Abstract
Background
Ultrasound (US) is used in the initial evaluation and surveillance of urinary tract dilation in children. Urinary tract dilation is diagnosed in 1–2% of all pregnancies during routine prenatal sonography with technological advances in US imaging. Urinary tract dilation classification systems, including the 2014 multidisciplinary consensus, assess anterior–posterior renal pelvic diameter and calyceal dilation. There is no consensus regarding optimal patient positioning — supine versus prone — during US assessment of urinary tract dilation.
Objective
We performed this study to determine whether there is a significant difference in the measurement of the anterior–posterior renal pelvic diameter, presence of calyceal dilation, or resulting urinary tract dilation consensus score obtained between supine and prone positions.
Materials and methods
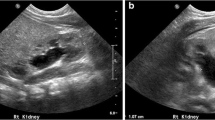
Two raters retrospectively reviewed renal bladder US exams of children with urinary tract dilation of one or both kidneys. We included technically adequate US examinations of orthotopic kidneys that were imaged in both supine and prone positions; we excluded children with renal anomalies or prior surgery. Anterior–posterior renal pelvic diameter measurements as well as central and peripheral calyceal dilation were documented in both supine and prone positions. A postnatal urinary tract dilation consensus score was assigned to each kidney based only on these features.
Results
Urinary tract dilation in either the supine or prone position was performed in 146 kidneys (69 right, 77 left) in 89 children. Median age was 0.26 years (interquartile ratio [IQR] 0.08–0.61 years). Female-to-male ratio was 1:3 (21/89). The interclass correlations of the anterior–posterior renal pelvic diameter were 0.88 and 0.87 in the supine and prone positions, respectively, without significant differences (P=0.1). When comparing all kidneys together, the mean anterior–posterior renal pelvic diameter was 7.1 mm (95% confidence interval [CI] 6.4–7.8) in supine and 7.9 (95% CI 7.1–8.7) in prone, with a mean difference between the measurements of 0.83 mm (95% CI 0.3–1.4; P=0.16). Central calyceal and peripheral calyceal dilation were more commonly found in the prone position versus the supine position in both kidneys. Central calyceal dilation was observed in 15 cases in the prone but not in the supine position. In one kidney, it was seen only in the supine but not in the prone position. Overall the urinary tract dilation score differed between positions in 10.3% (15/146) of cases, most of them (14/15) with a higher score in prone compared to the supine position.
Conclusion
Scanning in prone position tends to more frequently show calyceal dilation and a greater size of the anterior–posterior renal pelvic diameter, resulting in higher urinary tract dilation classification scores, with almost perfect interobserver agreement.



Similar content being viewed by others
References
Scoutt LM, Burns P, Brown JL et al (2000) Ultrasound evaluation of the urinary tract. In: Pollack HM (ed) Clinical urography, 2nd edn. W.B. Saunders, Philadelphia, pp 388–523
Nguyen HT, Benson CB, Bromley B et al (2014) Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol 10:982–998
Langer B, Simeoni U, Montoya Y et al (1996) Antenatal diagnosis of upper urinary tract dilation by ultrasonography. Fetal Diagn Ther 11:191–198
Ellenbogen PH, Scheible FW, Talner LB, Leopold GR (1978) Sensitivity of gray scale ultrasound in detecting urinary tract obstruction. AJR Am J Roentgenol 130:731–733
Grignon A, Filion R, Filiatrault D et al (1986) Urinary tract dilatation in utero: classification and clinical applications. Radiology 160:645–647
Fernbach SK, Maizels M, Conway JJ (1993) Ultrasound grading of hydronephrosis: introduction to the system used by the Society for Fetal Urology. Pediatr Radiol 23:478–480
Onen A (2007) An alternative grading system to refine the criteria for severity of hydronephrosis and optimal treatment guidelines in neonates with primary UPJ-type hydronephrosis. J Pediatr Urol 3:200–205
Riccabona M, Avni FE, Blickman JG et al (2008) Imaging recommendations in paediatric uroradiology: minutes of the ESPR workgroup session on urinary tract infection, fetal hydronephrosis, urinary tract ultrasonography and voiding cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol 38:138–145
Berdon WE, Baker DH, Leonidas J (1968) Advantages of prone positioning in gastrointestinal and genitourinary roentgenologic studies in infants and children. Am J Roentgenol Radium Therapy Nucl Med 103:444–455
Riggs W Jr, Hagood JH, Andrews AE (1970) Anatomic changes in the normal urinary tract betwen supine and prone urograms. Radiology 94:107–113
Fernbach SK, Bernfield JB (1990) Positional variation in the ultrasound appearance of the renal pelvis. Pediatr Radiol 21:45–47
Carrico CW, Zerin JM (1996) Sonographic measurement of renal length in children: does the position of the patient matter? Pediatr Radiol 26:553–555
De Sanctis JT, Connolly SA, Bramson RT (1998) Effect of patient position on sonographically measured renal length in neonates, infants, and children. AJR Am J Roentgenol 170:1381–1383
Nakamura M, Taniguchi N, Kawai F et al (2003) Sonographic measurement of renal length in children: variation associated with body position. J Med Ultrason 30:187–192
Sharma G, Sharma A, Maheshwari P (2012) Predictive value of decreased renal pelvis anteroposterior diameter in prone position for prenatally detected hydronephrosis. J Urol 187:1839–1843
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med 22:276–282
Schaeffer AJ, Kurtz MP, Logvinenko T et al (2016) MRI-based reference range for the renal pelvis anterior-posterior diameter in children ages 0-19 years. Br J Radiol 89:20160211
Rickard M, Easterbrook B, Kim S et al (2017) Six of one, half a dozen of the other: a measure of multidisciplinary inter/intra-rater reliability of the Society for Fetal Urology and urinary tract dilation grading systems for hydronephrosis. J Pediatr Urol 13:80.e1–80.e5
Back SJ, Christopher Edgar J et al (2018) Rater reliability of postnatal urinary tract dilation consensus classification. Pediatr Radiol 48:1606–1611
Nelson CP, Lee RS, Trout AT et al (2019) Interobserver and intra-observer reliability of the urinary tract dilation classification system in neonates: a multicenter study. J Urol 201:1186–1192
Chung EM, Soderlund KA, Fagen KE (2017) Imaging of the pediatric urinary system. Radiol Clin N Am 55:337–357
Nelson CP, Lee RS, Trout AT et al (2019) The association of postnatal urinary tract dilation risk score with clinical outcomes. J Pediatr Urol 19:30123–30128
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calle-Toro, J.S., Maya, C.L., Gorfu, Y. et al. Supine versus prone positioning for ultrasound evaluation of postnatal urinary tract dilation in children. Pediatr Radiol 50, 357–362 (2020). https://doi.org/10.1007/s00247-019-04546-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04546-7