil [1, 6,7,8,9]. However, conventional CLL therapies, such as fludarabine + cyclophosphamide + rituximab (FCR), may have toxic side effects and are poorly tolerated in frail patients [1, 7]. Therefore, the trade-off between efficacy and toxicity requires consideration of patient fitness, particularly in the elderly [1, 3, 10].
Ibrutinib is a first-in-class, oral, once-daily covalent Bruton’s tyrosine kinase inhibitor approved in the USA [11], Europe [12], and other countries worldwide for patients with treatment-naïve (TN) and relapsed/refractory (R/R) CLL. In randomized registration trials of patients with CLL, ibrutinib significantly improved progression-free survival (PFS) and overall survival (OS) versus chlorambucil in TN patients (RESONATE-2™; NCT01722487) [13] and versus ofatumumab in R/R patients (RESONATE™; NCT01578707) [14]. Additional head-to-head clinical trial comparisons of ibrutinib-based regimens versus other widely used treatments (including current standard-of-care chemoimmunotherapy regimens and other novel regimens incorporated into CLL guidelines [15,16,17]) are ongoing [18, 19], and recent results from multiple phase 3 trials have been positive [data available as abstracts] [20,21,22].
Real-world (RW) evidence, derived from the analysis of RW data, is becoming increasingly important in understanding the impact of different diseases and treatments [23, 24]. The Platform for Hematology in Europe, Middle East, Africa (EMEA): Data for Real-life Analyses (PHEDRA) is a unique, noninterventional project based on secondary data collection from RW patient-level databases, and was developed to gain a better insight into the treatment of CLL (and other hematological malignancies) in clinical practice [25]. PHEDRA has three main objectives: (1) to describe treatment patterns; (2) to compare outcomes, PFS and OS, between patients treated with ibrutinib in randomized clinical trials (RCTs) and patients treated with commonly used treatment regimens in clinical practice; (3) to confirm that ibrutinib outcomes in the RCT setting are comparable with outcomes in clinical practice. Methods and findings relating to these objectives in CLL are reported here.
Subjects and methods
CLL databases and data extraction
Patient-level data (PLD) for CLL in clinical practice were obtained from independent RW databases from France and the Czech Republic and analyzed retrospectively. The Lyon-Sud dataset provided medical records for patients with CLL diagnosed between 1980 and 2017 at the academic Lyon-Sud Hospital in France, the main treatment center for hematological cancers in the region. The CLLEAR database provided records for CLL patients diagnosed between 1988 and 2017 within the catchment area of contributing local hospitals at seven academic centers in the Czech Republic, located in Brno, Hradec Králové, Nový Jičín, Olomouc, Ostrava, Plzeň, and Prague.
Detailed methods for the PHEDRA project have been published separately [25]. In brief, PLD collected from Lyon-Sud and CLLEAR were transformed into a common data model, which enabled the data to be pooled and analyzed. Data access complied with local data protection rules and regulations. Where required, participation was approved by the local independent ethics committee/institutional review board. PLD were fully anonymized for analyses.
Treatment patterns
Physicians’ choice (PC) regimens for CLL in clinical practice were identified from the RW databases and analyzed descriptively for the TN and R/R settings (relative to objective 1).
Adjusted comparisons of RCT and RW data
An adjusted comparison of PFS and OS outcomes was performed on PLD from the ibrutinib arms of RESONATE-2™ (TN CLL) or RESONATE™ (R/R CLL) versus other PC regimens (any treatment regimen being used in clinical practice, except for ibrutinib) in the RW databases (data pooled; objective 2). TN patients were included in the RW cohort for the adjusted comparisons if they met the inclusion criteria of RESONATE-2™ (aged ≥ 65 years and without del17p). All R/R CLL patients from the RW cohort were included in the adjusted comparisons versus RESONATE™.
To account for noncomparability of patient populations due to lack of randomization in RW databases (vs RCTs), a multivariate Cox proportional hazards regression model was used to derive adjusted hazard ratios (HRs) for the relative treatment effect of ibrutinib on PFS and OS versus PC in the RW cohort (i.e., if ibrutinib was used instead of the various actual treatments). Prognostic factors for OS and PFS included in the model were age, sex, and disease stage (based on Binet/Rai) (TN and R/R), as well as line of treatment for the R/R-analysis. The adjusted HRs for treatment effects and prognostic covariates are graphically presented by endpoint using forest plots (point estimate and 95% confidence interval [CI]).
Based on the multivariate model, predicted survival curves for PFS and OS were estimated by patient, using patient-specific baseline characteristics as covariates. A first survival curve represents the predicted patient-specific survival under treatment as observed. A second survival curve represents the predicted survival, simulating the outcomes of these patients as if they were treated with ibrutinib rather than the treatment actually received. The difference between the predicted survival curves represents the adjusted HR for ibrutinib relative to other PC treatments [25].
To assess whether the introduction of novel targeted therapies impacted the results of the adjusted comparisons in the TN or R/R setting, a sensitivity analysis was done, restricting the data to treatments received since 2005 (SA1). As therapies prior and/or subsequent to ibrutinib may have impacted long-term OS outcomes for PC treatments, additional sensitivity analyses were performed on the RW data, excluding all treatment lines following ibrutinib treatment (R/R setting, SA2) and removing all patients treated with ibrutinib from the PC cohort (TN and R/R setting, SA3).
Further sensitivity analyses were conducted in the R/R setting. To evaluate whether the benefit of ibrutinib versus non-ibrutinib PC treatments was consistent across treatment lines, the analyses were done separately for second-line treatment only, and third- and later line treatment.
PFS and OS outcomes in the RW cohort for patients treated with ibrutinib in the R/R setting were compared versus non-ibrutinib–containing PC treatments (objective 3), using a similar methodological approach as described for objective 2. Treatment lines for patients who were initiated on experimental treatment during a later treatment line were censored at the start of the experimental treatment. The number of patients receiving first-line ibrutinib was too low at the time of the data cut to do a similar comparison for TN patients.
Handling of missing data
To account for missing data on the date of onset of progressive disease in the RW cohort, the date of initiation of the next treatment was assigned as best proxy. As time to the next treatment is expected to be longer than PFS, this approach was considered conservative for ibrutinib [25].
Unit of observation for RW cohort analyses
The chosen unit of observation for the analyses of RW PLD was the treatment line, rather than the patient [25]: When a patient moved into further treatment lines, second- and subsequent treatment lines were included as separate observations. Patient characteristics captured at the initiation of each treatment line were included as covariates, to reflect their corresponding baseline status at that point.
Using an approach where multiple observations from the same patient are correlated goes against traditional assumptions regarding the independence of observations in statistical analyses. However, this was accounted and controlled for by using the robust sandwich estimate for the covariance matrix [26, 27], which makes standard errors and CIs around point estimates broader than if all observations had come from different patients (and were independent). This is more efficient from a statistical standpoint, as all available information in the data is leveraged in the analyses, provided that appropriate adjustment of the usual variance estimator has been implemented [28].
Results
Table 1 shows baseline and disease characteristics for the RCTs and pooled RW cohort by setting (reported by database in Online Resource Tables 1 [TN] and 2 [R/R]). Figure 1 shows the numbers of patients and treatment lines included in the analysis for the RW cohort.
RW database description for Lyon-Sud and CLLEAR. R/R relapsed/refractory, RW real-world, TN treatment-naïve. N refers to treatment lines in RW databases. For the TN cohort, the patient number equals the treatment line (i.e., one treatment line per patient). In the R/R cohort, patients could contribute to multiple treatment lines (and both the TN and the R/R analyses)
Treatment-naïve CLL patients
In the TN setting, including only patients aged ≥ 65 years and without del17p (and excluding ibrutinib treatment, n = 5), PLD from 115 and 489 patients in the Lyon-Sud and CLLEAR databases, respectively, were analyzed as the TN RW cohort (pooled number of patients, n = 604). Median age was 72 and 73 years, and 61.3% and 64.7% of patients were male, for the RW cohort and RESONATE-2™, respectively. Median follow-up was 30.0 months (Lyon-Sud: 69.0 months; CLLEAR: 23.1 months) and 29.1 months, respectively (Table 1) [13].
Description of PC treatments from the RW databases
The most commonly used treatment regimens in TN patients were rituximab-based therapy (n = 417 [69.0%]), including FCR (n = 177 [29.3%]), bendamustine + rituximab (BR; n = 107 [17.7%]), and other rituximab-containing regimens (n = 133 [22.0%]), anti-CD20 + chlorambucil (n = 59 [9.8%]), and chlorambucil alone (n = 55 [9.1%]) (Table 1).
Comparison of outcomes with RCT ibrutinib (RESONATE-2™) versus PC treatments from the RW databases
Across all treatments, multivariate analysis of combined data from the RW databases and RESONATE-2™ identified older age as an independent risk factor impacting PFS and OS; male sex was another independent risk factor for OS. There was a strong trend for advanced disease stage to be associated with decreased survival outcomes (Online Resource Fig. 1a, b). These risk factors were included in the Cox proportional hazards model.
The adjusted HR for ibrutinib versus PC therapy (pooled regimens) was 0.23 for PFS (95% CI 0.14–0.37; p < 0.0001) (Fig. 2a) and 0.40 for OS (95% CI 0.22–0.76; p = 0.0048) (Fig. 2b), versus the unadjusted HRs of 0.23 (95% CI 0.14–0.37; p < 0.0001) and 0.46 (95% CI 0.25–0.85; p = 0.0142), respectively (Online Resource Fig. 2a, b). Adjusted HRs for PFS for ibrutinib versus specific regimens (including FCR and BR) ranged between 0.32 (95% CI 0.17–0.60; p = 0.0004) for anti-CD20 + chlorambucil and 0.14 (95% CI 0.08–0.24; p < 0.0001) for chlorambucil (Fig. 2a). The adjusted HRs for OS ranged between 0.75 (95% CI 0.32–1.79; p = 0.5216) for anti-CD20 + chlorambucil and 0.21 (95% CI 0.11–0.43; p < 0.0001) for other regimens (see Table 1 footnote for definition) (Fig. 2b). Figure 3a, b shows predicted survival curves (derived from the multivariate Cox model) for OS and PFS, reflecting outcomes for the RW patient cohort as treated versus estimated outcomes for these same patients if they would have been treated with ibrutinib. The difference between the predicted curves reflects the adjusted HRs and provides a visual estimation of improved survival for ibrutinib over other treatments.
Adjusted HR (95% CI) for (a) PFS and (b) OS: RESONATE-2™ versus RW TN cohort. Indirect comparison of data from ibrutinib arm of RESONATE-2™ with patient-level data from RW cohort. BR bendamustine + rituximab, Chlor chlorambucil, CI confidence interval, FCR fludarabine + cyclophosphamide + rituximab, HR hazard ratio, Ibr ibrutinib, LCL lower confidence limit, OS overall survival, PC physicians’ choice, PFS progression-free survival, R rituximab, RW real-world, TN treatment-naïve, UCL upper confidence limit
Results were similar when only including patients treated since 2005 (n = 590 treatment lines, SA1): adjusted HRs for PFS and OS were 0.22 (95% CI 0.14–0.36; p < 0.0001) and 0.44 (95% CI 0.24–0.83; p = 0.0101), respectively. Removing all patients treated with RW ibrutinib from the PC cohort (n = 7, SA3) did not impact the comparisons for PFS and OS (Online Resource Fig. 3a, b).
Relapsed/refractory CLL patients
After excluding ibrutinib (n = 53 treatment lines), PLD were available from 131 patients (282 treatment lines) and 389 patients (663 treatment lines) in Lyon-Sud and CLLEAR, respectively (pooled number of patients, n = 520; pooled number of treatment lines analyzed, n = 945) (Fig. 1). The ibrutinib arm of RESONATE™ provided data for 195 patients.
In the RW R/R CLL cohort and RESONATE™, the median age was 68 and 67 years, 68.0% and 66.2% of patients were male, and median follow-up was 38.4 (Lyon-Sud: 70.0 months; CLLEAR: 31.7 months) and 44.0 months, respectively [13].
Description of PC treatments from the RW databases
The most commonly used PC regimens across all lines for R/R CLL were other rituximab-containing regimens (outside of FCR and BR) (n = 366 [38.7%]), other (non-rituximab–containing) regimens (n = 269 [28.5%]), FCR (n = 141 [14.9%]), BR (n = 91 [9.6%]), anti-CD20 + chlorambucil (n = 48 [5.1%]), and chlorambucil (n = 30 [3.2%]) (Table 1).
Comparison of outcomes with ibrutinib (RESONATE™) versus PC treatments from the RW databases
Multivariate analysis using the Cox proportional hazards model of the pooled dataset combining the RW R/R cohort and RESONATE™ data identified older age, advanced disease stage, and later lines of therapy as independent risk factors for both OS and PFS. There was also a clear trend for male sex to be an independent risk factor for both endpoints (Online Resource Fig. 1a, b).
Adjusted HRs for ibrutinib RCT data versus pooled PC treatment regimens from the RW databases were 0.21 (95% CI 0.16–0.27; p < 0.0001) for PFS (Fig. 4a) and 0.29 (95% CI 0.21–0.41; p < 0.0001) for OS (Fig. 4b) versus unadjusted HRs of 0.28 (95% CI 0.22–0.35; p < 0.0001) and 0.43 (95% CI 0.33–0.56; p < 0.0001), respectively (Online Resource Fig. 5a, b).
Adjusted HR (95% CI) for (a) PFS and (b) OS: RESONATE™ versus RW R/R cohort. Indirect comparison of data from ibrutinib arm of RESONATE™ with patient-level data from RW cohort. BR bendamustine + rituximab, Chlor chlorambucil, CI confidence interval, FCR fludarabine + cyclophosphamide + rituximab, HR hazard ratio, Ibr ibrutinib, LCL lower confidence limit, OS overall survival, PC physicians’ choice, PFS progression-free survival, R rituximab, R/R relapsed/refractory, RW real-world, UCL upper confidence limit
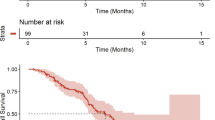
Predicted (a) PFS and (b) OS for R/R CLL: RESONATE™ versus RW R/R cohort. p value for ibrutinib versus PC. Median values are for PFS and OS (rather than follow-up). CLL chronic lymphocytic leukemia, OS overall survival, PC physicians’ choice, PFS progression-free survival, R/R relapsed/refractory, RW real-world
The adjusted HRs for PFS for ibrutinib versus commonly used PC treatment regimens from the RW databases ranged between 0.33 (95% CI 0.25–0.44; p < 0.0001 for FCR) and 0.17 (95% CI 0.13–0.22; p < 0.0001 for “other” regimens) (Fig. 4a). For OS, the adjusted HRs ranged between 0.44 (95% CI 0.30–0.65; p < 0.0001 for FCR) and 0.25 (95% CI 0.14–0.44; p < 0.0001 for anti-CD20 + chlorambucil) (Fig. 4b). Figure 5 a and b represent the predicted survival curves for PFS and OS, respectively, in the R/R setting.
The overall R/R results were similar when excluding patients treated before 2005 (n = 924 treatment lines, SA1): adjusted HRs for PFS and OS were 0.21 (95% CI 0.16–0.27; p < 0.0001) and 0.30 (95% CI 0.21–0.41; p < 0.0001), respectively. Additional sensitivity analyses showed that excluding post-ibrutinib treatment lines (SA2) or removing all patients treated with ibrutinib from the RW PC cohort (SA3) did not impact the outcomes (Online Resource Fig. 3a, b).
Adjusted HRs for PFS and OS (including age, sex, and disease stage in the model) for ibrutinib (n = 35) versus the PC regimens (n = 495) in second-line treatment only from the RW databases were 0.17 (95% CI 0.09–0.31; p < 0.0001) and 0.32 (95% CI 0.16–0.64; p = 0.0012), respectively (Fig. 6a, b). HRs and 95% CIs for ibrutinib versus individual regimens second-line were similar to those for ibrutinib (n = 160) versus the PC regimens (n = 450) in third- and later line treatment: 0.23 (95% CI 0.17–0.30; p < 0.0001) for PFS and 0.29 (95% CI 0.20–0.41; p < 0.0001) for OS (Fig. 7a, b).
Adjusted HR (95% CI) for (a) PFS and (b) OS for CLL second-line therapy: RESONATE™ versus RW R/R cohort. Indirect comparison of data from ibrutinib arm of RESONATE™ with patient-level data from RW cohort. BR bendamustine + rituximab, Chlor chlorambucil, CI confidence interval, CLL chronic lymphocytic leukemia, FCR fludarabine + cyclophosphamide + rituximab, HR hazard ratio, Ibr ibrutinib, LCL lower confidence limit, OS overall survival, PC physicians’ choice, PFS progression-free survival, R rituximab, R/R relapsed/refractory, RW real-world, UCL upper confidence limit
Adjusted HR (95% CI) for (a) PFS and (b) OS for CLL third- and later line therapy: RESONATE™ versus RW R/R cohort. Indirect comparison of data from ibrutinib arm of RESONATE™ with patient-level data from RW cohort. BR bendamustine + rituximab, Chlor chlorambucil, CI confidence interval, CLL chronic lymphocytic leukemia, FCR fludarabine + cyclophosphamide + rituximab, HR hazard ratio, Ibr ibrutinib, LCL lower confidence limit, OS overall survival, PC physicians’ choice, PFS progression-free survival, R rituximab, R/R relapsed/refractory, RW real-world, UCL upper confidence limit
Comparison of outcomes from the RW databases with ibrutinib versus PC treatments from the RW databases
Adjusted HRs for PFS and OS for ibrutinib (n = 53 patients/treatment lines; Table 1) versus PC regimens in the R/R setting (n = 945 treatment lines) were 0.37 (95% CI 0.22–0.63; p = 0.0003) for PFS (Fig. 8a) and 0.53 (95% CI 0.27–1.03; p = 0.0624) for OS (Fig. 8b), versus unadjusted HRs of 0.44 (95% CI 0.26–0.74; p = 0.0022) and 0.61 (95% CI 0.31–1.18; p = 0.1372), respectively (Online Resource Fig. 6a, b). These results were consistent versus individual PC regimens, except for FCR (0.61 [0.35–1.09]; p = 0.0932) for PFS, and FCR (0.81 [0.40–1.67]; p = 0.5649) and BR (0.79 [0.37–1.69]; p = 0.5402) for OS. The adjusted HR was statistically significant in favor of ibrutinib for OS versus anti-CD20 + chlorambucil, other rituximab-containing regimens, and other regimens (p < 0.05; Fig. 8b). The difference between the predicted survival curves (Online Resource Fig. 7a [PFS] and 7b [OS]) for ibrutinib versus PC treatment represents the corresponding adjusted HRs for this comparison.
Adjusted HR (95% CI) for (a) PFS and (b) OS for R/R CLL: ibrutinib RW data versus PCa. aPC cohort excludes any ibrutinib RW patients. BR bendamustine + rituximab, Chlor chlorambucil, CI confidence interval, CLL chronic lymphocytic leukemia, FCR fludarabine + cyclophosphamide + rituximab, HR hazard ratio, Ibr ibrutinib, LCL lower confidence limit, OS overall survival, PC physicians’ choice, PFS progression-free survival, R rituximab, R/R relapsed/refractory, RW real-world, UCL upper confidence limit
Discussion
Registrational phase 3 RCTs demonstrated the significant clinical benefits of ibrutinib in TN and R/R CLL versus chlorambucil (RESONATE-2™) and ofatumumab (RESONATE™), respectively [13, 14, 29, 30]. However, CLL treatment has advanced over the past few years, with an increase in available options for patients with TN or R/R disease. It is therefore informative to consider the comparative effectiveness of ibrutinib with other PC regimens being used in clinical practice.
In the current retrospective analyses, an adjusted comparison was performed using PLD on ibrutinib outcomes from RCTs versus outcomes for PC regimens from two existing RW databases in France and the Czech Republic. In the TN setting, the adjusted HRs for PFS and OS comparing ibrutinib from the RESONATE-2™ study and the RW PC cohort suggest a 4.3-fold improvement in PFS (i.e., the inverse of the reported HR of 0.23) and 2.5-fold (HR = 0.40) improvement in OS with ibrutinib. Comparative results for ibrutinib versus chlorambucil are in line with and confirm available RCT evidence in TN patients with CLL [13]. The adjusted comparison yielded similar findings in the R/R setting, with an estimated 4.8-fold (HR = 0.21) improvement in PFS and 3.4-fold (HR = 0.29) improvement in OS with ibrutinib versus PC regimens from the RW databases; results specific to anti-CD20 therapy are in line with those of the RESONATE™ trial, which had ofatumumab as a comparator [14]. These data show that ibrutinib is consistently associated with improved survival outcomes compared with other PC treatments across lines of therapy.
Sensitivity analyses excluding treatments received prior to 2005 did not impact the results in the TN or R/R setting and illustrate that ibrutinib therapy maintains its benefits compared with newer therapies and novel treatments, including anti-CD20 agents.
Other published analyses support the current findings, showing the clinical benefits of ibrutinib outside of RCTs [31]. Using similar methodology to the current study, PLD were collected from an observational cohort of R/R patients (n = 144) diagnosed with CLL between 2002 and 2013 in Sweden, and the ibrutinib arm of RESONATE™. Comparing survival outcomes for ibrutinib versus previous standard-of-care regimens used in second or later lines, the HRs (adjusted for age, sex, disease stage, performance status, and line of therapy) were 0.15 (p < 0.0001) for PFS and 0.36 (p < 0.0001) for OS, consistent with the results reported in this manuscript. HRs in line with these results have also been reported in studies using a similar modeling approach to compare PLD for single-agent ibrutinib from RESONATE™ with BR from the HELIOS trial (0.13 for PFS and 0.45 for OS) [data available as an abstract] [32].
The benefit of ibrutinib in the RW has also been shown to be comparable with that observed in clinical trials when analyzing data from patient access programs. Analysis of a series of 372 efficacy-evaluable patients with poor prognosis, R/R CLL from the French Temporary Authorization for Use database (December 2013 to November 2014) reported a best overall response rate of 88.5% with ibrutinib treatment after a median follow-up of 3 months [33] (similar to the 90% response rate reported in RESONATE™ at 12 months [14]). Results for 95 poor prognosis patients with CLL who were treated with ibrutinib in a Swedish compassionate use program (from May 2014 to May 2015) found in patients with R/R disease, with median follow-up of 10.2 months, the overall response rate was 84%, and 77% of patients were progression free (vs 88% at 6 months in RESONATE™) [14, 34]. A study of 216 R/R patients with CLL included in the named patient program for ibrutinib in Italy (from April 2014 to January 2015) reported an 80% response rate and PFS rate of 65% at 24 months [data available as an abstract] [35]. In addition, an observational retrospective study of data from 2908 patients with R/R CLL enrolled in the international named patient program for ibrutinib (from March 2014 to March 2015) found that estimated time on treatment (which broadly reflects PFS) in the RW was also similar to that observed in RESONATE™. Multivariate analysis showed that younger age (< 50 years) and achievement of complete or partial response to prior therapy were independent factors significantly associated with longer time on treatment [36].
It is important to note that, since our comparative analyses were conducted, additional data have become available from multiple phase 3 RCTs investigating ibrutinib in comparison with more modern and aggressive chemoimmunotherapy regimens for TN CLL than utilized in RESONATE-2™. These recent trial results support the benefit of ibrutinib-based regimens compared with modern standard therapeutic options. In the E1912 trial of young (≤ 70 years of age), fit patients with TN CLL, ibrutinib combined with rituximab led to superior PFS and OS compared with FCR [20], whereas in the ALLIANCE A014202 trial of fit, older patients (≥ 65 years of age), first-line treatment with single-agent ibrutinib or ibrutinib + rituximab significantly prolonged PFS compared with BR [21]. Further, in the iLLUMINATE study of patients with CLL and ≥ 65 years of age (or younger but with comorbidities), a chemotherapy-free regimen of ibrutinib + obinutuzumab improved PFS, response rates, and depth of remission compared with chlorambucil + obinutuzumab chemoimmunotherapy, irrespective of the presence of high-risk genomic features [22]. These RCT findings are likely to be practice changing in the TN setting. A recent cross-comparison of RCT data for ibrutinib from RESONATE-2™ and chemoimmunotherapy regimens from CLL8 (FCR), CLL10 (FCR and BR), CLL11 (obinutuzumab + chlorambucil and rituximab + chlorambucil), and COMPLEMENT-1 (ofatumumab + chlorambucil) found that PFS appeared longer with ibrutinib and OS was similar; in trials excluding patients with del17p (CLL10), or including older or less fit patients (CLL11), ibrutinib prolonged PFS in high-risk subgroups [37]. Although firm conclusions cannot be drawn from this analysis, the results are generally supportive of the favorable outcomes provided by ibrutinib in TN CLL populations compared with alternative standard regimens.
In the R/R setting, the current PHEDRA study is the first to compare outcomes for ibrutinib with other PC treatments in CLL patients from RW databases. HRs for PFS and OS confirmed the results of the ibrutinib RCT and RW database PC treatment comparison, suggesting that ibrutinib is more effective than several other frequently used regimens. However, results suggest the relative benefit (expressed as an HR) to be less in favor of ibrutinib than the RCT-based ibrutinib versus PC treatment comparison. As ibrutinib was first evaluated and approved for a more difficult to treat CLL population (i.e., in R/R disease/later lines of treatment, patients with del17p [14]), physicians might tend to reserve its use in patients with more advanced disease, or high-risk cytogenetic abnormalities, in clinical practice. Such channeling bias could then have led to a conservative estimate of the clinical benefit of ibrutinib versus PC treatment. There is also some uncertainty around the findings of the comparison of RW data owing to the small sample size for RW ibrutinib (n = 53), as reflected in the wide CIs. Further comparisons of outcomes with RW ibrutinib data versus PC treatment in both the TN and R/R CLL settings will be conducted as further data become available.
Our results should be interpreted in light of the following potential limitations. Firstly, estimates on OS benefit when comparing ibrutinib with specific regimens often had large CIs, due to the low number of events and small patient numbers. Pooling data from both RW databases helped to increase sample sizes and statistical power. Secondly, despite all attempts to adjust for differences between both compared patient populations, residual confounding cannot be excluded, as is the case for any nonrandomized comparison.
Some clinical factors, not consistently captured across the different data sources, may have also differed between the populations and may have led to residual bias. For instance, due to the high rate of missing cytogenetic baseline data (i.e., IGHV, del11q, or del17p status), mutational status could not be included or adjusted for in the multivariate analysis. However, compared with unadjusted analyses for both PFS and OS, adjustment for any of the available patient characteristics improved the HR in favor of ibrutinib, suggesting that any residual confounding factor may still bias results against ibrutinib. Exploratory analyses comparing the PFS and OS results with the RW database cohort excluding patients with missing del17p status showed only small numerical differences, indicating that inclusion or exclusion of these patients would not change the results.
Finally, the use of time to next treatment as proxy for missing progression dates (in the RW cohort only) may have biased results for PFS against ibrutinib, as time to next treatment is expected to be longer than PFS.
In conclusion, as therapeutic options continue to expand in CLL and there is no single standard-of-care regimen for all patients in the TN or R/R settings, it is worthwhile to compare the outcomes of different treatments in clinical practice as well as in RCTs. Our comparisons of outcomes for ibrutinib and PC treatments from two large high-quality data sources in CLL confirm RCT results, showing improved PFS and OS for ibrutinib over alternative regimens in both the TN and R/R settings. Outcomes for ibrutinib treatment based on RW data were also favorable. These findings extend available evidence on the benefit of ibrutinib versus a range of regimens, including those not yet evaluated in RCTs. Additionally, the results provide information on patient characteristics and treatment patterns, which is important given the absence of a pan-European registry of patients with CLL. Overall, the results from the PHEDRA project can help inform the choice of regimen for CLL across different lines of treatment.
References
Ghielmini M, Vitolo U, Kimby E, Montoto S, Walewski J, Pfreundschuh M, Federico M, Hoskin P, McNamara C, Caligaris-Cappio F, Stilgenbauer S, Marcus R, Trneny M, Dreger P, Montserrat E, Dreyling M (2013) ESMO guidelines consensus conference on malignant lymphoma 2011 part 1: diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL) and chronic lymphocytic leukemia (CLL). Ann Oncol 24(3):561–576. https://doi.org/10.1093/annonc/mds517
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Lewis DR, Chen HS, Feuer EJ, Cronin KA (2016) SEER Cancer Statistics Review, 1975-2013, National Cancer Institute. https://seer.cancer.gov/csr/1975_2013/. Accessed 6 November 2017
Shanafelt T (2013) Treatment of older patients with chronic lymphocytic leukemia: key questions and current answers. Hematology Am Soc Hematol Educ Program 2013:158–167. https://doi.org/10.1182/asheducation-2013.1.158
Goede V, Fischer K, Busch R, Engelke A, Eichhorst B, Wendtner CM, Chagorova T, de la Serna J, Dilhuydy MS, Illmer T, Opat S, Owen CJ, Samoylova O, Kreuzer KA, Stilgenbauer S, Dohner H, Langerak AW, Ritgen M, Kneba M, Asikanius E, Humphrey K, Wenger M, Hallek M (2014) Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions. N Engl J Med 370(12):1101–1110. https://doi.org/10.1056/NEJMoa1313984
Hallek M, Fischer K, Fingerle-Rowson G, Fink AM, Busch R, Mayer J, Hensel M, Hopfinger G, Hess G, von Grunhagen U, Bergmann M, Catalano J, Zinzani PL, Caligaris-Cappio F, Seymour JF, Berrebi A, Jager U, Cazin B, Trneny M, Westermann A, Wendtner CM, Eichhorst BF, Staib P, Buhler A, Winkler D, Zenz T, Bottcher S, Ritgen M, Mendila M, Kneba M, Dohner H, Stilgenbauer S (2010) Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet. 376(9747):1164–1174. https://doi.org/10.1016/S0140-6736(10)61381-5
Dutch/Belgium HOVON CLL Working Group (2016) Dutch guidelines for the diagnosis and treatment of chronic lymphocytic leukaemia. Neth J Med 74(2):68–74
Brown JR, Hallek MJ, Pagel JM (2017) Chemoimmunotherapy versus targeted treatment in chronic lymphocytic leukemia: when, how long, how much, and in which combination? In: ASCO Educational Book. American Society of Clinical Oncology, Alexandria, VA, pp e387–e398
Zelenetz AD, Abramson JS, Advani RH, Andreadis CB, Byrd JC, Czuczman MS, Fayad L, Forero A, Glenn MJ, Gockerman JP, Gordon LI, Harris NL, Hoppe RT, Horwitz SM, Kaminski MS, Kim YH, LaCasce AS, Mughal TI, Nademanee A, Porcu P, Press O, Prosnitz L, Reddy N, Smith MR, Sokol L, Swinnen L, Vose JM, Wierda WG, Yahalom J, Yunus F (2010) NCCN Clinical Practice Guidelines in Oncology: non-Hodgkin's lymphomas. J Natl Compr Cancer Netw 8(3):288–334
Zelenetz AD, Wierda WG, Abramson JS, Advani RH, Andreadis CB, Bartlett N, Bellam N, Byrd JC, Czuczman MS, Fayad LE, Glenn MJ, Gockerman JP, Gordon LI, Harris NL, Hoppe RT, Horwitz SM, Kelsey CR, Kim YH, Krivacic S, LaCasce AS, Nademanee A, Porcu P, Press O, Pro B, Reddy N, Sokol L, Swinnen L, Tsien C, Vose JM, Yahalom J, Zafar N, Dwyer MA, Naganuma M (2013) Non-Hodgkin's lymphomas, version 1.2013. J Natl Compr Cancer Netw 11(3):257–272
Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O, Marcos-Gragera R, Maynadie M, Simonetti A, Lutz JM, Berrino F (2010) Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 116(19):3724–3734. https://doi.org/10.1182/blood-2010-05-282632
IMBRUVICA® (2019) [prescribing information]. Pharmacyclics LLC, Sunnyvale, CA, Janssen Biotech, Inc., Horsham, PA.
IMBRUVICA (2019) [summary of product characteristics]. Janssen Pharmaceutica NV, Beerse, Belguim.
Burger JA, Tedeschi A, Barr PM, Robak T, Owen C, Ghia P, Bairey O, Hillmen P, Bartlett NL, Li J, Simpson D, Grosicki S, Devereux S, McCarthy H, Coutre S, Quach H, Gaidano G, Maslyak Z, Stevens DA, Janssens A, Offner F, Mayer J, O'Dwyer M, Hellmann A, Schuh A, Siddiqi T, Polliack A, Tam CS, Suri D, Cheng M, Clow F, Styles L, James DF, Kipps TJ (2015) Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med 373(25):2425–2437. https://doi.org/10.1056/NEJMoa1509388
Byrd JC, Brown JR, O'Brien S, Barrientos JC, Kay NE, Reddy NM, Coutre S, Tam CS, Mulligan SP, Jaeger U, Devereux S, Barr PM, Furman RR, Kipps TJ, Cymbalista F, Pocock C, Thornton P, Caligaris-Cappio F, Robak T, Delgado J, Schuster SJ, Montillo M, Schuh A, de Vos S, Gill D, Bloor A, Dearden C, Moreno C, Jones JJ, Chu AD, Fardis M, McGreivy J, Clow F, James DF, Hillmen P (2014) Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med 371(3):213–223. https://doi.org/10.1056/NEJMoa1400376
Eichhorst B, Robak T, Montserrat E, Ghia P, Hillmen P, Hallek M, Buske C, Guidelines Committee ESMO (2015) Chronic lymphocytic leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 26(Suppl 5):v78–v84. https://doi.org/10.1093/annonc/mdv303
National Comprehensive Cancer Network (2018) NCCN Clinical Practice Guidelines In Oncology (NCCN Guidelines). Chronic lymphocytic leukemia/small lymphocytic leukemia, v5.2018. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed 18 July 2018
Wierda WG, Zelenetz AD, Gordon LI, Abramson JS, Advani RH, Andreadis CB, Bartlett N, Byrd JC, Caimi P, Fayad LE, Fisher RI, Glenn MJ, Habermann TM, Harris NL, Hernandez-Ilizaliturri F, Hoppe RT, Horwitz SM, Kaminski MS, Kelsey CR, Kim YH, Krivacic S, LaCasce AS, Martin MG, Nademanee A, Porcu P, Press O, Rabinovitch R, Reddy N, Reid E, Roberts K, Saad AA, Snyder ED, Sokol L, Swinnen LJ, Vose JM, Yahalom J, Dwyer MA, Sundar H (2017) NCCN guidelines insights: chronic lymphocytic leukemia/small lymphocytic leukemia, version 1.2017. J Natl Compr Cancer Netw 15(3):293–311
Davids MS, Brown JR (2014) Ibrutinib: a first in class covalent inhibitor of Bruton's tyrosine kinase. Future Oncol 10(6):957–967. https://doi.org/10.2217/fon.14.51
Itchaki G, Brown JR (2018) Experience with ibrutinib for first-line use in patients with chronic lymphocytic leukemia. Ther Adv Hematol 9(1):3–19. https://doi.org/10.1177/2040620717741861
Shanafelt TD, Wang V, Kay NE, Hanson CA, O'Brien SM, Barrientos JC, Erba HP, Stone RM, Litzow MR, Tallman MS (2018) A randomized phase III study of ibrutinib (PCI-32765)-based therapy vs. standard fludarabine, cyclophosphamide, and rituximab (FCR) chemoimmunotherapy in untreated younger patients with chronic lymphocytic leukemia (CLL): a trial of the ECOG-ACRIN Cancer Research Group (E1912) [ASH abstract]. Blood 132:LBA–LB4. https://doi.org/10.1182/blood-2018-120779
Woyach JA, Ruppert AS, Heerema NA, Zhao W, Booth AM, Ding W, Bartlett NL, Brander DM, Barr P, Rogers KA, Parikh SA, Coutre S, Hurria A, Lozanski G, Nattam S, Larson RA, Erba HP, Litzow MR, Owen C, Atkins J, Abramson JS, Little RF, Smith SE, Stone RM, Mandrekar SJ, Byrd JC (2018) Ibrutinib alone or in combination with rituximab produces superior progression free survival (PFS) compared with bendamustine plus rituximab in untreated older patients with chronic lymphocytic leukemia (CLL): results of Alliance North American Intergroup Study A041202 [ASH abstract]. Blood. 132:6. https://doi.org/10.1182/blood-2018-99-116653
Moreno C, Greil R, Demirkan F, Tedeschi A, Anz B, Larratt L, Simkovic M, Samoilova O, Novak J, Ben-Yehuda D, Strugov V, Gill D, Gribben JG, Hsu E, Zhou C, Clow F, James DF, Styles L, Flinn IW (2018) Ibrutinib + obinutuzumab versus chlorambucil + obinutuzumab as first-line treatment in patients with chronic lymphocytic leukemia or small lymphocytic lymphoma (CLL/SLL): results from phase 3 iLLUMINATE [ASH abstract]. Blood. 132:691. https://doi.org/10.1182/blood-2018-99-111370
U.S. Food & Drug Administration (2018) Framework for FDA’s real-world evidence program. https://www.fda.gov/media/120060/download. Accessed 27 August 2019
Berger ML, Sox H, Willke RJ, Brixner DL, Eichler HG, Goettsch W, Madigan D, Makady A, Schneeweiss S, Tarricone R, Wang SV, Watkins J, Daniel Mullins C (2017) Good practices for real-world data studies of treatment and/or comparative effectiveness: recommendations from the joint ISPOR-ISPE Special Task Force on real-world evidence in health care decision making. Pharmacoepidemiol Drug Saf 26(9):1033–1039. https://doi.org/10.1002/pds.4297
Garside J, Healy N, Besson H, Hermans R, MacDougall F, Lestelle D, Diels J, Iraqi W (2018) PHEDRA: using real-world data to analyze treatment patterns and ibrutinib effectiveness in hematological malignancies. J Comp Eff Res 7(1):29–38. https://doi.org/10.2217/cer-2017-0046
Lin Y (2016) Robust inference for responder analysis: innovative clinical trial design using a minimum p-value approach. Contemp Clin Trials Commun 3:65–69. https://doi.org/10.1016/j.conctc.2016.04.001
Robins JM, Hernan MA, Brumback B (2000) Marginal structural models and causal inference in epidemiology. Epidemiology 11(5):550–560
Hernan MA, Robins JM (2016) Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol 183(8):758–764. https://doi.org/10.1093/aje/kwv254
Brown JR, Hillmen P, O'Brien S, Barrientos JC, Reddy NM, Coutre SE, Tam CS, Mulligan SP, Jaeger U, Barr PM, Furman RR, Kipps TJ, Cymbalista F, Thornton P, Caligaris-Cappio F, Delgado J, Montillo M, DeVos S, Moreno C, Pagel JM, Munir T, Burger JA, Chung D, Lin J, Gau L, Chang B, Cole G, Hsu E, James DF, Byrd JC (2018) Extended follow-up and impact of high-risk prognostic factors from the phase 3 RESONATE study in patients with previously treated CLL/SLL. Leukemia. 32(1):83–91. https://doi.org/10.1038/leu.2017.175
O'Brien S, Furman RR, Coutre S, Flinn IW, Burger JA, Blum K, Sharman J, Wierda W, Jones J, Zhao W, Heerema NA, Johnson AJ, Luan Y, James DF, Chu AD, Byrd JC (2018) Single-agent ibrutinib in treatment-naive and relapsed/refractory chronic lymphocytic leukemia: a 5-year experience. Blood. 131(17):1910–1919. https://doi.org/10.1182/blood-2017-10-810044
Hansson L, Asklid A, Diels J, Eketorp-Sylvan S, Repits J, Soltoft F, Jager U, Osterborg A (2017) Ibrutinib versus previous standard of care: an adjusted comparison in patients with relapsed/refractory chronic lymphocytic leukaemia. Ann Hematol 96(10):1681–1691. https://doi.org/10.1007/s00277-017-3061-3
Hillmen P, Fraser G, Jones J, Rule S, O’Brien S, Dilhuydy M, Jaeger U, Grosicki S, F. C, Sun S, Ninomoto J, Mahler M, Cheng M, Diels J, Clow F, Salman M, James D, Howes A, Chanan-Khan A (2015) Comparing single-agent ibrutinib, bendamustine plus rituximab (BR) and ibrutinib plus BR in patients with previously treated chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL): an indirect comparison of the RESONATE and HELIOS trials [ASH abstract]. Blood. 126(23):2944
Ysebaert L, Aurran-Schleinitz T, Dartigeas C, Dilhuydy MS, Feugier P, Michallet AS, Tournilhac O, Dupuis J, Sinet P, Albrecht C, Cymbalista F (2017) Real-world results of ibrutinib in relapsed/refractory CLL in France: early results on a large series of 428 patients. Am J Hematol 92(8):E166–E168. https://doi.org/10.1002/ajh.24773
Winqvist M, Asklid A, Andersson PO, Karlsson K, Karlsson C, Lauri B, Lundin J, Mattsson M, Norin S, Sandstedt A, Hansson L, Osterborg A (2016) Real-world results of ibrutinib in patients with relapsed or refractory chronic lymphocytic leukemia: data from 95 consecutive patients treated in a compassionate use program. A study from the Swedish Chronic Lymphocytic Leukemia Group. Haematologica. 101(12):1573–1580. https://doi.org/10.3324/haematol.2016.144576
Mauro FR, Soddu S, Frustaci AM, Orsucci L, Motta M, Scarfo L, Zinzani PL, Falzetti F, Farina L, Marasca R, Cortelezzi A, Carlo-Stella C, Molica S, Coscia M, Zaja F, Laurenti L, de Fabritiis P, Gaidano G, Gobbi M, Tani M, Di Renzo N, Fazi P, Vignetti M, Cuneo A, Foà R (2018) Outcome of patients with relapsed/refractory (R/R) chronic lymphocytic leukemia (CLL) treated with ibrutinib within a named patient program (NPP) in Italy. a real-life retrospective study [ASH abstract]. Blood 132:3147. https://doi.org/10.1182/blood-2018-99-116653
Hillmen P, Diels J, Healy N, Iraqi W, Aschan J, Wildgust M (2018) Ibrutinib for chronic lymphocytic leukemia: international experience from a named patient program. Haematologica. 103(5):e204–e206. https://doi.org/10.3324/haematol.2017.178798
Robak T, Burger JA, Tedeschi A, Barr PM, Owen C, Bairey O, Hillmen P, Simpson D, Grosicki S, Devereux S, McCarthy H, Coutre SE, Quach H, Gaidano G, Maslyak Z, Stevens DA, Moreno C, Gill DS, Flinn IW, Gribben JG, Mokatrin A, Cheng M, Styles L, James DF, Kipps TJ, Ghia P (2018) Single-agent ibrutinib versus chemoimmunotherapy regimens for treatment-naive patients with chronic lymphocytic leukemia: a cross-trial comparison of phase 3 studies. Am J Hematol 93(11):1402–1410. https://doi.org/10.1002/ajh.25259
Acknowledgments
The authors would like to thank the CLL database owners and their teams, the patients included in the databases, and IQVIA Real-World Insight Solutions for their collaboration in cleaning/extracting/harmonizing the data. The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.”
Funding
This study was sponsored by Janssen Pharmaceutica NV and Pharmacyclics LLC, an AbbVie Company. The real-world databases utilized are not owned by Janssen Pharmaceutica NV or IQVIA Real-World Insight Solutions. Writing assistance was provided by Jennifer Fuchs and Emma Fulkes, of Parexel, and funded by Janssen Global Services, LLC.
Author information
Authors and Affiliations
Contributions
GS, EB, NG, JG, WI, JD, and MD were involved in the concept and design of the study; GS, EB, LS, MSi, LB, AP, MSp, RU, DL, JL, EC-B, and MD were involved in the data acquisition and collection; GS, EB, LS, LB, AP, HB, NH, JG, WI, CP-L, RH, and MD were responsible for data analyses and interpretation. All authors reviewed the draft during development, provided comments for revision, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
GS received consultancy/honoraria/research funding from Roche/Genentech; consultancy/honoraria from Janssen, Celgene, Novartis, and Amgen; honoraria/research funding from Gilead; honoraria from Mundipharma; EB received consultancy/honoraria/research funding from Roche/Genentech; research funding from Mundipharma; consultancy/honoraria from Sandoz; honoraria from Amgen; LS received consultancy/honoraria/travel grants from Roche/Genentech, Janssen, Gilead, and AbbVie; MS received consultancy/honoraria/travel grants from Roche/Genentech, Janssen, and Gilead; AP, LB, and EC-B declare no competing financial interests; MS received consultancy/honoraria from AbbVie, Gilead, Janssen, and Roche; RU and DL received consultancy/honoraria from Gilead, Janssen, and Roche; HB, RH and JL are employees of IQVIA Real-World Insight Solutions; MD received consultancy/research funding from AbbVie; consultancy/honoraria from Gilead, Janssen, and Roche; NH, JG, WI, and CP-L are employees of Janssen Pharmaceutica NV; HB is a previous employee of Janssen Pharmaceutica NV; JD is an employee and equity owner of Janssen Pharmaceutica NV.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008
Informed consent
Informed consent was obtained from all patients for being included in the database. PLD were fully anonymized for analyses; re-identification was not permitted by the database owners.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Salles, G., Bachy, E., Smolej, L. et al. Single-agent ibrutinib in RESONATE-2™ and RESONATE™ versus treatments in the real-world PHEDRA databases for patients with chronic lymphocytic leukemia. Ann Hematol 98, 2749–2760 (2019). https://doi.org/10.1007/s00277-019-03830-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03830-8