Abstract
Purpose
To culturally adapt the Patient-Reported Outcomes Measurement Information System-29 into Thai (T-PROMIS-29) and evaluate the reliability and validity of the culturally adapted questionnaire.
Methods
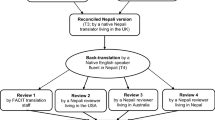
The translation was performed using the Functional Assessment of Chronic Illness Therapy (FACIT) translation guidelines. Unidimensionality, internal consistency, and test–retest reliability at a 1-week interval for the translated measure were computed. Construct validity was evaluated by computing correlations between the T-PROMIS-29 scores and selected SF-36 scale scores.
Results
The study sample comprised of 241 participants with chronic low back pain. Internal consistencies were good to excellent, with Cronbach’s alphas ranging from 0.84 to 0.94. The test–retest stability of all T-PROMIS-29 domains were moderate to good, with ICCs(2,1) ranging from 0.57 to 0.74. Unidimensionality, convergent validity, and divergent construct validity were satisfactory.
Conclusions
The findings support the reliability and validity of the T-PROMIS-29 scale scores. The measure can be used to assess key quality of life domains in individuals from Thailand with chronic low back pain.
Similar content being viewed by others
References
Breivik, H., Collett, B., Ventafridda, V., Cohen, R., & Gallacher, D. (2006). Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. European Journal of Pain,10(4), 287–333. https://doi.org/10.1016/j.ejpain.2005.06.009.
Kawai, K., Kawai, A. T., Wollan, P., & Yawn, B. P. (2017). Adverse impacts of chronic pain on health-related quality of life, work productivity, depression and anxiety in a community-based study. Family Practice,34(6), 656–661. https://doi.org/10.1093/fampra/cmx034.
Bjornsdottir, S. V., Jonsson, S. H., & Valdimarsdottir, U. A. (2014). Mental health indicators and quality of life among individuals with musculoskeletal chronic pain: A nationwide study in Iceland. Scandinavian Journal of Rheumatology,43(5), 419–423. https://doi.org/10.3109/03009742.2014.881549.
Hirase, T., Kataoka, H., Inokuchi, S., Nakano, J., Sakamoto, J., & Okita, M. (2017). Factors associated with chronic musculoskeletal pain in Japanese community-dwelling older adults: A cross-sectional study. Medicine (Baltimore),96(23), e7069. https://doi.org/10.1097/MD.0000000000007069.
Husky, M. M., Ferdous Farin, F., Compagnone, P., Fermanian, C., & Kovess-Masfety, V. (2018). Chronic back pain and its association with quality of life in a large French population survey. Health and Quality of Life Outcomes,16(1), 195. https://doi.org/10.1186/s12955-018-1018-4.
Gore, M., Sadosky, A., Stacey, B. R., Tai, K. S., & Leslie, D. (2012). The burden of chronic low back pain: Clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine (Phila Pa 1976),37(11), E668–E677. https://doi.org/10.1097/brs.0b013e318241e5de.
Choi, Y. S., Kim, D. J., Lee, K. Y., Park, Y. S., Cho, K. J., Lee, J. H., et al. (2014). How does chronic back pain influence quality of life in koreans: A cross-sectional study. Asian Spine Journal,8(3), 346–352. https://doi.org/10.4184/asj.2014.8.3.346.
Wettstein, M., Eich, W., Bieber, C., & Tesarz, J. (2019). Pain intensity, disability, and quality of life in patients with chronic low back pain: Does age matter? Pain Medicine,20(3), 464–475. https://doi.org/10.1093/pm/pny062.
Roland, M., & Morris, R. (1983). A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976),8(2), 141–144. https://doi.org/10.1097/00007632-198303000-00004.
Fairbank, J. C., Couper, J., Davies, J. B., & O’Brien, J. P. (1980). The Oswestry low back pain disability questionnaire. Physiotherapy,66(8), 271–273.
Kopec, J. A., Esdaile, J. M., Abrahamowicz, M., Abenhaim, L., Wood-Dauphinee, S., Lamping, D. L., et al. (1996). The Quebec Back Pain Disability Scale: Conceptualization and development. Journal of Clinical Epidemiology,49(2), 151–161.
Jirarattanaphochai, K., Jung, S., Sumananont, C., & Saengnipanthkul, S. (2005). Reliability of the Roland- Morris Disability Questionnaire (Thai version) for the evaluation of low back pain patients. Journal of the Medical Association of Thailand,88(3), 407–411.
Sanjaroensuttikul, N. (2007). The Oswestry low back pain disability questionnaire (version 1.0) Thai version. Journal of the Medical Association of Thailand,90(7), 1417–1422.
Felce, D., & Perry, J. (1995). Quality of life: Its definition and measurement. Research in Developmental Disabilities,16(1), 51–74.
Cella, D., Yount, S., Rothrock, N., Gershon, R., Cook, K., Reeve, B., et al. (2007). The patient-reported outcomes measurement information system (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care,45(5 Suppl 1), S3–S11. https://doi.org/10.1097/01.mlr.0000258615.42478.55.
Deyo, R. A., Dworkin, S. F., Amtmann, D., Andersson, G., Borenstein, D., Carragee, E., et al. (2014). Report of the NIH Task Force on research standards for chronic low back pain. The Journal of Pain,15(6), 569–585. https://doi.org/10.1016/j.jpain.2014.03.005.
Deyo, R. A., Katrina, R., Buckley, D. I., Michaels, L., Kobus, A., Eckstrom, E., et al. (2016). Performance of a patient reported outcomes measurement information system (PROMIS) short form in older adults with chronic musculoskeletal pain. Pain Medicine,17(2), 314–324. https://doi.org/10.1093/pm/pnv046.
Kroenke, K., Yu, Z., Wu, J., Kean, J., & Monahan, P. O. (2014). Operating characteristics of PROMIS four-item depression and anxiety scales in primary care patients with chronic pain. Pain Medicine,15(11), 1892–1901. https://doi.org/10.1111/pme.12537.
Askew, R. L., Cook, K. F., Revicki, D. A., Cella, D., & Amtmann, D. (2016). Evidence from diverse clinical populations supported clinical validity of PROMIS pain interference and pain behavior. Journal of Clinical Epidemiology,73, 103–111. https://doi.org/10.1016/j.jclinepi.2015.08.035.
Cook, K. F., Jensen, S. E., Schalet, B. D., Beaumont, J. L., Amtmann, D., Czajkowski, S., et al. (2016). PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. Journal of Clinical Epidemiology,73, 89–102. https://doi.org/10.1016/j.jclinepi.2015.08.038.
Purvis, T. E., Andreou, E., Neuman, B. J., Riley, L. H., 3rd, & Skolasky, R. L. (2017). Concurrent validity and responsiveness of PROMIS health domains among patients presenting for anterior cervical spine surgery. Spine (Phila Pa 1976),42(23), E1357–E1365. https://doi.org/10.1097/brs.0000000000002347.
Terwee, C. B., Roorda, L. D., de Vet, H. C., Dekker, J., Westhovens, R., van Leeuwen, J., et al. (2014). Dutch-Flemish translation of 17 item banks from the patient-reported outcomes measurement information system (PROMIS). Quality of Life Research,23(6), 1733–1741. https://doi.org/10.1007/s11136-013-0611-6.
Eremenco, S. L., Cella, D., & Arnold, B. J. (2005). A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Evaluation and the Health Professions,28(2), 212–232. https://doi.org/10.1177/0163278705275342.
Brazier, J. E., Harper, R., Jones, N. M., O’Cathain, A., Thomas, K. J., Usherwood, T., et al. (1992). Validating the SF-36 health survey questionnaire: New outcome measure for primary care. BMJ,305(6846), 160–164.
Lim, L. L., Seubsman, S. A., & Sleigh, A. (2008). Thai SF-36 health survey: Tests of data quality, scaling assumptions, reliability and validity in healthy men and women. Health and Quality of Life Outcomes,6, 52. https://doi.org/10.1186/1477-7525-6-52.
Laosanguanek, N., Wiroteurairuang, T., Siritho, S., & Prayoonwiwat, N. (2011). Reliability of the Thai version of SF-36 questionnaire for an evaluation of quality of life in multiple sclerosis patients in multiple sclerosis clinic at Siriraj Hospital. Journal of the Medical Association of Thailand,94(Suppl 1), S84–S88.
Kamper, S. J., Ostelo, R. W., Knol, D. L., Maher, C. G., de Vet, H. C., & Hancock, M. J. (2010). Global Perceived Effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. Journal of Clinical Epidemiology,63(7), 760–766. https://doi.org/10.1016/j.jclinepi.2009.09.009.
Tavakol, M., & Dennick, R. (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education,2, 53–55. https://doi.org/10.5116/ijme.4dfb.8dfd.
Weir, J. P. (2005). Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. Journal of Strength and Conditioning Research,19(1), 231–240. https://doi.org/10.1519/15184.1.
Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine,15(2), 155–163. https://doi.org/10.1016/j.jcm.2016.02.012.
de Vet, H. C. W., Terwee, C. B., Knol, D. L., & Bouter, L. M. (2006). When to use agreement versus reliability measures. Journal of Clinical Epidemiology,59(10), 1033–1039. https://doi.org/10.1016/j.jclinepi.2005.10.015.
de Vet, H. C., Terwee, C. B., Ostelo, R. W., Beckerman, H., Knol, D. L., & Bouter, L. M. (2006). Minimal changes in health status questionnaires: Distinction between minimally detectable change and minimally important change. Health and Quality of Life Outcomes,4, 54. https://doi.org/10.1186/1477-7525-4-54.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling,6(1), 1–55.
MacCallum, R. C., Browne, M. W., & Sugawara, H. M. (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods,1(2), 130–149. https://doi.org/10.1037/1082-989X.1.2.130.
Terwee, C. B., Bot, S. D. M., de Boer, M. R., van der Windt, D. A. W. M., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology,60(1), 34–42. https://doi.org/10.1016/j.jclinepi.2006.03.012.
Cella, D., Riley, W., Stone, A., Rothrock, N., Reeve, B., Yount, S., et al. (2010). The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. Journal of Clinical Epidemiology,63(11), 1179–1194. https://doi.org/10.1016/j.jclinepi.2010.04.011.
Hung, M., Bounsanga, J., Voss, M. W., & Saltzman, C. L. (2018). Establishing minimum clinically important difference values for the patient-reported outcomes measurement information system physical function, hip disability and osteoarthritis outcome score for joint reconstruction, and knee injury and osteoarthritis outcome score for joint reconstruction in orthopaedics. World Journal of Orthopedics,9(3), 41–49. https://doi.org/10.5312/wjo.v9.i3.41.
Hung, M., Saltzman, C. L., Kendall, R., Bounsanga, J., Voss, M. W., Lawrence, B., et al. (2018). What are the MCIDs for PROMIS, NDI, and ODI instruments among patients with spinal conditions? Clinical Orthopaedics and Related Research,476(10), 2037–2039. https://doi.org/10.1097/Corr.0000000000000465.
Miles, J., & Shevlin, M. (2007). A time and a place for incremental fit indices. Personality and Individual Differences,42(5), 869–874. https://doi.org/10.1016/j.paid.2006.09.022.
Schreiber, J. B., Nora, A., Stage, F. K., Barlow, E. A., & King, J. (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. Journal of Educational Research,99(6), 323–337. https://doi.org/10.3200/Joer.99.6.323-338.
Kenney, R. J., Houck, J., Giordano, B. D., Baumhauer, J. F., Herbert, M., & Maloney, M. D. (2019). Do patient reported outcome measurement information system (PROMIS) scales demonstrate responsiveness as well as disease-specific scales in patients undergoing knee arthroscopy? American Journal of Sports Medicine,47(6), 1396–1403. https://doi.org/10.1177/0363546519832546.
Hung, M., Baumhauer, J. F., Brodsky, J. W., Cheng, C., Ellis, S. J., Franklin, J. D., et al. (2014). Psychometric comparison of the PROMIS physical function CAT with the FAAM and FFI for measuring patient-reported outcomes. Foot and Ankle International,35(6), 592–599. https://doi.org/10.1177/1071100714528492.
Hung, M., Saltzman, C. L., Greene, T., Voss, M. W., Bounsanga, J., Gu, Y., et al. (2018). Evaluating instrument responsiveness in joint function: The HOOS JR, the KOOS JR, and the PROMIS PF CAT. Journal of Orthopaedic Research,36(4), 1178–1184. https://doi.org/10.1002/jor.23739.
Brodke, D. S., Goz, V., Voss, M. W., Lawrence, B. D., Spiker, W. R., & Hung, M. (2017). PROMIS PF CAT outperforms the ODI and SF-36 physical function domain in spine patients. Spine (Phila Pa 1976),42(12), 921–929. https://doi.org/10.1097/brs.0000000000001965.
Funding
This study was funded by the 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund) [GCUGR1125614073M]. A scholarship from the Graduate School, Chulalongkorn University to commemorate the 72th anniversary of his Majesty King Bhumibol Adulyadej is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Table 7.
Rights and permissions
About this article
Cite this article
Rawang, P., Janwantanakul, P., Correia, H. et al. Cross-cultural adaptation, reliability, and construct validity of the Thai version of the Patient-Reported Outcomes Measurement Information System-29 in individuals with chronic low back pain. Qual Life Res 29, 793–803 (2020). https://doi.org/10.1007/s11136-019-02363-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-019-02363-x