Abstract
Background and Aims
Bile is the only significant pathway for cholesterol elimination. Cholecystectomy (CS) increases fecal bile acid loss, and endoscopic biliary sphincterotomy (ES) is thought to have a similar effect. We speculated that a combined effect of ES + CS would further enhance fecal bile acid loss, potentially causing lipid profile changes in these patients.
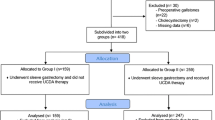
Methods
Fecal bile acids and sterols were determined using gas chromatography in cohorts of post-CS + ES, post-CS and in healthy controls. The effect of ES + CS on blood lipid profile was assessed retrospectively in a single-center cohort of post-CS + ES patients, using a computerized database. Parameters of interest included demographics, medical history, and lipid profiles.
Results
Fecal primary bile acid concentrations were increased after CS + ES compared to CS and controls (cholic acid [CA] 1.4 ng/mg vs. 0.26 ng/mg, p = 0.02 vs. 0.23 ng/mg, p = 0.004, chenodeoxycholic acid [CDCA] 1.92 ng/mg vs. 0.39 ng/mg, p = 0.02 vs. 0.23 ng/mg, p = 0.01, respectively). Fecal cholesterol excretion was similar in all three groups. Baseline serum lipid profile and subsequent changes following CS + ES were correlated. In patients with baseline hypercholesterolemia (total cholesterol (TC) > 200 mg/dl), TC levels decreased by 28.5 mg/dl, and LDL levels decreased by 21.5 mg/dl. The effect was more pronounced in those with TC > 200 mg/dl, despite of statin intake. In patients with hypertriglyceridemia [triglycerides (TG) > 200 mg/dl], TG decreased by 67.8 mg/dl following ES + CS. Among patients without dyslipidemia or dyslipidemia with adequate response to statins, the effect of ES + CS on lipid profile was minor.
Conclusions
Fecal bile acid loss increases following CS + ES. The effect on blood lipid profile depends on baseline TC and TG levels. Lipid profile is improved in dyslipidemic patients, while the impact of CS + ES is minimal on the normolipemic population.





Similar content being viewed by others
Abbreviations
- CA:
-
Cholic acid
- CDCA:
-
Chenodeoxycholic acid
- CS:
-
Cholecystectomy
- DCA:
-
Deoxycholic acid
- ES:
-
Endoscopic biliary sphincterotomy
- HDL:
-
High-density cholesterol
- LCA:
-
Lithocholic acid
- TBA:
-
Total bile acids
- TC:
-
Total blood cholesterol
- TG:
-
Triglycerides
- UDCA:
-
Ursodeoxycholic acid
References
Fort JM, Azpiroz F, Casellas F, et al. Bowel habits after cholecystectomy: physiological changes and clinical implications. Gastroenterology. 1996;111:617–622.
Breuer NF, Jaekel S, Dommes P, et al. Fecal bile acid excretion pattern in cholecystectomized patients. Dig Dis Sci. 1986;31:953–960 https://doi.org/10.1007/bf01303216
Fromm H, Tunuguntla AK, Malavolti M, et al. Absence of significant role of bile acids in diarrhea of heterogenous group of postcholecystectomy patients. Dig Dis Sci. 1987;32:33–44. https://doi.org/10.1007/bf01296685
Sauter GH, Moussavian AC, Meyer G, et al. Bowel habits and bile acid malabsorption in the months after cholecystectomy. Am J Gastroenterol. 2002;97:1732–1735.
Almond HR, Vlahcevic ZR, Bell CC, et al. Bile acid pools, kinetics and biliary lipid composition before and after cholecystectomy. N Engl J Med. 1973;289:1213–1216.
Berr F, Stellaard F, Pratschke E, et al. Effects of cholecystectomy on the kinetics of primary and secondary bile acids. J Clin Investig. 1989;83:1541–1550.
Kullak-Ublick GA, Paumgartner G, Berr F. Long term effects of cholecystectomy on bile acid metabolism. Hepatology. 1995;21:41–45.
Malik AA, Wani ML, Tak SI, et al. Association of dyslipidemia with cholilithiasis and effect of cholecystectomy on the same. Int J Surg. 2011;9:641–642.
Juvonen T, Kervinen K, Kairaluoma MI, et al. Effect of cholecystectomy on plasma lipid and lipoprotein levels. Hepatogastroenterology. 1995;42:377–382.
Sauerbruch T, Stellaard F, et al. Effect of endoscopic sphincterotomy on bile acid pool size and bile lipid composition in man. Digestion. 1983;27:87–92.
Alazmi WM, Fogel EL, Watkins JL, et al. The effects of biliary sphincterotomy on serum cholesterol levels in postcholecystectomy patients: a pilot study. Can J Gastroenterol. 2005;21:81–84.
Ung KA, Mottacki N, Rudling M, et al. Biliary sphincterotomy does not relate to diarrhea or major changes in bile acid synthesis or plasma lipids. Scand J Gastroenterol. 2009;44:1132–1138.
Batta AK, Salen G, Arora R, et al. Side chain conjugation prevents bacterial 7-dehydroxylation of bile acids. J Biol Chem. 1990;265:10925–10928.
Keren N, Konikoff FM, Paitan Y, et al. Interactions between the intestinal microbiota and bile acids in gallstones patients. Environ Microbiol Rep. 2015;7:874–880.
Soran H, Dent R, Dirrington P. Evidence-based goals in LDL-C reduction. Clin Res Cardiol. 2017;106:237–248.
Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115:450–458.
Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovasculardisease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk. 1996;3:213–219.
Catapano AL, Graham I, De Backer G, et al. ESC/EAS Guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37:2999–3058.
Denke MA, Frantz ID. Response to a cholesterol lowering diet: efficacy is greater in hypercholesterolemia subjects even after adjustment for regression to mean. Am J Med. 1993;94:626–631.
Clifton PM, Kestin M, Abbey M, et al. Relationship between sensitivity to dietary fat and dietary cholesterol. Arterioscler Thromb Vasc Biol. 1990;10:394–401.
Goldberg RB, Guyon JR, Mazone T, et al. Relationships between metabolic syndrome and other baseline factors and the efficacy of ezetimibe/simvastatin and atorvastatin in patients with type 2 diabetes and hypercholesterolemia. Diabetes Care. 2010;33:1021–1024.
Smiderle L, Lima LO, Hutz MH, et al. Evaluation of sexual dimorphism in the efficacy and safety of imvastatin/atorvastatin therapy in a southern Brazilian cohort. Arq Bras Cardiol. 2014;103:33–40.
Farnier M, Salko T, Isaacson JL, et al. Effects of baseline level of triglycerides on changes in lipid levels from combined fluvastatin + fibrate (bezafibrate, fenofibrate or gemfibrozil). Am J Cardiol. 2003;92:794–797.
Chen MM, Hale C, Stanislaus S, et al. FGF21 acts as a negative regulator of bile acid synthesis. J Endocrinol. 2018;237:139–152.
Inagaki T, Choi M, Moschetta A, et al. Fibroblast growth factor 15 functions as an enterohepatic signal to regulate bile acid homeostasis. Cell Metab. 2005;2:217–225.
Chiang JY. Bile acid metabolism and signaling. Compr Physiol. 2013;3:1191–1212.
Guo S, Li L, Yin H. Cholesterol homeostasis and liver X receptor (LXR) in atherosclerosis. Cardiovasc Hematol Disord Drug Targets. 2018;18:27–33.
Goodwin B, Watson MA, Kim H, et al. Differential regulation of rat and human CYP7A1 by the nuclear oxysterol receptor liver X receptor-alpha. Mol Endocrinol. 2003;17:386–394.
Lee SD, Tontonoz P. Liver X receptors at the intersection of lipid metabolism and atherogenesis. Atherosclerosis.. 2015;242:29–36.
Dergunov AD. Apolipoprotein E genotype as a most significant predictor of lipid response at lipid-lowering therapy: mechanistic and clinical studies. Biomed Pharmacother. 2011;65:597–603.
Brisson D, Ledoux K, Bosse Y, et al. Effect of apolipoprotein E, peroxisome proliferator-activated receptor alpha and lipoprotein lipase gene mutations on the ability of fenofibrate to improve lipid profiles and reach clinical guideline targets among hypertriglyceridemic patients. Pharmacogenetics. 2002;12:313–320.
Kriaa A, Bourgin M, Potiron A, et al. Microbial impact on cholesterol and bile acid metabolism: current status and future prospects. J Lipid Res. 2019;60:323–332.
Acknowledgments
We thank Professor Uri Gophna for his help with study concept and preparation.
Funding
This study was supported in part by the Josefina Maus and Gabriela Cesarman Chair for Research in Liver Diseases, Sackler Faculty of Medicine, Tel Aviv University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sergeev, I., Keren, N., Naftali, T. et al. Cholecystectomy and Biliary Sphincterotomy Increase Fecal Bile Loss and Improve Lipid Profile in Dyslipidemia. Dig Dis Sci 65, 1223–1230 (2020). https://doi.org/10.1007/s10620-019-05823-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05823-z