Abstract
Background
Metabolic information obtained through 18F-flurodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) is used to evaluate malignancy by calculating the glucose uptake rate, and these parameters play important roles in determining the prognosis of non-small cell lung cancer (NSCLC). The expression of immune-related markers in tumor tissue reflects the immune status in the tumor microenvironment. However, there is lack of reports on the association between metabolic variables and intra-tumor immune markers. Herein, we investigate the correlation between metabolic status on 18F-FDG PET/CT and intra-tumor immunomarkers’ expression in NSCLC patients.
Methods
From April 2008 to August 2014, 763 patients were enrolled in the analysis to investigate the role of maximum standardized uptake value (SUVmax) in lung cancer. One hundred twenty-two tumor specimens were analyzed by immunohistochemistry (IHC) to intra-tumor immune cells and programmed death protein ligand 1(PD-L1) expression on tumor cells. The correlation between metabolic variables and the expression of tissue immune markers were analyzed.
Results
SUVmax values have significant variations in different epidermal growth factor receptor (EGFR) statuses (wild type vs mutant type), high/low neutrophil-to-lymphocyte ratio (NLR) groups, and high/low platelets-to-lymphocyte ratio (PLR) groups (p < 0.001, p < 0.001, p = 0.003, respectively). SUVmax was an independent prognostic factor in lung cancer patients (p = 0.013). IHC demonstrated a statistically significant correlation between SUVmax and the expression of CD8 tumor-infiltrating lymphocytes (p = 0.015), CD163 tumor-associated macrophages (TAMs) (p = 0.003), and Foxp3-regulatory T cells (Tregs) (p = 0.004), as well as PD-1 and PD-L1 (p = 0.003 and p = 0.012, respectively). With respect to patient outcomes, disease stage, BMI, SUVmax, metabolic tumor volume (MTV), TLG (tumor lesion glycolysis), CD163-TAMs, CD11c-dendritic cells (DCs), PD-L1, and Tregs showed a statistically significant correlation with progression-free survival (PFS) (p < 0.001, 0.023, < 0.001, 0.007, 0.005, 0.004, 0.008, 0.048, and 0.014, respectively), and disease stage, SUVmax, MTV, TLG, CD163-TAMs, CD11c-DCs, and PD-L1 showed a statistically significant correlation with overall survival (OS) (p < 0.001, < 0.001, 0.014, 0.012, < 0.001, 0.001, and < 0.001, respectively).
Conclusion
This study revealed an association between metabolic variable and immune cell expression in the tumor microenvironment and suggests that SUVmax on 18F-FDG PET/CT could be a potential predictor for selecting candidates for immunotherapy.



Similar content being viewed by others
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- 18F-FDG PET/CT:
-
18F-Flurodeoxyglucose positron emission tomography/computed tomography
- TILs:
-
Tumor-infiltrating lymphocytes
- TAMs:
-
Tumor-associated macrophages
- Tregs:
-
Regulatory T cells
- DCs:
-
Dendritic cells
- PD-1:
-
Programmed death protein 1
- IHC:
-
Immunohistochemistry
- SUV:
-
Standardized uptake value
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- SCC:
-
Squamous cell carcinoma
- ADC:
-
Adenocarcinoma
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelets-to-lymphocyte ratio
- BMI:
-
Body mass index
References
Saintigny P, Burger JA. Recent advances in non-small cell lung cancer biology and clinical management. Discov Med. 2012;13:287–97.
Ashamalla H, Rafla S, Parikh K, Mokhtar B, Goswami G, Kambam S, et al. The contribution of integrated PET/CT to the evolving definition of treatment volumes in radiation treatment planning in lung cancer. Int J Radiat Oncol Biol Phys. 2005;63:1016–23. https://doi.org/10.1016/j.ijrobp.2005.04.021.
Mac MM, Hicks RJ. The role of positron emission tomography/computed tomography in radiation therapy planning for patients with lung cancer. Semin Nucl Med. 2012;42:308–19. https://doi.org/10.1053/j.semnuclmed.2012.04.003.
Opoka L, Szolkowska M, Podgajny Z, Kunikowska J, Baranska I, Blasinska-Przerwa K, et al. Assessment of recurrence of non-small cell lung cancer after therapy using CT and Integrated PET/CT. Pneumonol Alergol Pol. 2013;81:214–20.
Palsson-McDermott EM, O’Neill LA. The Warburg effect then and now: from cancer to inflammatory diseases. Bioessays. 2013;35:965–73. https://doi.org/10.1002/bies.201300084.
Appelberg R, Moreira D, Barreira-Silva P, Borges M, Silva L, Dinis-Oliveira RJ, et al. The Warburg effect in mycobacterial granulomas is dependent on the recruitment and activation of macrophages by interferon-gamma. Immunology. 2015;145:498–507. https://doi.org/10.1111/imm.12464.
Gajewski TF, Schreiber H, Fu YX. Innate and adaptive immune cells in the tumor microenvironment. Nat Immunol. 2013;14:1014–22. https://doi.org/10.1038/ni.2703.
Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309–22. https://doi.org/10.1016/j.ccr.2012.02.022.
Fridman WH, Pages F, Sautes-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12:298–306. https://doi.org/10.1038/nrc3245.
Dunn GP, Old LJ, Schreiber RD. The three Es of cancer immunoediting. Annu Rev Immunol. 2004;22:329–60. https://doi.org/10.1146/annurev.immunol.22.012703.104803.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39. https://doi.org/10.1056/NEJMoa1507643.
Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50. https://doi.org/10.1016/S0140-6736(15)01281-7.
Fehrenbacher L, Spira A, Ballinger M, Kowanetz M, Vansteenkiste J, Mazieres J, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387:1837–46. https://doi.org/10.1016/S0140-6736(16)00587-0.
Chang CH, Qiu J, O’Sullivan D, Buck MD, Noguchi T, Curtis JD, et al. Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell. 2015;162:1229–41. https://doi.org/10.1016/j.cell.2015.08.016.
Pearce EL, Pearce EJ. Metabolic pathways in immune cell activation and quiescence. Immunity. 2013;38:633–43. https://doi.org/10.1016/j.immuni.2013.04.005.
Na F, Wang J, Li C, Deng L, Xue J, Lu Y. Primary tumor standardized uptake value measured on F18-Fluorodeoxyglucose positron emission tomography is of prediction value for survival and local control in non-small-cell lung cancer receiving radiotherapy: meta-analysis. J Thorac Oncol. 2014;9:834–42. https://doi.org/10.1097/JTO.0000000000000185.
Nair VS, Krupitskaya Y, Gould MK. Positron emission tomography 18F-fluorodeoxyglucose uptake and prognosis in patients with surgically treated, stage I non-small cell lung cancer: a systematic review. J Thorac Oncol. 2009;4:1473–9. https://doi.org/10.1097/JTO.0b013e3181bccbc6.
Paesmans M, Berghmans T, Dusart M, Garcia C, Hossein-Foucher C, Lafitte JJ, et al. Primary tumor standardized uptake value measured on fluorodeoxyglucose positron emission tomography is of prognostic value for survival in non-small cell lung cancer: update of a systematic review and meta-analysis by the European Lung Cancer Working Party for the International Association for the Study of Lung Cancer Staging Project. J Thorac Oncol. 2010;5:612–9. https://doi.org/10.1097/JTO.0b013e3181d0a4f5.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–44. https://doi.org/10.1038/nature07205.
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106:u124. https://doi.org/10.1093/jnci/dju124.
Liu H, Wu Y, Wang Z, Yao Y, Chen F, Zhang H, et al. Pretreatment platelet-to-lymphocyte ratio (PLR) as a predictor of response to first-line platinum-based chemotherapy and prognosis for patients with non-small cell lung cancer. J Thorac Dis. 2013;5:783–9. https://doi.org/10.3978/j.issn.2072-1439.2013.12.34.
Kaya V, Yildirim M, Demirpence O, Yildiz M, Yalcin AY. Prognostic significance of basic laboratory methods in non- small-cell-lung cancer. Asian Pac J Cancer Prev. 2013;14:5473–6.
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30:1073–81. https://doi.org/10.1093/carcin/bgp127.
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357:539–45. https://doi.org/10.1016/S0140-6736(00)04046-0.
Elkord E, Alcantar-Orozco EM, Dovedi SJ, Tran DQ, Hawkins RE, Gilham DE. T regulatory cells in cancer: recent advances and therapeutic potential. Expert Opin Biol Ther. 2010;10:1573–86. https://doi.org/10.1517/14712598.2010.529126.
Na II, Byun BH, Kim KM, Cheon GJ, Choe DH, Koh JS, et al. 18F-FDG uptake and EGFR mutations in patients with non-small cell lung cancer: a single-institution retrospective analysis. Lung Cancer. 2010;67:76–80. https://doi.org/10.1016/j.lungcan.2009.03.010.
Mak RH, Digumarthy SR, Muzikansky A, Engelman JA, Shepard JA, Choi NC, et al. Role of 18F-fluorodeoxyglucose positron emission tomography in predicting epidermal growth factor receptor mutations in non-small cell lung cancer. Oncologist. 2011;16:319–26. https://doi.org/10.1634/theoncologist.2010-0300.
Higashi K, Ueda Y, Sakurai A, Mingwang X, Xu L, Murakami M, et al. Correlation of Glut-1 glucose transporter expression with [18F]FDG uptake in non-small cell lung cancer. Eur J Nucl Med. 2000;27(12):1778–85. https://doi.org/10.1007/s002590000367.
Wei T, Zhang J, Qin Y, Wu Y, Zhu L, Lu L, et al. Increased expression of immunosuppressive molecules on intratumoral and circulating regulatory T cells in non-small-cell lung cancer patients. Am J Cancer Res. 2015;5:2190–201.
Jayaraman P, Jacques MK, Zhu C, Steblenko KM, Stowell BL, Madi A, et al. TIM3 mediates t cell exhaustion during Mycobacterium tuberculosis infection. PLoS Pathog. 2016;12:e1005490. https://doi.org/10.1371/journal.ppat.1005490.
Liang B, Workman C, Lee J, Chew C, Dale BM, Colonna L, et al. Regulatory T cells inhibit dendritic cells by lymphocyte activation gene-3 engagement of MHC class II. J Immunol. 2008;180:5916–26.
Rabe H, Nordstrom I, Andersson K, Lundell AC, Rudin A. Staphylococcus aureus convert neonatal conventional CD4(+) T cells into FOXP3(+) CD25(+) CD127(low) T cells via the PD-1/PD-L1 axis. Immunology. 2014;141:467–81. https://doi.org/10.1111/imm.12209.
Hasegawa T, Suzuki H, Yamaura T, Muto S, Okabe N, Osugi J, et al. Prognostic value of peripheral and local forkhead box P3+ regulatory T cells in patients with non-small-cell lung cancer. Mol Clin Oncol. 2014;2:685–94. https://doi.org/10.3892/mco.2014.299.
Bille A, Okiror L, Skanjeti A, Errico L, Arena V, Penna D, et al. The prognostic significance of maximum standardized uptake value of primary tumor in surgically treated non-small-cell lung cancer patients: analysis of 413 cases. Clin Lung Cancer. 2013;14:149–56. https://doi.org/10.1016/j.cllc.2012.04.007.
Lopci E, Toschi L, Grizzi F, Rahal D, Olivari L, Castino GF, et al. Correlation of metabolic information on FDG-PET with tissue expression of immune markers in patients with non-small cell lung cancer (NSCLC) who are candidates for upfront surgery. Eur J Nucl Med Mol Imaging. 2016;43:1954–61. https://doi.org/10.1007/s00259-016-3425-2.
Fox CJ, Hammerman PS, Thompson CB. Fuel feeds function: energy metabolism and the T-cell response. Nat Rev Immunol. 2005;5:844–52. https://doi.org/10.1038/nri1710.
Jones RG, Thompson CB. Revving the engine: signal transduction fuels T cell activation. Immunity. 2007;27:173–8. https://doi.org/10.1016/j.immuni.2007.07.008.
van Bruggen R, Koker MY, Jansen M, van Houdt M, Roos D, Kuijpers TW, et al. Human NLRP3 inflammasome activation is Nox1–4 independent. Blood. 2010;115:5398–400. https://doi.org/10.1182/blood-2009-10-250803.
Zou W, Chen L. Inhibitory B7-family molecules in the tumour microenvironment. Nat Rev Immunol. 2008;8:467–77. https://doi.org/10.1038/nri2326.
Curiel TJ, Wei S, Dong H, Alvarez X, Cheng P, Mottram P, et al. Blockade of B7-H1 improves myeloid dendritic cell-mediated antitumor immunity. Nat Med. 2003;9:562–7. https://doi.org/10.1038/nm863.
Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192:1027–34.
Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149:274–93. https://doi.org/10.1016/j.cell.2012.03.017.
Spranger S, Koblish HK, Horton B, Scherle PA, Newton R, Gajewski TF. Mechanism of tumor rejection with doublets of CTLA-4, PD-1/PD-L1, or IDO blockade involves restored IL-2 production and proliferation of CD8(+) T cells directly within the tumor microenvironment. J Immunother Cancer. 2014;2:3. https://doi.org/10.1186/2051-1426-2-3.
Funding
This work was supported by National Natural Science Funds of China (Nos. 81401887 and 81401888).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent and ethics statement
Informed consent was obtained from all individual participants included in the study. Written informed obtained from each subject complies with the Declaration of Helsinki. The study was approved by the Ethical Committee of TMUCHI.
Confirmation statement
My study’s involvement with human subjects complies with the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology – Chest
Electronic supplementary material
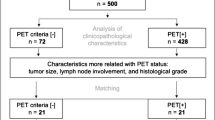
Supplementary Figure 1
(PNG 33 kb)
Supplementary Figure 2
(PNG 25 kb)
Supplementary Figure 3
(PNG 84 kb)
Supplementary Figure 4
(PNG 54 kb)
Supplementary Figure 5
(PNG 58 kb)
Supplementary Figure 6
(PNG 74 kb)
ESM 1
(DOC 52 kb)
Rights and permissions
About this article
Cite this article
Wang, Y., Zhao, N., Wu, Z. et al. New insight on the correlation of metabolic status on 18F-FDG PET/CT with immune marker expression in patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging 47, 1127–1136 (2020). https://doi.org/10.1007/s00259-019-04500-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04500-7