Abstract
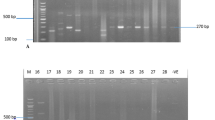
Glycopeptides, particularly the cell wall-acting antibiotic vancomycin, are the safest cure for methicillin-resistant Staphylococcus aureus. The aim of this study was to evaluate nonsusceptibility of clinical isolates of S. aureus to vancomycin and investigate mutations in vraSR, a cell wall synthesis regulator gene, in vancomycin-resistant strains. Susceptibility of 110 clinical strains of S. aureus to methicillin and vancomycin were determined using disc diffusion method and determination of minimum inhibitory concentration, respectively. Presence of mecA and vanA genes was determined by PCR. Determination of spa types and mutations of the vraSR gene in vancomycin nonsusceptible isolates were assessed by PCR-sequencing analyses. In total, 47 isolates (42.73%) were recognized as MRSA, three (2.73%) strains were resistant to vancomycin, and eight (7.27%) strains were vancomycin intermediates. The MIC of vancomycin was 4–64 μg/ml in these isolates. All vancomycin nonsusceptible S. aureus strains were mecA positive and one isolate was positive for the vanA gene. Spa type t030 was found as the most common type. In vraSR sequence analysis, all 11 vancomycin nonsusceptible isolates had the D59E mutation in the vraR and E45G in vraS genes. R117H, R121S, and R121I are the other identified missense mutations in the vraR gene. The identification of a high percentage of MRSA and presence of VRSA and VISA isolates is a serious warning about the treatment of future MRSA infections and reveals the need for new and effective therapeutic agents.

Similar content being viewed by others

References
Azimian A, Havaei SA, Fazeli H, Naderi M, Ghazvini K, Samiee SM, Soleimani M, Peerayeh SN (2012) Genetic characterization of a vancomycin-resistant Staphylococcus aureus isolate from the respiratory tract of a patient in a university hospital in northeastern Iran. J Clin Microbiol 50(11):3581–3585
Baseria N, Najar-Peerayeha S, Bagheri Amirib F (2018) Prevalence of vancomycin-intermediate Staphylococcus aureus among clinical isolates in Iran: a systematic review and meta-analysis. J Glob Antimicrob Resist 15:178–187
Boyle-Vavra S, Yin S, Daum RS (2006) The VraS/VraR two-component regulatory system required for oxacillin resistance in community-acquired methicillin-resistant Staphylococcus aureus. FEMS Microbiol Lett 262(2):163–171
Cui L, Neoh HM, Shoji M, Hiramatsu K (2009) Contribution of vraSR and graSR point mutations to vancomycin resistance in vancomycin-intermediate Staphylococcus aureus. Antimicrob Agents Chemother 53(3):1231–1234
Dadashi M, Nasiri MJ, Fallah F, Owlia P, Hajikhani B, Emaneini M, Mirpour M (2018) Methicillin-resistant Staphylococcus aureus (MRSA) in Iran: a systematic review and meta-analysis. J Glob Antimicrob Resist 12:96–103
Galbusera E, Renzoni A, Andrey DO, Monod A, Barras C, Tortora P, Polissi A, Kelley WL (2011) Site-specific mutation of Staphylococcus aureus VraS reveals a crucial role for the VraR-VraS sensor in the emergence of glycopeptide resistance. Antimicrob Agents Chemother 55(3):1008–1020
Gardete S, Wu SW, Gill S, Tomasz A (2006) Role of VraSR in antibiotic resistance and antibiotic-induced stress response in Staphylococcus aureus. Antimicrob Agents Chemother 50(10):3424–3434
Goetghebeur M, Landry PA, Han D, Vicente C (2007) Methicillin-resistant Staphylococcus aureus: a public health issue with economic consequences. Can J Infect Dis Med Microbiol 18(1):27–34
Hamdan-Partida A, Sainz-Espuñes T, Bustos-Martínez J (2010) Characterization and persistence of Staphylococcus aureus strains isolated from the anterior nares and throats of healthy carriers in a Mexican community. J Clin Microbiol 48(5):1701–1705
Hiramatsu K, Aritaka N, Hanaki H, Kawasaki S, Hosoda Y, Hori S, Fukuchi Y, Kobayashi I (1997) Dissemination in Japanese hospitals of strains of Staphylococcus aureus heterogeneously resistant to vancomycin. Lancet 350(9092):1670–1673
Hiramatsu K, Kayayama Y, Matsuo M, Aiba Y, Saito M, Hishinuma T, Iwamoto A (2014) Vancomycin-intermediate resistance in Staphylococcus aureus. J Glob Antimicrob Resist 2(4):213–224
Holden MT, Feil EJ, Lindsay JA, Peacock SJ, Day NP, Enright MC, Foster TJ, Moore CE, Hurst L, Atkin R, Barron A (2004) Complete genomes of two clinical Staphylococcus aureus strains: evidence for the rapid evolution of virulence and drug resistance. Proc Natl Acad Sci U S A 101(26):9786–9791
Howden BP, Davies JK, Johnson PD, Stinear TP, Grayson ML (2010) Reduced vancomycin susceptibility in Staphylococcus aureus, including vancomycin-intermediate and heterogeneous vancomycin-intermediate strains: resistance mechanisms, laboratory detection, and clinical implications. Clin Microbiol Rev 23(1):99–139
Kato Y, Suzuki T, Ida T, Maebashi K, Sakurai M, Shiotani J, Hayashi I (2008) Microbiological and clinical study of methicillin-resistant Staphylococcus aureus (MRSA) carrying VraS mutation: changes in susceptibility to glycopeptides and clinical significance. Int J Antimicrob Agents 31(1):64–70
Kuroda M, Kuroda H, Oshima T, Takeuchi F, Mori H, Hiramatsu K (2003) Two-component system VraSR positively modulates the regulation of cell-wall biosynthesis pathway in Staphylococcus aureus. Mol Microbiol 49(3):807–821
Leonard PG, Golemi-Kotra D, Stock AM (2013) Phosphorylation-dependent conformational changes and domain rearrangements in Staphylococcus aureus VraR activation. Proc Natl Acad Sci 110(21):8525–8530
McAleese F, Wu SW, Sieradzki K, Dunman P, Murphy E, Projan S, Tomasz A (2006) Overexpression of genes of the cell wall stimulon in clinical isolates of Staphylococcus aureus exhibiting vancomycin intermediate S. aureus type resistance to vancomycin. J Bacteriol 188(3):1120–1133
Moubareck C, Meziane-Cherif D, Patrice Courvalin P, Périchon B (2009) VanA-type Staphylococcus aureus strain VRSA-7 is partially dependent on vancomycin for growth. Antmicrob Agents Chemother 53(9):3657–3663
Najar-Peerayeh S, Mirzaee M, Behmanesh M (2016) Molecular characterization of vancomycin-intermediate Staphylococcus aureus isolates from Tehran. Asian Pac J Trop Dis 6(9):726–731
Paniagua-Contreras G, Sáinz-Espuñes T, Monroy-Pérez E, Rodríguez-Moctezuma JR, Arenas-Aranda D, Negrete-Abascal E et al (2012) Virulence markers in Staphylococcus aureus strains isolated from hemodialysis catheters of Mexican patients. Adv Microbiol 2(04):476–487
Périchon B, Courvalin P (2009) VanA-type vancomycin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 53(11):4580–4587
Robinson DA, Enright MC (2004) Multilocus sequence typing and the evolution of methicillin-resistant Staphylococcus aureus. Clin Microbiol Infect 10(2):92–97
Tiwari KB (2009) Vancomycin resistance in Staphylococcus aureus may occur faster than expected. Int J Life Sci 3
Worthington RJ, Blackledge MS, Melander C (2013) Small-molecule inhibition of bacterial two-component systems to combat antibiotic resistance and virulence. Future Med Chem 5(11):1265–1284
Yousefi M, Fallah F, Arshadi M, Pourmand MR, Hashemi A, Pourmand G (2017) Identification of tigecycline and vancomycin resistant Staphylococcus aureus strains among UTI patients in Iran. New Microbes New Infect 24:8–12
Acknowledgments
The authors are grateful to the Islamic Azad University, Rasht Branch, Rasht, Iran, for support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Asadpour, L., Ghazanfari, N. Detection of vancomycin nonsusceptible strains in clinical isolates of Staphylococcus aureus in northern Iran. Int Microbiol 22, 411–417 (2019). https://doi.org/10.1007/s10123-019-00063-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10123-019-00063-7