Abstract
Purpose
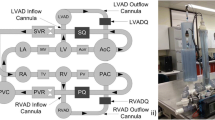
This study compares preload sensitivity of continuous flow (CF) VAD support to counterpulsation using the Windmill toroidal VAD (TORVAD). The TORVAD is a two-piston rotary pump that ejects 30 mL in early diastole, which increases cardiac output while preserving aortic valve flow.
Methods
Preload sensitivity was compared for CF vs. TORVAD counterpulse support using two lumped parameter models of the cardiovascular system: (1) an open-loop model of the systemic circulation was used to obtain ventricular function curves by isolating the systemic circulation and prescribing preload and afterload boundary conditions, and (2) a closed-loop model was used to test the physiological response to changes in pulmonary vascular resistance, systemic vascular resistance, heart rate, inotropic state, and blood volume. In the open-loop model, ventricular function curves (cardiac output vs left ventricular preload) are used to assess preload sensitivity. In the closed-loop model, left ventricular end systolic volume is used to assess the risk of left ventricular suction.
Results
At low preloads of 5 mmHg, CF support overpumps the circulation compared to TORVAD counterpulse support (cardiac output of 3.3 L/min for the healthy heart, 4.7 with CF support, and 3.5 with TORVAD counterpulse support) and has much less sensitivity than counterpulse support (0.342 L/min/mmHg for the healthy heart, 0.092 with CF support, and 0.306 with TORVAD counterpulse support). In the closed-loop model, when PVR is increased beyond 0.035 mmHg s/mL, CF support overpumps the circulation and causes ventricular suction events, but TORVAD counterpulse support maintains sufficient ventricular volume and does not cause suction.
Conclusions
Counterpulse support with the TORVAD preserves aortic valve flow and provides physiological sensitivity across all preload conditions. This should prevent overpumping and minimize the risk of suction.






Similar content being viewed by others
References
AlOmari, A.-H. H., A. V. Savkin, M. Stevens, D. G. Mason, D. L. Timms, R. F. Salamonsen, et al. Developments in control systems for rotary left ventricular assist devices for heart failure patients: a review. Physiol. Meas. 34(1):R1–R27, 2013.
Bakouri, M. A., R. F. Salamonsen, A. V. Savkin, A. H. H. Alomari, E. Lim, and N. H. Lovell. A sliding mode-based starling-like controller for implantable rotary blood pumps. Artif. Organs 38(7):587–593, 2014.
Baumwol, J., P. S. MacDonald, A. M. Keogh, E. Kotlyar, P. Spratt, P. Jansz, et al. Right heart failure and “failure to thrive” after left ventricular assist device: clinical predictors and outcomes. J. Heart Lung Transpl. 30(8):888–895, 2011.
Berlin, D. A., and J. Bakker. Starling curves and central venous pressure. Crit. Care 19(1):55, 2014.
Burkhoff, D. Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. AJP Heart Circ. Physiol. 289(2):H501–H512, 2005.
Cleveland, J. C., D. C. Naftel, T. B. Reece, M. Murray, J. Antaki, F. D. Pagani, et al. Survival after biventricular assist device implantation: an analysis of the Interagency registry for mechanically assisted circulatory support database. J. Heart Lung Transpl. 30(8):863–869, 2011.
Conover, T., A. M. Hlavacek, F. Migliavacca, E. Kung, A. Dorfman, R. S. Figliola, et al. An interactive simulation tool for patient-specific clinical decision support in single-ventricle physiology. J. Thorac. Cardiovasc. Surg. 155(2):712–721, 2017.
Doshi, D., and D. Burkhoff. Cardiovascular simulation of heart failure pathophysiology and therapeutics. J. Card Fail. 22(4):303–311, 2016.
Fried, J., A. R. Garan, S. Shames, A. Masoumi, M. Yuzefpolskaya, K. Takeda, et al. Aortic root thrombosis in patients supported with continuous-flow left ventricular assist devices. J. Heart Lung Transpl. 37(12):1425–1432, 2018.
Fukamachi, K., A. Shiose, A. Massiello, D. J. Horvath, L. A. R. Golding, S. Lee, et al. Preload sensitivity in cardiac assist devices. Ann. Thorac. Surg. 95(1):373–380, 2013.
Gaddum, N. R., M. Stevens, E. Lim, J. Fraser, N. Lovell, D. Mason, et al. Starling-like flow control of a left ventricular assist device: in vitro validation. Artif. Organs 38(3):E46–E56, 2014.
Gohean, J. R., M. J. George, K. W. Chang, E. R. Larson, T. D. Pate, M. Kurusz, et al. Preservation of native aortic valve flow and full hemodynamic support with the TORVAD using a computational model of the cardiovascular system. ASAIO J. 61(3):259–265, 2015.
Gohean, J. R., M. J. George, T. D. Pate, M. Kurusz, R. G. Longoria, and R. W. Smalling. Verification of a computational cardiovascular system model comparing the hemodynamics of a continuous flow to a synchronous valveless pulsatile flow left ventricular assist device. Asaio J. 59(2):107–116, 2013.
Guyton, A. C. Circulatory physiology: Cardiac output and its regulation (1st ed.). Philadelphia: W.B. Saunders Company, 1963.
Hardy, H. H., and R. E. Collins. On the pressure-volume relationship in circulatory elements. Med. Biol. Eng. Comput. 20(5):565–570, 1982.
Horn, M., W. Hooper, B. Brach, W. Ashburn, and K. Moser. Postural changes in pulmonary blood flow in pulmonary hypertension: a noninvasive technique using ventilation-perfusion scans. Circulation 66(3):621–627, 1982.
Houston, B. A., R. J. Kalathiya, S. Hsu, R. Loungani, M. E. Davis, S. T. Coffin, et al. Right ventricular afterload sensitivity dramatically increases after left ventricular assist device implantation: a multi-center hemodynamic analysis. J. Heart Lung Transpl. 35(7):868–876, 2016.
Khalil, H. A., W. E. Cohn, R. W. Metcalfe, and O. H. Frazier. Preload sensitivity of the Jarvik 2000 and HeartMate II left ventricular assist devices. ASAIO J. 54(3):245–248, 2008.
Kirklin, J. K., F. D. Pagani, R. L. Kormos, L. W. Stevenson, E. D. Blume, S. L. Myers, et al. Eighth annual INTERMACS report: special focus on framing the impact of adverse events. J. Heart Lung Transpl. 36(10):1080–1086, 2017.
Klotz, S., M. L. Dickstein, and D. Burkhoff. A computational method of prediction of the end-diastolic pressure–volume relationship by single beat. Nat. Protoc. 2(9):2152–2158, 2007.
Korakianitis, T., and Y. Shi. A concentrated parameter model for the human cardiovascular system including heart valve dynamics and atrioventricular interaction. Med. Eng. Phys. 28(7):613–628, 2006.
Letsou, G. V., T. D. Pate, J. R. Gohean, M. Kurusz, R. G. Longoria, L. Kaiser, et al. Improved left ventricular unloading and circulatory support with synchronized pulsatile left ventricular assistance compared with continuous-flow left ventricular assistance in an acute porcine left ventricular failure model. J. Thorac. Cardiovasc. Surg. 140(5):1181–1188, 2010.
Lim, H. S., N. Howell, and A. Ranasinghe. The physiology of continuous-flow left ventricular assist devices. J. Card Fail. 23(2):169–180, 2017.
May-Newman, K., Y. K. Wong, R. Adamson, P. Hoagland, V. Vu, and W. Dembitsky. Thromboembolism is linked to intraventricular flow stasis in a patient supported with a left ventricle assist device. ASAIO J. 59(4):452–455, 2013.
Patterson, S. W., and E. H. Starling. On the mechanical factors which determine the output of the ventricles. J. Physiol. 48(5):357–379, 1914.
Pauls, J. P., M. C. Stevens, N. Bartnikowski, J. F. Fraser, S. D. Gregory, and G. Tansley. Evaluation of physiological control systems for rotary left ventricular assist devices: an in-vitro study. Ann. Biomed. Eng. 44(8):1–11, 2016.
Pauls, J. P., M. C. Stevens, N. Bartnikowski, J. F. Fraser, S. D. Gregory, and G. Tansley. Evaluation of physiological control systems for rotary left ventricular assist devices: an in vitro study. Ann. Biomed. Eng. 44(8):2377–2387, 2016.
Pauls, J. P., M. C. Stevens, E. Schummy, G. Tansley, J. F. Fraser, D. Timms, et al. In vitro comparison of active and passive physiological control systems for biventricular assist devices. Ann. Biomed. Eng. 44(5):1370–1380, 2016.
Salamonsen, R. F., E. Lim, N. Gaddum, A. H. H. Alomari, S. D. Gregory, M. Stevens, et al. Theoretical foundations of a starling-like controller for rotary blood pumps. Artif. Organs 36(9):787–796, 2012.
Salamonsen, R. F., D. G. Mason, and P. J. Ayre. Response of rotary blood pumps to changes in preload and afterload at a fixed speed setting are unphysiological when compared with the natural heart. Artif. Organs 35(3):E47–E53, 2011.
Slaughter, M. S., F. D. Pagani, J. G. Rogers, L. W. Miller, B. Sun, S. D. Russell, et al. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J. Heart Lung Transpl. 29(4 Suppl):S1–S39, 2010.
Stevens MC, Gaddum NR, Pearcy M, Salamonsen RF, Timms DL, Mason DG, et al. Frank-starling control of a left ventricular assist device. In: Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, 2011, pp. 1335–1338.
Stevens, M. C., S. Wilson, A. Bradley, J. Fraser, and D. Timms. Physiological control of dual rotary pumps as a biventricular assist device using a master/slave approach. Artif. Organs 38(9):766–774, 2014.
Suga, H., and K. Sagawa. Instantaneous pressure volume relationships and their ratio in the excised, supported canine left ventricle. Circ. Res. 35(1):117–126, 1974.
Tchantchaleishvili, V., J. G. Y. Luc, C. M. Cohan, K. Phan, L. Hübbert, S. W. Day, et al. Clinical implications of physiologic flow adjustment in continuous-flow left ventricular assist devices. ASAIO J. 63(3):241–250, 2017.
Walley, K. R. Left ventricular function: Time-varying elastance and left ventricular aortic coupling [Internet]. Crit. Care 20:1–11, 2016.
Warriner, D. R., A. G. Brown, S. Varma, P. J. Sheridan, P. Lawford, D. R. Hose, et al. Closing the loop: modelling of heart failure progression from health to end-stage using a meta-analysis of left ventricular pressure-volume loops. PLoS ONE 9(12):1–19, 2014.
Zhong, L., D. N. Ghista, E. Y. K. Ng, and S. T. Lim. Passive and active ventricular elastances of the left ventricle. Biomed. Eng. Online 4:1–13, 2005.
Funding
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health (NIH) under award No. R44HL117446.
Conflict of interest
All authors have equity interests in Windmill. JG and EL are employees of Windmill, RL and MK consult with Windmill, and RS receives no financial support other than travel reimbursement.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Ajit P. Yoganathan oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Brief details of the cardiovascular system lumped parameter are provided here. This model is based on previously published work.12,13 Lumped parameter models of the systemic and pulmonary vessels contain two energy storage elements (representing vessel compliance \(C\) and fluid inertance \(L\)), and one passive element (representing viscous fluid resistance \(R\)).
Energy storage elements can be represented by differential equations, which can be integrated over time to simulate the dynamics of the cardiovascular system. The equation for the rate of change of pressure (\(P\)) is a function of the compliance (\(C\)) and the flow in (\(Q_{i}\)) and out (\(Q_{o}\)) of the vessel.
When fluid inertance elements are present in the model, the differential equation for flow in the element (\(Q\)) is a function of the viscous resistance (\(R\)), inertance of the fluid in the tube (\(L\)), and the pressure at the inlet (\(P_{i}\)) and outlet (\(P_{o}\)).
When inertial effects are neglected and there is only a passive resistance between two independent pressures, the flow becomes a dependent variable.
The volume in the atria and ventricles are modeled following the conservation of mass principle.
And the heart valves are represented as ideal diodes with a nonlinear orifice model,
Pressure in the atria and ventricle are defined by active and passive pressures, which are functions of volume that are modulated by the normalized time varying elastance function \(e\left( t \right)\).34,38
The passive pressure (\(P_{p}\)) is also known as the end diastolic pressure volume relationship (EDPVR) and represents the passive elastance of the ventricle during diastole when the ventricle is not contracting and has been modeled several ways. Some studies have opted for a simple linear relationship described by a minimum ventricular elastance, which is clearly not physiologic but may suffice for simulation studies over a very limited range of ventricular preloads.21,37 Logarithmic models have also been proposed to define an initial stiffness at the unstressed volume as well as an asymptotic maximum volume determined by the pericardium and cardiac cytoskeleton.15,36 Most computational models in the literature use exponential relationship.5,20 Exponential coefficients are derived from passive filling curves obtained from excised hearts of human and animals. These curves have been shown to represent the nonlinear aspect of filling relatively well and account for increased stiffness at higher filling volumes.
The approach taken in this study makes use of principles from all models above by superimposing an exponential and linear function.7
In this way, one extra term is added to the typical exponential model so that the stiffness (\(S_{0}\)) at the unstressed volume (\(V_{0}\)) can be controlled as it is done in the logarithmic model. This can be seen by determining the slope of the curve by evaluating the derivative with respect to volume at the unstressed volume.
To parameterize the passive pressure, the exponential constant (\(\alpha\)) is defined as well as the stiffness (\(S_{0}\)) at the unstressed volume. Then a single operating point through which the passive pressure curve should pass is defined (\(P_{op}\) and \(V_{op}\)). From these, the coefficient \(r\) can be found by
Table A1 provides values for healthy and heart failure conditions.
The active pressure (\(P_{a}\)) is also known as the end systolic pressure volume relationship (ESPVR) and is assumed to be a linear function of volume with a maximum elastance \(E_{m}\)
The model is parameterized for healthy and heart failure conditions using values described in previous publications.12,13 The ordinary differential equations (ODEs) that represent the time rate of change of the energy storage elements in the model are numerically integrated using an ODE solver in Matlab.
Rights and permissions
About this article
Cite this article
Gohean, J.R., Larson, E.R., Longoria, R.G. et al. Preload Sensitivity with TORVAD Counterpulse Support Prevents Suction and Overpumping. Cardiovasc Eng Tech 10, 520–530 (2019). https://doi.org/10.1007/s13239-019-00419-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-019-00419-0