Abstract
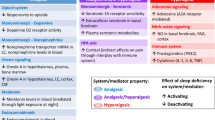
Sleep disturbances and chronic pain are considered public health concerns. They are frequently associated, and the direction of its relationship and possible mechanisms underlying it are frequently debated. The exploration of the sleep–pain association is of great clinical interest to explore in order to steer potential therapeutic avenues, accommodate the patient’s experience, and adapt the common practice of health professionals. In this review, the direction between sleep–pain in adult and pediatric populations will be discussed. Moreover, the possible mechanisms contributing to this relationship as endogenous pain modulation, inflammation, affect, mood and other states, the role of different endogenous substances (dopamine, orexin, melatonin, vitamin D) as well as other lesser known such as cyclic alternating pattern among others, will be explored. Finally, directions for future studies on this area will be discussed, opening up to the addition of tools such as brain imaging (e.g., fMRI), electrophysiology and non-invasive brain stimulation techniques. Such resources paired with artificial intelligence are key to personalized medicine management for patients facing pain and sleep interacting conditions.


Similar content being viewed by others
Abbreviations
- IL-6:
-
Interleukin 6
- CRP:
-
C-reactive protein
- NAc:
-
Nucleus accumbens
- A2A:
-
Adenosine 2 receptor
- PAG:
-
Periaqueductal gray
- EEG:
-
Electroencephalogram
- EMG:
-
Electromyogram
- 25OHD:
-
25-Hydroxyvitamin D
References
Adams RJ, Appleton SL, Taylor AW et al (2017) Sleep health of Australian adults in 2016: results of the 2016 Sleep Health Foundation national survey. Sleep Health 3(1):35–42
Afolalu EF, Ramlee F, Tang NKY (2018) Effects of sleep changes on pain-related health outcomes in the general population: a systematic review of longitudinal studies with exploratory meta-analysis. Sleep Med Rev 39:82–97
Andersen ML, Araujo P, Frange C, Tufik S (2018) Sleep disturbance and pain: a tale of two common problems. Chest 154(5):1249–1259
Arendt-Nielsen L, Sluka KA, Nie HL (2008) Experimental muscle pain impairs descending inhibition. Pain 140(3):465–471
Arewasikporn A, Ehde DM, Alschuler KN, Turner AP, Jensen MP (2018) Positive factors, pain, and function in adults with multiple sclerosis. Rehabil Psychol 63(4):612–620
Banno M, Harada Y, Taniguchi M et al (2018) Exercise can improve sleep quality: a systematic review and meta-analysis. PeerJ 6:e5172
Bastuji H, Perchet C, Legrain V, Montes C, Garcia-Larrea L (2008) Laser evoked responses to painful stimulation persist during sleep and predict subsequent arousals. Pain 137(3):589–599
Bentley AJ, Newton S, Zio CD (2003) Sensitivity of sleep stages to painful thermal stimuli. J Sleep Res 12(2):143–147
Bergman P, Sperneder S, Hoijer J, Bergqvist J, Bjorkhem-Bergman L (2015) Low vitamin D levels are associated with higher opioid dose in palliative cancer patients—results from an observational study in Sweden. PLoS One 10(5):e0128223
Besedovsky L, Lange T, Haack M (2019) The sleep-immune crosstalk in health and disease. Physiol Rev 99(3):1325–1380
Bishop TM, Ashrafioun L, Pigeon WR (2018) The association between sleep apnea and suicidal thought and behavior: an analysis of national survey data. J Clin Psychiatry 79(1):17m11480
Boakye PA, Olechowski C, Rashiq S et al (2016) A critical review of neurobiological factors involved in the interactions between chronic pain, depression, and sleep disruption. Clin J Pain 32(4):327–336
Bonvanie IJ, Oldehinkel AJ, Rosmalen JG, Janssens KA (2016) Sleep problems and pain: a longitudinal cohort study in emerging adults. Pain 157(4):957–963
Born J, Lange T, Hansen K, Molle M, Fehm HL (1997) Effects of sleep and circadian rhythm on human circulating immune cells. J Immunol 158(9):4454–4464
Buenaver LF, Quartana PJ, Grace EG et al (2012) Evidence for indirect effects of pain catastrophizing on clinical pain among myofascial temporomandibular disorder participants: the mediating role of sleep disturbance. Pain 153(6):1159–1166
Burgess HJ, Burns JW, Buvanendran A et al (2019) Associations between sleep disturbance and chronic pain intensity and function: a test of direct and indirect pathways. Clin J Pain 35:569–576
Cady RJ, Denson JE, Sullivan LQ, Durham PL (2014) Dual orexin receptor antagonist 12 inhibits expression of proteins in neurons and glia implicated in peripheral and central sensitization. Neuroscience 269:79–92
Cappuccio FP, Taggart FM, Kandala NB et al (2008) Meta-analysis of short sleep duration and obesity in children and adults. Sleep 31(5):619–626
Carra MC, Rompre PH, Kato T et al (2011) Sleep bruxism and sleep arousal: an experimental challenge to assess the role of cyclic alternating pattern. J Oral Rehabil 38(9):635–642
Caumo W, Hidalgo MP, Souza A, Torres ILS, Antunes LC (2019) Melatonin is a biomarker of circadian dysregulation and is correlated with major depression and fibromyalgia symptom severity. J Pain Res 12:545–556
Chae CU, Lee RT, Rifai N, Ridker PM (2001) Blood pressure and inflammation in apparently healthy men. Hypertension 38(3):399–403
Chokroverty S (2010) Overview of sleep and sleep disorders. Indian J Med Res 131:126–140
Chouchou F, Chauny JM, Rainville P, Lavigne GJ (2015) Selective REM sleep deprivation improves expectation-related placebo analgesia. PLoS One [Electron Resour] 10(12):e0144992
Chouchou F, Dang-Vu TT, Rainville P, Lavigne G (2018) The role of sleep in learning placebo effects. Int Rev Neurobiol 139:321–355
Danilov A, Kurganova J (2016) Melatonin in chronic pain syndromes. Pain Ther 5(1):1–17
de Oliveira DL, Hirotsu C, Tufik S, Andersen ML (2017) The interfaces between vitamin D, sleep and pain. J Endocrinol 234(1):R23–R36
Dinges DF, Pack F, Williams K et al (1997) Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep 20(4):267–277
Dinh ST, Nickel MM, Tiemann L et al (2019) Brain dysfunction in chronic pain patients assessed by resting-state electroencephalography. Pain 1:595470
Dubrovsky B, Janal MN, Lavigne GJ et al (2017) Depressive symptoms account for differences between self-reported versus polysomnographic assessment of sleep quality in women with myofascial TMD. J Oral Rehabil 44(12):925–933
Duenas M, Ojeda B, Salazar A, Mico JA, Failde I (2016) A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res 9:457–467
Dunietz GL, Swanson LM, Jansen EC et al (2018) Key insomnia symptoms and incident pain in older adults: direct and mediated pathways through depression and anxiety. Sleep 41(9):309
Edwards RR (2005) Individual differences in endogenous pain modulation as a risk factor for chronic pain. Neurology 65(3):437–443
Edwards RR, Grace E, Peterson S, Klick B, Haythornthwaite JA, Smith MT (2009) Sleep continuity and architecture: associations with pain-inhibitory processes in patients with temporomandibular joint disorder. Eur J Pain 13(10):1043–1047
Eichhorn N, Treede RD, Schuh-Hofer S (2018) The role of sex in sleep deprivation related changes of nociception and conditioned pain modulation. Neuroscience 387:191–200
Evans S, Djilas V, Seidman LC, Zeltzer LK, Tsao JCI (2017) Sleep quality, affect, pain, and disability in children with chronic pain: is affect a mediator or moderator? J Pain 18(9):1087–1095
Everson CA (1993) Sustained sleep deprivation impairs host defense. Am J Physiol 265(5 Pt 2):R1148–R1154
Faraut B, Leger D, Medkour T et al (2015) Napping reverses increased pain sensitivity due to sleep restriction. PLoS One [Electron Resour] 10(2):e0117425
Fatima Y, Doi SA, Mamun AA (2016) Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev 17(11):1154–1166
Finan PH, Garland EL (2015) The role of positive affect in pain and its treatment. Clin J Pain 31(2):177–187
Finan PH, Remeniuk B (2016) Is the brain reward system a mechanism of the association of sleep and pain? Pain Manag 6(1):5–8
Finan PH, Goodin BR, Smith MT (2013) The association of sleep and pain: an update and a path forward. J Pain 14(12):1539–1552
Finan PH, Buenaver LF, Coryell VT, Smith MT (2014) Cognitive-behavioral therapy for comorbid insomnia and chronic pain. Sleep Med Clin 9(2):261–274
Finan PH, Quartana PJ, Remeniuk B et al (2017) Partial sleep deprivation attenuates the positive affective system: effects across multiple measurement modalities. Sleep 40(1):zsw017
Fisher K, Laikin AM, Sharp KMH, Criddle CA, Palermo TM, Karlson CW (2018) Temporal relationship between daily pain and actigraphy sleep patterns in pediatric sickle cell disease. J Behav Med 41(3):416–422
Frase L, Selhausen P, Krone L et al (2019) Differential effects of bifrontal tDCS on arousal and sleep duration in insomnia patients and healthy controls. Brain Stimul 12(3):674–683
Gangwisch JE, Heymsfield SB, Boden-Albala B et al (2007) Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep 30(12):1667–1673
Gaskin DJ, Richard P (2012) The economic costs of pain in the United States. J Pain 13(8):715–724
Generaal E, Vogelzangs N, Penninx BW, Dekker J (2017) Insomnia, sleep duration, depressive symptoms, and the onset of chronic multisite musculoskeletal pain. Sleep 40(1):zsw030
Gonzalez-Ortiz M, Martinez-Abundis E, Balcazar-Munoz BR, Pascoe-Gonzalez S (2000) Effect of sleep deprivation on insulin sensitivity and cortisol concentration in healthy subjects. Diabetes Nutr Metab 13(2):80–83
Goodin BR, Smith MT, Quinn NB, King CD, McGuire L (2012) Poor sleep quality and exaggerated salivary cortisol reactivity to the cold pressor task predict greater acute pain severity in a non-clinical sample. Biol Psychol 91(1):36–41
Gotter AL, Webber AL, Coleman PJ, Renger JJ, Winrow CJ (2012) International Union of Basic and Clinical Pharmacology. LXXXVI. Orexin receptor function, nomenclature and pharmacology. Pharmacol Rev 64(3):389–420
Grill JD, Coghill RC (2002) Transient analgesia evoked by noxious stimulus offset. J Neurophysiol 87(4):2205–2208
Haack M, Scott-Sutherland J, Santangelo G, Simpson NS, Sethna N, Mullington JM (2012) Pain sensitivity and modulation in primary insomnia. Eur J Pain 16(4):522–533
Haack M, Simpson N, Sethna N, Kaur S, Mullington J (2019) Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology. https://doi.org/10.1038/s41386-019-0439-z
Herrero Babiloni A, Guay S, Nixdorf DR, de Beaumont L, Lavigne G (2018a) Non-invasive brain stimulation in chronic orofacial pain: a systematic review. J Pain Res 11:1445–1457
Herrero Babiloni A, De Beaumont L, Lavigne GJ (2018b) Transcranial magnetic stimulation: potential use in obstructive sleep apnea and sleep bruxism. Sleep Med Clin 13(4):571–582
Herrero JF, Laird JM, Lopez-Garcia JA (2000) Wind-up of spinal cord neurones and pain sensation: much ado about something? Prog Neurobiol 61(2):169–203
Hillman DR, Lack LC (2013) Public health implications of sleep loss: the community burden. Med J Aust 199(8):S7–10
Hillman D, Mitchell S, Streatfeild J, Burns C, Bruck D, Pezzullo L (2018) The economic cost of inadequate sleep. Sleep 41(8):zsy083
Holick MF (2004) Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80(6 Suppl):1678S–1688S
Hong S, Mills PJ, Loredo JS, Adler KA, Dimsdale JE (2005) The association between interleukin-6, sleep, and demographic characteristics. Brain Behav Immun 19(2):165–172
Huang CT, Chiang RP, Chen CL, Tsai YJ (2014) Sleep deprivation aggravates median nerve injury-induced neuropathic pain and enhances microglial activation by suppressing melatonin secretion. Sleep 37(9):1513–1523
Huang Z, Li Y, Bianchi MT et al (2018) Repetitive transcranial magnetic stimulation of the right parietal cortex for comorbid generalized anxiety disorder and insomnia: a randomized, double-blind, sham-controlled pilot study. Brain Stimul 11(5):1103–1109
International Pain Summit of the International Association for the Study of P (2011) Declaration of Montreal: declaration that access to pain management is a fundamental human right. J Pain Palliat Care Pharmacother 25(1):29–31
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80(1):40–52
Janssen SA (2002) Negative affect and sensitization to pain. Scand J Psychol 43(2):131–137
Jodoin M, Rouleau D, Larson-Dupuis C, Gosselin N, De Beaumont L (2017) The clinical utility of repetitive transcranial magnetic stimulation in reducing the risks of transitioning from acute to chronic pain in traumatically injured patients. Prog Neuropsychopharmacol Biol Psychiatry. 87(Pt B):322–331. https://doi.org/10.1016/j.pnpbp.2017.07.005
Karmann AJ, Lauer C, Ziegler E, Killian L, Horn-Hofmann C, Lautenbacher S (2018) Associations of nocturnal sleep with experimental pain and pain catastrophizing in healthy volunteers. Biol Psychol 135:1–7
Kaur T, Shyu BC (2018) Melatonin: a new-generation therapy for reducing chronic pain and improving sleep disorder-related pain. Adv Exp Med Biol 1099:229–251
Kichline T, Cushing CC, Ortega A, Friesen C, Schurman JV (2019) Associations between physical activity and chronic pain severity in youth with chronic abdominal pain. Clin J Pain 35:618–624
Killgore WD, Balkin TJ, Wesensten NJ (2006) Impaired decision making following 49 h of sleep deprivation. J Sleep Res 15(1):7–13
Klyne DM, Moseley GL, Sterling M, Barbe MF, Hodges PW (2018) Individual variation in pain sensitivity and conditioned pain modulation in acute low back pain: effect of stimulus type, sleep, and psychological and lifestyle factors. J Pain 19(8):942 e941–942 e918
Knutson KL, Spiegel K, Penev P, Van Cauter E (2007) The metabolic consequences of sleep deprivation. Sleep Med Rev 11(3):163–178
Koffel EA, Koffel JB, Gehrman PR (2015) A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Med Rev 19:6–16
Konjarski M, Murray G, Lee VV, Jackson ML (2018) Reciprocal relationships between daily sleep and mood: a systematic review of naturalistic prospective studies. Sleep Med Rev 42:47–58
Kothari DJ, Davis MC, Yeung EW, Tennen HA (2015) Positive affect and pain: mediators of the within-day relation linking sleep quality to activity interference in fibromyalgia. Pain 156(3):540–546
Krause AJ, Prather AA, Wager TD, Lindquist MA, Walker MP (2019) The pain of sleep loss: a brain characterization in humans. J Neurosci 39(12):2291–2300
Landry GJ, Best JR, Liu-Ambrose T (2015) Measuring sleep quality in older adults: a comparison using subjective and objective methods. Front Aging Neurosci 7:166
Larsen JT, Hershfield HE, Stastny BJ, Hester N (2017) On the relationship between positive and negative affect: their correlation and their co-occurrence. Emotion 17(2):323–336
Lautenbacher S (2018) Sleep and pain are definitely coupled-but how tight is this coupling? Pain 159(1):3–4
Lautenbacher S, Kundermann B, Krieg JC (2006) Sleep deprivation and pain perception. Sleep Med Rev 10(5):357–369
Laverdure-Dupont D, Rainville P, Renancio C, Montplaisir J, Lavigne G (2018) Placebo analgesia persists during sleep: an experimental study. Prog Neuropsychopharmacol Biol Psychiatry 85:33–38
Lavigne GJ, Sessle BJ (2016) The neurobiology of orofacial pain and sleep and their interactions. J Dent Res 95:1109–1116
Lavigne G, Zucconi M, Castronovo C, Manzini C, Marchettini P, Smirne S (2000) Sleep arousal response to experimental thermal stimulation during sleep in human subjects free of pain and sleep problems. Pain 84(2–3):283–290
Lee MA, Walker RW, Hildreth TJ, Prentice WM (2006) A survey of pain in idiopathic Parkinson’s disease. J Pain Symptom Manag 32(5):462–469
Lee YC, Lu B, Edwards RR et al (2013) The role of sleep problems in central pain processing in rheumatoid arthritis. Arthritis Rheum 65(1):59–68
Lewandowski Holley A, Rabbitts J, Zhou C, Durkin L, Palermo TM (2017) Temporal daily associations among sleep and pain in treatment-seeking youth with acute musculoskeletal pain. J Behav Med 40(4):675–681
Lewis GN, Rice DA, McNair PJ (2012) Conditioned pain modulation in populations with chronic pain: a systematic review and meta-analysis. J Pain 13(10):936–944
Ligato D, Petersen KK, Morch CD, Arendt-Nielsen L (2018) Offset analgesia: the role of peripheral and central mechanisms. Eur J Pain 22(1):142–149
Liguori C, Izzi F, Mercuri NB et al (2017) Vitamin D status of male OSAS patients improved after long-term CPAP treatment mainly in obese subjects. Sleep Med 29:81–85
Liu JW, Tu YK, Lai YF et al (2019) Associations between sleep disturbances and suicidal ideation, plans, and attempts in adolescents: a systematic review and meta-analysis. Sleep 42:zsz054
Lotsch J, Ultsch A (2018) Machine learning in pain research. Pain 159(4):623–630
Marshansky S, Mayer P, Rizzo D, Baltzan M, Denis R, Lavigne GJ (2018) Sleep, chronic pain, and opioid risk for apnea. Prog Neuropsychopharmacol Biol Psychiatry 87(Pt B):234–244
Mathias JL, Cant ML, Burke ALJ (2018) Sleep disturbances and sleep disorders in adults living with chronic pain: a meta-analysis. Sleep Med 52:198–210
Matre D, Andersen MR, Knardahl S, Nilsen KB (2016) Conditioned pain modulation is not decreased after partial sleep restriction. Eur J Pain 20(3):408–416
Mazza S, Magnin M, Bastuji H (2012) Pain and sleep: from reaction to action. Neurophysiol Clin 42(5):337–344
McCrae CS, Williams J, Roditi D et al (2018) Cognitive behavioral treatments for insomnia (CBT-I) and pain (CBT-P) in adults with comorbid chronic insomnia and fibromyalgia: clinical outcomes from the SPIN randomized controlled trial. Sleep 14:1595–1603
Melzack R (1990) Phantom limbs and the concept of a neuromatrix. Trends Neurosci 13(3):88–92
Moana-Filho EJ, Herrero Babiloni A (2018) Endogenous pain modulation in chronic temporomandibular disorders: Derivation of pain modulation profiles and assessment of its relationship with clinical characteristics. J Oral Rehabil 46(3):219–232. https://doi.org/10.1111/joor.12745
Moana-Filho EJ, Herrero Babiloni A, Theis-Mahon NR (2018) Endogenous pain modulation in chronic orofacial pain: a systematic review and meta-analysis. Pain 159(8):1441–1455
Moana-Filho EJ, Herrero Babiloni A, Nisley A (2019) Endogenous pain modulation assessed with offset analgesia is not impaired in chronic temporomandibular disorder pain patients. J Oral Rehabil. https://doi.org/10.1111/joor.12832
Moradi M, Yazdanian M, Haghparast A (2015) Role of dopamine D2-like receptors within the ventral tegmental area and nucleus accumbens in antinociception induced by lateral hypothalamus stimulation. Behav Brain Res 292:508–514
Mullington JM, Simpson NS, Meier-Ewert HK, Haack M (2010) Sleep loss and inflammation. Best Pract Res Clin Endocrinol Metab 24(5):775–784
Ng KY, Leong MK, Liang H, Paxinos G (2017) Melatonin receptors: distribution in mammalian brain and their respective putative functions. Brain Struct Funct 222(7):2921–2939
Niesters M, Hoitsma E, Sarton E, Aarts L, Dahan A (2011) Offset analgesia in neuropathic pain patients and effect of treatment with morphine and ketamine. Anesthesiology 115(5):1063–1071
Nir RR, Yarnitsky D (2015) Conditioned pain modulation. Curr Opin Support Palliat Care 9(2):131–137
O’Brien AT, Deitos A, Trinanes Pego Y, Fregni F, Carrillo-de-la-Pena MT (2018) Defective endogenous pain modulation in fibromyalgia: a meta-analysis of temporal summation and conditioned pain modulation paradigms. J Pain 19(8):819–836
O’Connell NE, Marston L, Spencer S, DeSouza LH, Wand BM (2018) Non-invasive brain stimulation techniques for chronic pain. Cochrane Database Syst Rev 3:CD008208
Ogilvie RD (2001) The process of falling asleep. Sleep Med Rev 5(3):247–270
Parrino L, Boselli M, Spaggiari MC, Smerieri A, Terzano MG (1998) Cyclic alternating pattern (CAP) in normal sleep: polysomnographic parameters in different age groups. Electroencephalogr Clin Neurophysiol 107(6):439–450
Parrino L, Ferri R, Bruni O, Terzano MG (2012) Cyclic alternating pattern (CAP): the marker of sleep instability. Sleep Med Rev 16(1):27–45
Parrino L, Grassi A, Milioli G (2014) Cyclic alternating pattern in polysomnography: what is it and what does it mean? Curr Opin Pulm Med 20(6):533–541
Paul-Savoie E, Marchand S, Morin M et al (2012) Is the deficit in pain inhibition in fibromyalgia influenced by sleep impairments? Open Rheumatol J 6:296–302
Peter-Derex L, Magnin M, Bastuji H (2015) Heterogeneity of arousals in human sleep: a stereo-electroencephalographic study. Neuroimage 123:229–244
Pigeon WR, Pinquart M, Conner K (2012) Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry 73(9):e1160–e1167
Price DD (2000) Psychological and neural mechanisms of the affective dimension of pain. Science 288(5472):1769–1772
Price DD, Hu JW, Dubner R, Gracely RH (1977) Peripheral suppression of first pain and central summation of second pain evoked by noxious heat pulses. Pain 3(1):57–68
Quartana PJ, Campbell CM, Edwards RR (2009) Pain catastrophizing: a critical review. Expert Rev Neurother 9(5):745–758
Rabbitts JA, Zhou C, Narayanan A, Palermo TM (2017) Longitudinal and temporal associations between daily pain and sleep patterns after major pediatric surgery. J Pain 18(6):656–663
Racine M (2018) Chronic pain and suicide risk: a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry 87(Pt B):269–280
Ravyts SG, Dzierzewski JM, Raldiris T, Perez E (2018) Sleep and pain interference in individuals with chronic pain in mid- to late-life: the influence of negative and positive affect. J Sleep Res 1:e12807
Razavi BM, Hosseinzadeh H (2017) A review of the role of orexin system in pain modulation. Biomed Pharmacother 90:187–193
Redwine L, Hauger RL, Gillin JC, Irwin M (2000) Effects of sleep and sleep deprivation on interleukin-6, growth hormone, cortisol, and melatonin levels in humans. J Clin Endocrinol Metab 85(10):3597–3603
Ree A, Nilsen KB, Knardahl S, Sand T, Matre D (2019) Sleep restriction does not potentiate nocebo-induced changes in pain and cortical potentials. Eur J Pain. https://doi.org/10.1002/ejp.1466
Rizzi M, Sarzi-Puttini P, Atzeni F et al (2004) Cyclic alternating pattern: a new marker of sleep alteration in patients with fibromyalgia? J Rheumatol 31(6):1193–1199
Rizzi M, Radovanovic D, Santus P et al (2017) Influence of autonomic nervous system dysfunction in the genesis of sleep disorders in fibromyalgia patients. Clin Exp Rheumatol 35 Suppl 105(3):74–80
Roohbakhsh A, Alavi MS, Azhdari-Zarmehri H (2018) The orexinergic (hypocretin) system and nociception: an update to supraspinal mechanisms. Curr Med Chem 25(32):3917–3929
Salas RE, Galea JM, Gamaldo AA et al (2014) Increased use-dependent plasticity in chronic insomnia. Sleep 37(3):535–544
Sardi NF, Lazzarim MK, Guilhen VA et al (2018a) Chronic sleep restriction increases pain sensitivity over time in a periaqueductal gray and nucleus accumbens dependent manner. Neuropharmacology 139:52–60
Sardi NF, Tobaldini G, Morais RN, Fischer L (2018b) Nucleus accumbens mediates the pronociceptive effect of sleep deprivation: the role of adenosine A2A and dopamine D2 receptors. Pain 159(1):75–84
Sauvet F, Leftheriotis G, Gomez-Merino D et al (2010) Effect of acute sleep deprivation on vascular function in healthy subjects. J Appl Physiol 108(1):68–75
Schuh-Hofer S, Wodarski R, Pfau DB et al (2013) One night of total sleep deprivation promotes a state of generalized hyperalgesia: a surrogate pain model to study the relationship of insomnia and pain. Pain 154(9):1613–1621
Schuh-Hofer S, Baumgartner U, Treede RD (2015) Effect of sleep deprivation on the electrophysiological signature of habituation to noxious laser stimuli. Eur J Pain 19(8):1197–1209
Schuh-Hofer S, Eichhorn N, Grinevich V, Treede RD (2018) Sleep deprivation related changes of plasma oxytocin in males and female contraceptive users depend on sex and correlate differentially with anxiety and pain hypersensitivity. Front Behav Neurosci 12:161
Schwartz N, Temkin P, Jurado S et al (2014) Chronic pain. Decreased motivation during chronic pain requires long-term depression in the nucleus accumbens. Science 345(6196):535–542
Seminowicz DA, Remeniuk B, Krimmel SR et al (2019) Pain-related nucleus accumbens function: modulation by reward and sleep disruption. Pain 160(5):1196–1207
Shahin M, Ahmed B, Hamida ST, Mulaffer FL, Glos M, Penzel T (2017) Deep learning and insomnia: assisting clinicians with their diagnosis. IEEE J Biomed Health Inform 21(6):1546–1553
Shi L, Chen SJ, Ma MY et al (2018) Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev 40:4–16
Shipton EA, Shipton EE (2015) Vitamin D and pain: vitamin D and its role in the aetiology and maintenance of chronic pain states and associated comorbidities. Pain Res Treat 2015:904967
Siegel JM (2005) Clues to the functions of mammalian sleep. Nature 437(7063):1264–1271
Siegel JM (2011) REM sleep: a biological and psychological paradox. Sleep Med Rev 15(3):139–142
Simpson N, Dinges DF (2007) Sleep and inflammation. Nutr Rev 65(12 Pt 2):S244–S252
Simpson NS, Scott-Sutherland J, Gautam S, Sethna N, Haack M (2018) Chronic exposure to insufficient sleep alters processes of pain habituation and sensitization. Pain 159(1):33–40
Smith BW, Zautra AJ (2008) Vulnerability and resilience in women with arthritis: test of a two-factor model. J Consult Clin Psychol 76(5):799–810
Smith MT, Edwards RR, McCann UD, Haythornthwaite JA (2007) The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep 30(4):494–505
Smith MT Jr, Remeniuk B, Finan PH et al (2019) Sex differences in measures of central sensitization and pain sensitivity to experimental sleep disruption: implications for sex differences in chronic pain. Sleep 42(2):zsy209
Staud R (2012) Abnormal endogenous pain modulation is a shared characteristic of many chronic pain conditions. Expert Rev Neurother 12(5):577–585
Taylor AM, Becker S, Schweinhardt P, Cahill C (2016) Mesolimbic dopamine signaling in acute and chronic pain: implications for motivation, analgesia, and addiction. Pain 157(6):1194–1198
Tiede W, Magerl W, Baumgartner U, Durrer B, Ehlert U, Treede RD (2010) Sleep restriction attenuates amplitudes and attentional modulation of pain-related evoked potentials, but augments pain ratings in healthy volunteers. Pain 148(1):36–42
Treede RD (2018) The International Association for the Study of Pain definition of pain: as valid in 2018 as in 1979, but in need of regularly updated footnotes. Pain Rep 3(2):e643
Treede RD, Rief W, Barke A et al (2015) A classification of chronic pain for ICD-11. Pain 156(6):1003–1007
Treede RD, Rief W, Barke A et al (2019) Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 160(1):19–27
Turk DC, Fillingim RB, Ohrbach R, Patel KV (2016) Assessment of psychosocial and functional impact of chronic pain. J Pain 17(9 Suppl):T21–T49
Valeriani M (2015) Increased habituation to painful stimuli: a self-protective mechanism during prolonged wakefulness? Eur J Pain 19(8):1055–1056
Valrie CR, Bromberg MH, Palermo T, Schanberg LE (2013) A systematic review of sleep in pediatric pain populations. J Dev Behav Pediatr JDBP 34(2):120–128
Valrie CR, Kilpatrick RL, Alston K et al (2019) Investigating the sleep-pain relationship in youth with sickle cell utilizing mHealth technology. J Pediatr Psychol 44(3):323–332
Venner A, Todd WD, Fraigne J et al (2019) Newly identified sleep-wake and circadian circuits as potential therapeutic targets. Sleep 42(5):zsz023
Vgontzas AN, Papanicolaou DA, Bixler EO et al (1999) Circadian interleukin-6 secretion and quantity and depth of sleep. J Clin Endocrinol Metab 84(8):2603–2607
Volkow ND, Tomasi D, Wang GJ et al (2012) Evidence that sleep deprivation downregulates dopamine D2R in ventral striatum in the human brain. J Neurosci 32(19):6711–6717
von Kanel R, Muller-Hartmannsgruber V, Kokinogenis G, Egloff N (2014) Vitamin D and central hypersensitivity in patients with chronic pain. Pain Med 15(9):1609–1618
Walker MP, Stickgold R (2006) Sleep, memory, and plasticity. Annu Rev Psychol 57:139–166
Watkins LR, Milligan ED, Maier SF (2003) Glial proinflammatory cytokines mediate exaggerated pain states: implications for clinical pain. Adv Exp Med Biol 521:1–21
Web statement on pain management guidance (2019) https://www.who.int/medicines/areas/quality_safety/guide_on_pain/en/. Accessed 24 Aug 2019
Whibley D, AlKandari N, Kristensen K et al (2019) Sleep and pain: a systematic review of studies of mediation. Clin J Pain 20:S19–S20
Wiech K, Tracey I (2009) The influence of negative emotions on pain: behavioral effects and neural mechanisms. Neuroimage 47(3):987–994
Williams AC, Craig KD (2016) Updating the definition of pain. Pain 157(11):2420–2423
Wilt JA, Davin S, Scheman J (2016) A multilevel path model analysis of the relations between sleep, pain, and pain catastrophizing in chronic pain rehabilitation patients. Scand J Pain 10:122–129
Wood PB, Patterson JC 2nd, Sunderland JJ, Tainter KH, Glabus MF, Lilien DL (2007) Reduced presynaptic dopamine activity in fibromyalgia syndrome demonstrated with positron emission tomography: a pilot study. J Pain 8(1):51–58
Woolf CJ (2010) What is this thing called pain? J Clin Investig 120(11):3742–3744
Wu YL, Chang LY, Lee HC, Fang SC, Tsai PS (2017) Sleep disturbances in fibromyalgia: a meta-analysis of case–control studies. J Psychosom Res 96:89–97
Wu Z, Malihi Z, Stewart AW, Lawes CM, Scragg R (2018) The association between vitamin D concentration and pain: a systematic review and meta-analysis. Public Health Nutr 21(11):2022–2037
Yarnitsky D (2015) Role of endogenous pain modulation in chronic pain mechanisms and treatment. Pain 156(Suppl 1):S24–S31
Yarnitsky D, Granot M, Granovsky Y (2014) Pain modulation profile and pain therapy: between pro- and antinociception. Pain 155(4):663–665
Yin J, Jin X, Shan Z et al (2017) Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose–response meta-analysis of prospective cohort studies. J Am Heart Assoc 6(9):e005947
Zhai L, Zhang H, Zhang D (2015) Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety 32(9):664–670
Zhang JM, An J (2007) Cytokines, inflammation, and pain. Int Anesthesiol Clin 45(2):27–37
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Herrero Babiloni, A., De Koninck, B.P., Beetz, G. et al. Sleep and pain: recent insights, mechanisms, and future directions in the investigation of this relationship. J Neural Transm 127, 647–660 (2020). https://doi.org/10.1007/s00702-019-02067-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-019-02067-z