Abstract
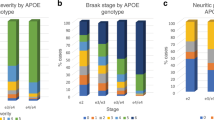
Cerebral amyloid angiopathy (CAA) often coexists with Alzheimer’s disease (AD). APOE4 is a strong genetic risk factor for both AD and CAA. Sex-dependent differences have been shown in AD as well as in cerebrovascular diseases. Therefore, we examined the effects of APOE4, sex, and pathological components on CAA in AD subjects. A total of 428 autopsied brain samples from pathologically confirmed AD cases were analyzed. CAA severity was histologically scored in inferior parietal, middle frontal, motor, superior temporal and visual cortexes. In addition, subgroups with severe CAA (n = 60) or without CAA (n = 39) were subjected to biochemical analysis of amyloid-β (Aβ) and apolipoprotein E (apoE) by ELISA in the temporal cortex. After adjusting for age, Braak neurofibrillary tangle stage and Thal amyloid phase, we found that overall CAA scores were higher in males than females. Furthermore, carrying one or more APOE4 alleles was associated with higher overall CAA scores. Biochemical analysis revealed that the levels of detergent-soluble and detergent-insoluble Aβ40, and insoluble apoE were significantly elevated in individuals with severe CAA or APOE4. The ratio of Aβ40/Aβ42 in insoluble fractions was also increased in the presence of CAA or APOE4, although it was negatively associated with male sex. Levels of insoluble Aβ40 were positively associated with those of insoluble apoE, which were strongly influenced by CAA status. Pertaining to insoluble Aβ42, the levels of apoE correlated regardless of CAA status. Our results indicate that sex and APOE genotypes differentially influence the presence and severity of CAA in AD, likely by affecting interaction and aggregation of Aβ40 and apoE.





Similar content being viewed by others

References
Altmann A, Tian L, Henderson VW, Greicius MD (2014) Sex modifies the APOE-related risk of developing Alzheimer disease. Ann Neurol 75:563–573. doi:10.1002/ana.24135
Alzheimer’sAssociation (2015) 2015 Alzheimer’s disease facts and figures. Alzheimer’s Dement 11:332–384
Attems J (2005) Sporadic cerebral amyloid angiopathy: pathology, clinical implications, and possible pathomechanisms. Acta Neuropathol 110:345–359. doi:10.1007/s00401-005-1074-9
Bakker EN, Bacskai BJ, Arbel-Ornath M, Aldea R, Bedussi B, Morris AW, Weller RO, Carare RO (2016) Lymphatic clearance of the brain: perivascular, paravascular and significance for neurodegenerative diseases. Cell Mol Neurobiol. doi:10.1007/s10571-015-0273-8
Barnes LL, Wilson RS, Bienias JL, Schneider JA, Evans DA, Bennett DA (2005) Sex differences in the clinical manifestations of Alzheimer disease pathology. Arch Gen Psychiatry 62:685–691. doi:10.1001/archpsyc.62.6.685
Bell RD, Winkler EA, Singh I, Sagare AP, Deane R, Wu Z, Holtzman DM, Betsholtz C, Armulik A, Sallstrom J et al (2012) Apolipoprotein E controls cerebrovascular integrity via cyclophilin A. Nature 485:512–516. doi:10.1038/nature11087
Biffi A, Sonni A, Anderson CD, Kissela B, Jagiella JM, Schmidt H, Jimenez-Conde J, Hansen BM, Fernandez-Cadenas I, Cortellini L et al (2010) Variants at APOE influence risk of deep and lobar intracerebral hemorrhage. Ann Neurol 68:934–943. doi:10.1002/ana.22134
Bu G (2009) Apolipoprotein E and its receptors in Alzheimer’s disease: pathways, pathogenesis and therapy. Nat Rev Neurosci 10:333–344. doi:10.1038/nrn2620
Carter CL, Resnick EM, Mallampalli M, Kalbarczyk A (2012) Sex and gender differences in Alzheimer’s disease: recommendations for future research. J Womens Health (Larchmt) 21:1018–1023. doi:10.1089/jwh.2012.3789
Corder EH, Ghebremedhin E, Taylor MG, Thal DR, Ohm TG, Braak H (2004) The biphasic relationship between regional brain senile plaque and neurofibrillary tangle distributions: modification by age, sex, and APOE polymorphism. Ann N Y Acad Sci 1019:24–28. doi:10.1196/annals.1297.005
de la Torre JC (2002) Alzheimer disease as a vascular disorder: nosological evidence. Stroke 33:1152–1162
Ellis RJ, Olichney JM, Thal LJ, Mirra SS, Morris JC, Beekly D, Heyman A (1996) Cerebral amyloid angiopathy in the brains of patients with Alzheimer’s disease: the CERAD experience, part XV. Neurology 46:1592–1596
Esiri M, Chance S, Joachim C, Warden D, Smallwood A, Sloan C, Christie S, Wilcock G, Smith AD (2015) Cerebral amyloid angiopathy, subcortical white matter disease and dementia: literature review and study in OPTIMA. Brain Pathol 25:51–62. doi:10.1111/bpa.12221
Filippini N, Ebmeier KP, MacIntosh BJ, Trachtenberg AJ, Frisoni GB, Wilcock GK, Beckmann CF, Smith SM, Matthews PM, Mackay CE (2011) Differential effects of the APOE genotype on brain function across the lifespan. Neuroimage 54:602–610. doi:10.1016/j.neuroimage.2010.08.009
Fryer JD, Simmons K, Parsadanian M, Bales KR, Paul SM, Sullivan PM, Holtzman DM (2005) Human apolipoprotein E4 alters the amyloid-beta 40:42 ratio and promotes the formation of cerebral amyloid angiopathy in an amyloid precursor protein transgenic model. J Neurosci 25:2803–2810. doi:10.1523/JNEUROSCI.5170-04.2005
Gahr M, Nowak DA, Connemann BJ, Schonfeldt-Lecuona C (2013) Cerebral Amyloidal Angiopathy—a disease with implications for neurology and psychiatry. Brain Res 1519:19–30. doi:10.1016/j.brainres.2013.04.052
Gravina SA, Ho L, Eckman CB, Long KE, Otvos L Jr, Younkin LH, Suzuki N, Younkin SG (1995) Amyloid beta protein (A beta) in Alzheimer’s disease brain. Biochemical and immunocytochemical analysis with antibodies specific for forms ending at A beta 40 or A beta 42(43). J Biol Chem 270:7013–7016
Greenberg SM, Al-Shahi Salman R, Biessels GJ, van Buchem M, Cordonnier C, Lee JM, Montaner J, Schneider JA, Smith EE, Vernooij M et al (2014) Outcome markers for clinical trials in cerebral amyloid angiopathy. Lancet Neurol 13:419–428. doi:10.1016/S1474-4422(14)70003-1
Harold D, Abraham R, Hollingworth P, Sims R, Gerrish A, Hamshere ML, Pahwa JS, Moskvina V, Dowzell K, Williams A et al (2009) Genome-wide association study identifies variants at CLU and PICALM associated with Alzheimer’s disease. Nat Genet 41:1088–1093. doi:10.1038/ng.440
Herzig MC, Van Nostrand WE, Jucker M (2006) Mechanism of cerebral beta-amyloid angiopathy: murine and cellular models. Brain Pathol 16:40–54
Huang Y, Mucke L (2012) Alzheimer mechanisms and therapeutic strategies. Cell 148:1204–1222. doi:10.1016/j.cell.2012.02.040
Kanekiyo T, Xu H, Bu G (2014) ApoE and Abeta in Alzheimer’s disease: accidental encounters or partners? Neuron 81:740–754. doi:10.1016/j.neuron.2014.01.045
Krause DN, Duckles SP (1985) Pelligrino DA (2006) Influence of sex steroid hormones on cerebrovascular function. J Appl Physiol 101:1252–1261. doi:10.1152/japplphysiol.01095.2005
La Porte SL, Bollini SS, Lanz TA, Abdiche YN, Rusnak AS, Ho WH, Kobayashi D, Harrabi O, Pappas D, Mina EW et al (2012) Structural basis of C-terminal beta-amyloid peptide binding by the antibody ponezumab for the treatment of Alzheimer’s disease. J Mol Biol 421:525–536. doi:10.1016/j.jmb.2011.11.047
Lambert JC, Heath S, Even G, Campion D, Sleegers K, Hiltunen M, Combarros O, Zelenika D, Bullido MJ, Tavernier B et al (2009) Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer’s disease. Nat Genet 41:1094–1099. doi:10.1038/ng.439
Liu CC, Kanekiyo T, Xu H, Bu G (2013) Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy. Nat Rev Neurol 9:106–118. doi:10.1038/nrneurol.2012.263
Maia LF, Mackenzie IR, Feldman HH (2007) Clinical phenotypes of cerebral amyloid angiopathy. J Neurol Sci 257:23–30. doi:10.1016/j.jns.2007.01.054
Mandybur TI (1986) Cerebral amyloid angiopathy: the vascular pathology and complications. J Neuropathol Exp Neurol 45:79–90
Miller DL, Papayannopoulos IA, Styles J, Bobin SA, Lin YY, Biemann K, Iqbal K (1993) Peptide compositions of the cerebrovascular and senile plaque core amyloid deposits of Alzheimer’s disease. Arch Biochem Biophys 301:41–52. doi:10.1006/abbi.1993.1112
Morris AW, Sharp MM, Albargothy NJ, Fernandes R, Hawkes CA, Verma A, Weller RO, Carare RO (2016) Vascular basement membranes as pathways for the passage of fluid into and out of the brain. Acta Neuropathol. doi:10.1007/s00401-016-1555-z
Murray ME, Graff-Radford NR, Ross OA, Petersen RC, Duara R, Dickson DW (2011) Neuropathologically defined subtypes of Alzheimer’s disease with distinct clinical characteristics: a retrospective study. Lancet Neurol 10:785–796. doi:10.1016/S1474-4422(11)70156-9
Nelson PT, Pious NM, Jicha GA, Wilcock DM, Fardo DW, Estus S, Rebeck GW (2013) APOE-epsilon2 and APOE-epsilon4 correlate with increased amyloid accumulation in cerebral vasculature. J Neuropathol Exp Neurol 72:708–715. doi:10.1097/NEN.0b013e31829a25b9
Nicoll JA, Burnett C, Love S, Graham DI, Dewar D, Ironside JW, Stewart J, Vinters HV (1997) High frequency of apolipoprotein E epsilon 2 allele in hemorrhage due to cerebral amyloid angiopathy. Ann Neurol 41:716–721. doi:10.1002/ana.410410607
Petrea RE, Beiser AS, Seshadri S, Kelly-Hayes M, Kase CS, Wolf PA (2009) Gender differences in stroke incidence and poststroke disability in the Framingham heart study. Stroke 40:1032–1037. doi:10.1161/STROKEAHA.108.542894
Pu Y, Liu L, Wang Y, Zou X, Pan Y, Soo Y, Leung T, Zhao X, Wong KS (2013) Geographic and sex difference in the distribution of intracranial atherosclerosis in China. Stroke 44:2109–2114. doi:10.1161/STROKEAHA.113.001522
Rannikmae K, Kalaria RN, Greenberg SM, Chui HC, Schmitt FA, Samarasekera N, Al-Shahi Salman R, Sudlow CL (2014) APOE associations with severe CAA-associated vasculopathic changes: collaborative meta-analysis. J Neurol Neurosurg Psychiatry 85:300–305. doi:10.1136/jnnp-2013-306485
Rensink AA, de Waal RM, Kremer B, Verbeek MM (2003) Pathogenesis of cerebral amyloid angiopathy. Brain Res Brain Res Rev 43:207–223
Revesz T, Ghiso J, Lashley T, Plant G, Rostagno A, Frangione B, Holton JL (2003) Cerebral amyloid angiopathies: a pathologic, biochemical, and genetic view. J Neuropathol Exp Neurol 62:885–898
Ringman JM, Sachs MC, Zhou Y, Monsell SE, Saver JL, Vinters HV (2014) Clinical predictors of severe cerebral amyloid angiopathy and influence of APOE genotype in persons with pathologically verified Alzheimer disease. JAMA Neurol 71:878–883. doi:10.1001/jamaneurol.2014.681
Schmechel DE, Saunders AM, Strittmatter WJ, Crain BJ, Hulette CM, Joo SH, Pericak-Vance MA, Goldgaber D, Roses AD (1993) Increased amyloid beta-peptide deposition in cerebral cortex as a consequence of apolipoprotein E genotype in late-onset Alzheimer disease. Proc Natl Acad Sci USA 90:9649–9653
Selkoe DJ (2002) Deciphering the genesis and fate of amyloid beta-protein yields novel therapies for Alzheimer disease. J Clin Invest 110:1375–1381. doi:10.1172/JCI16783
Shinohara M, Fujioka S, Murray ME, Wojtas A, Baker M, Rovelet-Lecrux A, Rademakers R, Das P, Parisi JE, Graff-Radford NR et al (2014) Regional distribution of synaptic markers and APP correlate with distinct clinicopathological features in sporadic and familial Alzheimer’s disease. Brain 137:1533–1549. doi:10.1093/brain/awu046
Shinohara M, Petersen RC, Dickson DW, Bu G (2013) Brain regional correlation of amyloid-beta with synapses and apolipoprotein E in non-demented individuals: potential mechanisms underlying regional vulnerability to amyloid-beta accumulation. Acta Neuropathol 125:535–547. doi:10.1007/s00401-013-1086-9
Soontornniyomkij V, Lynch MD, Mermash S, Pomakian J, Badkoobehi H, Clare R, Vinters HV (2010) Cerebral microinfarcts associated with severe cerebral beta-amyloid angiopathy. Brain Pathol 20:459–467. doi:10.1111/j.1750-3639.2009.00322.x
Suzuki N, Iwatsubo T, Odaka A, Ishibashi Y, Kitada C, Ihara Y (1994) High tissue content of soluble beta 1-40 is linked to cerebral amyloid angiopathy. Am J Pathol 145:452–460
Thal DR, Papassotiropoulos A, Saido TC, Griffin WS, Mrak RE, Kolsch H, Del Tredici K, Attems J, Ghebremedhin E (2010) Capillary cerebral amyloid angiopathy identifies a distinct APOE epsilon4-associated subtype of sporadic Alzheimer’s disease. Acta Neuropathol 120:169–183. doi:10.1007/s00401-010-0707-9
Thambisetty M, Beason-Held L, An Y, Kraut MA, Resnick SM (2010) APOE epsilon4 genotype and longitudinal changes in cerebral blood flow in normal aging. Arch Neurol 67:93–98. doi:10.1001/archneurol.2009.913
Vinters HV (1987) Cerebral amyloid angiopathy. A critical review. Stroke 18:311–324
Vinters HV, Gilbert JJ (1983) Cerebral amyloid angiopathy: incidence and complications in the aging brain. II. The distribution of amyloid vascular changes. Stroke 14:924–928
Weller RO, Subash M, Preston SD, Mazanti I, Carare RO (2008) Perivascular drainage of amyloid-beta peptides from the brain and its failure in cerebral amyloid angiopathy and Alzheimer’s disease. Brain Pathol 18:253–266. doi:10.1111/j.1750-3639.2008.00133.x
Zlokovic BV (2013) Cerebrovascular effects of apolipoprotein e: implications for Alzheimer disease. JAMA Neurol 70:440–444. doi:10.1001/jamaneurol.2013.2152
Acknowledgments
This work was supported by NIH Grants RF1AG051504, R01AG027924, R01AG035355, R01AG046205, and P01 NS074969 (to G. B.), P50 AG016574 (to G. B. and R. C. P.), U01AG006786 and R01AG034676 (to R. C. P.), and R01NS094137 (to J. D. F), grants from Florida Department of Health Ed and Ethel Moore Alzheimer’s Disease Research Program [to G. B. (5AZ08) and M. E. M (6AZ01)], and a Scientist Development Grant from the American Heart Association (to T. K.). The authors would like to acknowledge the continuous commitment and teamwork offered by Amanda M. Liesinger, Linda G. Rousseau, Virginia R. Phillips, and Monica Castanedes-Casey for their dedicated efforts to Mayo Clinic Brain Bank.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
R. C. Petersen: Consultant to Roche, Inc., Merck, Inc., Genentech, Inc., Biogen, Inc., Eli Lilly and Co.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shinohara, M., Murray, M.E., Frank, R.D. et al. Impact of sex and APOE4 on cerebral amyloid angiopathy in Alzheimer’s disease. Acta Neuropathol 132, 225–234 (2016). https://doi.org/10.1007/s00401-016-1580-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-016-1580-y