Abstract
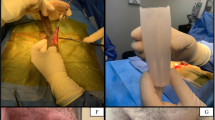
We have previously reported on the use of Tutoplast® cadaveric pericardium as an alternative material for grafting the tunica albugineal defect after Peyronie's plaque excision with satisfactory results in 11 patients. We now review long-term outcomes in this cohort of men. Eleven patients with significant penile curvature interfering with sexual intercourse were evaluated after at least 12 months of conservative therapy. All patients underwent pre-operative evaluation, including penile duplex Doppler ultrasound studies. Chemically processed and gamma-irradiated pericardium (Biodynamics International, Parsippany, NJ) was used to graft the cavernosal defect after surgical excision of the penile plaque. Three patients simultaneously underwent placement of penile prostheses secondary to documented erection problems identified at duplex Doppler ultrasound evaluation. The long-term postoperative complications and erectile function were evaluated with a mean follow-up of 30 months (range 25–35 months). All patients reported resolution of penile curvature allowing for normal sexual function after a mean follow-up of the first 14 months. Thirty months after placement of cadaveric pericardium, the three prosthetic patients still reported excellent sexual function. For the eight patients who did not undergo placement of a prosthesis, three with small to medium plaque size (<2×5 cm) continued to do well. The remaining five patients with a large plaque size (>2×5 cm) did well initially, but later reported difficulty maintaining erection due to venous leakage, thus they are currently using either a vacuum constriction device or an Actis ring. Three out of these five venous leakage patients had ventral plaques; two had dorsal plaques, one of significant size (4×5 cm). We conclude that for those patients who do not undergo placement of a prosthesis, a better long-term outcome is observed when the plaque is small to medium in size (<2×5 cm) and dorsally located. Patients with ventral plaque, extreme curvature, or plaque size >4×5 cm were more likely to have veno-occlusive dysfunction, necessitating further intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Carson CC. . Francois Gigot de la Peyronie (1678–1747). Invest Urol 1981 19, 62–63.
Levine LA. . Peyronie's disease: a difficult sexual dysfunction problem. West J Med 1998 169, 168–169.
Gelbard MK, Dorey F, James K. . The natural history of Peyronie's disease. J Urol 1990 144, 1376–1379.
Schwarzer U et al. Prevalence of Peyronie's disease: results of an 8000 men survey. J Urol 2000 163(Suppl), 742A.
Nooter RI, Bosch JLHR, Schroder FH. . Peyronie's disease and congenital penile curvature: long-term results of operative treatment with the plication procedure. Br J Urol 1994 74, 497–500.
Carson CC. . Peyronie's disease: medical and surgical management. In: Hellstrom WJG (ed). The Handbook of Sexual Dysfunction Allen Press: Lawrence, Kansas 1999 93–98.
Lamberge RJ, Bishop MC, Bailey CP. . Nesbit's operation for Peyronie's disease. Br J Urol 1984 56, 721–723.
Gholami SS, Goharderakhshan RZ, Lue TF. . Correction of penile curvature using minimal tension paired plications and papaverine: a review of 84 patients. J Urol 2000 163(Suppl), 993A.
Hicks CC et al. Experience with the Horton-Devine dermal graft in the treatment of Peyronie's disease. J Urol 1978 119, 504–506.
Fallon B. . Cadaveric dura mater graft for correction of penile curvature in Peyronie's disease. Urology 1990 35, 121–129.
Das S. . Peyronie's disease: excision and auotgrafting with tunica vaginalis. J Urol 1980 124, 818–819.
Brock G et al. Can a venous patch graft be substitute for the tunica albuginea of the penis? J Urol 1993 150, 1306–1309.
Teloken C et al. Penile straightening in Peyronie's disease with crural graft of the corpus cavernosum. J Urol 2000 163(Suppl), 991A.
Lowe DH et al. Surgical treatment of Peyronie's disease with dacron graft. Urology 1982 19, 609–610.
Bazeed MA et al. New surgical procedure for management of Peyronie's disease. Urology 1983 21, 501–504.
Ganabathi K et al. Peyronie's disease: surgical treatment based on penile rigidity. J Urol 1985 153, 662–666.
Nesbit RM. . Congenital curvature of the penis: a report of three cases with description of corrective operation. J Urol 1965 93, 230.
Yachia D. . Corporal plication for surgical correction of Peyronie's disease. J Urol 1993 149, 869.
Pryor JP, Fitzpatrick JM. . A new approach to the correction of the penile deformity in Peyronie's disease. J Urol 1979 122, 622–623.
Lue TF, El-Sakka AI. . Venous patch graft for Peyronie's disease. Part I: technique. J Urol 1998 160, 2047–2049.
El-Sakka AI, Rashwan HM, Lue TF. . Venous patch graft for Peyronie's disease. Part II: outcome analysis. J Urol 1998 160, 2050–2053.
Hellstrom WJG. . The use of prosthetic materials in the surgical management of Peyronie's disease. Int J Impot Res 1994 6, 32.
Hellstrom WJG, Reddy S. . Application of pericardial graft in the surgical treatment of Peyronie's disease. J Urol 2000 163, 1445–1447.
Raviv T et al. Pericardial patch grafts in glaucoma implant surgery. J Glaucoma 1998 7, 27–32.
Sibayan SA, Latina MA. . The use of processed pericardium in the repair of corneoscleral fistulas. Ophthalmic Surg Lasers 1997 28, 334–335.
Pesch HJ. . Solvent-preserved grafts of dura mater and fascia lata. Studies on their tissue tolerability in animals. In: Portman (ed). Facial Nerve Masson: New York 1985 506–511.
Leungwattanakij S, Bivalacqua TJ, Caufield JJ, Hellstrom WJG. . Evaluation of cadaveric pericardium in the rat for the surgical treatment of Peyronie's disease. Urology 2000 56, 1075–1080.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Leungwattanakij, S., Bivalacqua, T., Reddy, S. et al. Long-term follow-up on use of pericardial graft in the surgical management of Peyronie's disease. Int J Impot Res 13, 183–186 (2001). https://doi.org/10.1038/sj.ijir.3900676
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijir.3900676
Keywords
This article is cited by
-
Comparing Outcomes of Grafts Used in Peyronie’s Disease Surgery: a Systematic Review
Current Sexual Health Reports (2020)
-
Engineering of erectile tissue: the state and future of corporal restoration
World Journal of Urology (2020)
-
Bicentric prospective evaluation of corporoplasty with porcine small intestinal submucosa (SIS) in patients with severe Peyronie’s disease
World Journal of Urology (2017)
-
Surgery for Peyronie's disease
Asian Journal of Andrology (2013)
-
Peyronie’s surgery: Graft choices and outcomes
Current Urology Reports (2009)