Abstract
Purpose
Conventional methods of seeding decellularized heart valves for heart valve tissue engineering have led to inconsistent results in interstitial cellular repopulation, particularly of the distal valve leaflet, and notably distinct from documented re-endothelialization. The use of bioreactor conditioning mimicking physiologic parameters has been well explored but cellular infiltration remains challenging. Non-characteristic, non-physiologic conditioning parameters within a bioreactor, such as hypoxia and cyclic chamber pressure, may be used to increase the cellular infiltration leading to increased recellularization.
Methods
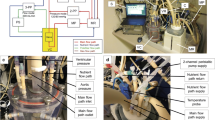
To investigate the effects of novel and perhaps non-intuitive bioreactor conditioning parameters, ovine aortic heart valves were seeded with mesenchymal stem cells and cultured in one of four environments: hypoxia and high cyclic pressures (120 mmHg), normoxia and high cyclic pressures, hypoxia and negative cyclic pressures (− 20 mmHg), and normoxia and negative cyclic pressures. Analysis included measurements of cellular density, cell phenotype, and biochemical concentrations.
Results
The results revealed that the bioreactor conditioning parameters influenced the degree of recellularization. Groups that implemented hypoxic conditioning exhibited increased cellular infiltration into the valve leaflet tissue compared to normoxic conditioning, while pressure conditioning did not have a significant effect of recellularization. Protein expression across all groups was similar, exhibiting a stem cell and valve interstitial cell phenotype. Biochemical analysis of the extracellular matrix was similar between all groups.
Conclusion
These results suggest the use of non-physiologic bioreactor conditioning parameters can increase in vitro recellularization of tissue engineered heart valve leaflets. Particularly, hypoxic culture was found to increase the cellular infiltration. Therefore, bioreactor conditioning of tissue engineered constructs need not always mimic physiologic conditions, and it is worth investigating novel or uncharacteristic culture conditions as they may benefit aspects of tissue culture.



Similar content being viewed by others
References
Annabi, B., et al. Hypoxia promotes murine bone-marrow-derived stromal cell migration and tube formation. Stem Cells 21(3):337–347, 2003.
Balguid, A., et al. Hypoxia induces near-native mechanical properties in engineered heart valve tissue. Circulation 119(2):290–297, 2009.
Ballotta, V., et al. Synergistic protein secretion by mesenchymal stromal cells seeded in 3D scaffolds and circulating leukocytes in physiological flow. Biomaterials 35(33):9100–9113, 2014.
Batten, P., et al. Human mesenchymal stem cells induce T cell anergy and downregulate T cell allo-responses via the TH2 pathway: relevance to tissue engineering human heart valves. Tissue Eng. 12(8):2263–2273, 2006.
Berry, J. L., et al. Bioreactors for development of tissue engineered heart valves. Ann. Biomed. Eng. 38(11):3272–3279, 2010.
Ciria, M., et al. Mesenchymal stem cell migration and proliferation are mediated by hypoxia-inducible factor-1alpha upstream of Notch and SUMO pathways. Stem Cells Dev 26(13):973–985, 2017.
Colazzo, F., et al. Extracellular matrix production by adipose-derived stem cells: implications for heart valve tissue engineering. Biomaterials 32(1):119–127, 2011.
Converse, G. L., et al. Poster: effects of decellularization of the viscoelastic behavior of the pulmonary valve leaflet. Biomedical Engineering Society 2011 Annual Meeting, 2011.
Converse, G. L., et al. Effects of cryopreservation, decellularization and novel extracellular matrix conditioning on the quasi-static and time-dependent properties of the pulmonary valve leaflet. Acta Biomater. 8(7):2722–2729, 2012.
Converse, G. L., et al. Design and efficacy of a single-use bioreactor for heart valve tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 105(2):249–259, 2015.
da Costa, F. D., et al. The early and midterm function of decellularized aortic valve allografts. Ann. Thorac. Surg. 90(6):1854–1860, 2010.
Dohmen, P. M. Clinical results of implanted tissue engineered heart valves. HSR Proc. Intensive Care Cardiovasc. Anesth. 4(4):225–231, 2012.
Dohmen, P. M., et al. Histological evaluation of tissue-engineered heart valves implanted in the juvenile sheep model: is there a need for in-vitro seeding? J. Heart Valve Dis. 15(6):823–829, 2006.
Dohmen, P. M., et al. In-vivo repopularization of a tissue-engineered heart valve in a human subject. J. Heart Valve Dis. 16(4):447–449, 2007.
Garreta, E., et al. Low oxygen tension enhances the generation of lung progenitor cells from mouse embryonic and induced pluripotent stem cells. Physiol Rep 2(7):e12075, 2014.
Harpa, M., et al. In vivo testing of xenogeneic acellular aortic valves seeded with stem cells. Rev. Rom. Med. Lab. 24(3):343–346, 2016.
Hopkins, R. From cadaver harvested homograft valves to tissue-engineered valve conduits. Prog. Pediatr. Cardiol. 21(2):137–152, 2006.
Huang, C., et al. Effect of negative pressure wound therapy on wound healing. Curr. Probl. Surg. 51(7):301–331, 2014.
Jana, S., R. T. Tranquillo, and A. Lerman. Cells for tissue engineering of cardiac valves. J. Tissue Eng. Regen. Med. 10:804–824, 2015.
Kajbafzadeh, A. M., et al. Aortic valve conduit implantation in the descending thoracic aorta in a sheep model: the outcomes of pre-seeded scaffold. Int. J. Surg. 28:97–105, 2016.
Kim, S. S., et al. Tissue engineering of heart valves by recellularization of glutaraldehyde-fixed porcine valves using bone marrow-derived cells. Exp. Mol. Med. 38(3):273–283, 2006.
Kinnaird, T., et al. Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ. Res. 94(5):678–685, 2004.
Lichtenberg, A., et al. Flow-dependent re-endothelialization of tissue-engineered heart valves. J. Heart Valve Dis. 15(2):287–293, 2006; (discussion 293-4).
Lichtenberg, A., et al. In vitro re-endothelialization of detergent decellularized heart valves under simulated physiological dynamic conditions. Biomaterials 27(23):4221–4229, 2006.
Liu, A. C., V. R. Joag, and A. I. Gotlieb. The emerging role of valve interstitial cell phenotypes in regulating heart valve pathobiology. Am. J. Pathol. 171(5):1407–1418, 2007.
Ma, T., et al. Hypoxia and stem cell-based engineering of mesenchymal tissues. Biotechnol. Prog. 25(1):32–42, 2009.
Merryman, W. D., et al. Correlation between heart valve interstitial cell stiffness and transvalvular pressure: implications for collagen biosynthesis. Am. J. Physiol. Heart Circ. Physiol. 290(1):H224–H231, 2006.
Neumann, A., et al. Early systemic cellular immune response in children and young adults receiving decellularized fresh allografts for pulmonary valve replacement. Tissue Eng. Part A 20(5–6):1003–1011, 2014.
Quinn, R. W., et al. Performance and morphology of decellularized pulmonary valves implanted in juvenile sheep. Ann. Thorac. Surg. 92(1):131–137, 2011.
Quinn, R., et al. Enhanced autologous re-endothelialization of decellularized and extracellular matrix conditioned allografts implanted into the right ventricular outflow tracts of juvenile sheep. Cardiovasc. Eng. Technol. 3(2):217–227, 2012.
Ramaswamy, S., et al. The role of organ level conditioning on the promotion of engineered heart valve tissue development in-vitro using mesenchymal stem cells. Biomaterials 31(6):1114–1125, 2010.
Rath, S., et al. Differentiation and distribution of marrow stem cells in flex-flow environments demonstrate support of the valvular phenotype. PLoS ONE 10(11):e0141802, 2015.
Sarikouch, S., et al. Decellularized fresh homografts for pulmonary valve replacement: a decade of clinical experience. Eur. J. Cardiothorac. Surg. 50:281–290, 2016.
Schenke-Layland, K., et al. Complete dynamic repopulation of decellularized heart valves by application of defined physical signals-an in vitro study. Cardiovasc. Res. 60(3):497–509, 2003.
Schoen, F. J. Cardiac valves and valvular pathology: update on function, disease, repair, and replacement. Cardiovasc. Pathol. 14(4):189–194, 2005.
Sierad, L. N., et al. Design and testing of a pulsatile conditioning system for dynamic endothelialization of polyphenol-stabilized tissue engineered heart valves. Cardiovasc. Eng. Technol. 1(2):138–153, 2010.
Simon, P., et al. Early failure of the tissue engineered porcine heart valve SYNERGRAFT in pediatric patients. Eur. J. Cardiothorac. Surg. 23(6):1002–1006, 2003; (discussion 1006).
VeDepo, M. C., et al. Recellularization of decellularized heart valves: progress toward the tissue-engineered heart valve. J. Tissue Eng. 8:2041731417726327, 2017.
VeDepo, M. C., et al. Species-specific effects of aortic valve decellularization. Acta Biomater. 50:249–258, 2017.
Vincentelli, A., et al. In vivo autologous recellularization of a tissue-engineered heart valve: are bone marrow mesenchymal stem cells the best candidates? J. Thorac. Cardiovasc. Surg. 134(2):424–432, 2007.
Xu, W., et al. Hypoxia changes chemotaxis behaviour of mesenchymal stem cells via HIF-1alpha signalling. J. Cell Mol. Med. 23(3):1899–1907, 2019.
Conflict of interest
M. VeDepo, E. Buse, A. Paul, G. Converse, and R. Hopkins declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Jane Grande-Allen oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
VeDepo, M.C., Buse, E.E., Paul, A. et al. Non-physiologic Bioreactor Processing Conditions for Heart Valve Tissue Engineering. Cardiovasc Eng Tech 10, 628–637 (2019). https://doi.org/10.1007/s13239-019-00438-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-019-00438-x