Abstract
Background
Much data about prescription adherence in patients with heart failure (HF) are available, but few exist about the evaluation of true patient adherence. Further, methods for analyzing this issue are poorly known.
Objectives
Our objective was to evaluate the impact of patient adherence to disease-modifying drugs after HF hospitalization in a community-based cohort.
Methods and Results
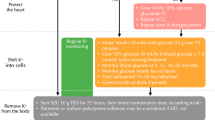
Patients hospitalized with first diagnostic HF code and at least one post-discharge purchase of evidence-based drugs for HF between 2009 and 2015 were included (12,938 patients). A new method for measuring adherence to polypharmacy (patient adherence indicator [PAI]) was introduced, based on proportion of days covered (PDC) and medication possession ratio (MPR). The investigated drugs were β-blockers (BBs), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin-receptor blockers (ARBs), and anti-aldosterone agents (AAs). Regional administrative databases were analyzed.
Results
The mean age of the cohort was 80 years; 53% was female; the median Charlson Comorbidity Index score was 2, and the overall death rate was 60%. PAI based on PDC estimated a nonadherence rate of 47%. Median daily dosages were well below target dosages for all drugs considered. A good PAI significantly lowered the mortality risk, irrespective of the computational method used: PDC (PAI adjusted hazard ratio [HR] 0.93; 95% confidence interval [CI] 0.88–0.97; p = 0.001) or MPR (PAI adjusted HR 0.93; 95% CI 0.89–0.98; p = 0.004).
Conclusions
In a real-world setting, medication adherence of patients with HF remains unsatisfactory, especially when in a polypharmacy setting. Irrespective of PDC and MPR, good patient adherence to polypharmacy was associated with a lower death rate.





Similar content being viewed by others
References
Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J, American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:948–54.
MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet. 1999;353:2001–7.
Kalogeropoulos AP, Samman-Tahhan A, Hedley JS, McCue AA, Bjork JB, Markham DW, Bhatt KN, Georgiopoulou VV, Smith AL, Butler J. Progression to stage D heart failure among outpatients with stage C heart failure and reduced ejection fraction. JACC Heart Fail. 2017;5:528–37.
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez‐Sanchez MA, Jaarsma T, Køber L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Rønnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2012;14:803–69.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos G, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016;134:e282–93.
Cohen‐Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole‐Wilson PA, Stromberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10(10):933–89.
Qin X, Hung J, Knuiman M, Teng TK, Briffa T, Sanfilippo FM. Evidence-based pharmacotherapies used in the postdischarge phase are associated with improved one-year survival in senior patients hospitalized with heart failure. Cardiovasc Ther. 2018;20:e12464.
Gayat E, Arrigo M, Littnerova S, Sato N, Parenica J, Ishihara S, Spinar J, Müller C, Harjola VP, Lassus J, Miró Ò, Maggioni AP, AlHabib KF, Choi DJ, Park JJ, Zhang Y, Zhang J, Januzzi JL Jr, Kajimoto K, Cohen-Solal A, Mebazaa A. GREAT Network. Heart failure oral therapies at discharge are associated with better outcome in acute heart failure: a propensity-score matched study. Eur J Heart Fail. 2018;20:345–54.
Yoo BS, Oh J, Hong BK, Shin DH, Bae JH,Yang DH, Shim WJ, Kim HS, Kim SH, Choi JO, Chun WJ, Go CW, Kang HJ, Baek SH, Cho JH, Hong SK, Shin JH, Oh SK, Pyun WB, Kwan J, Hong YJ, Jeong JO, Kang SM, Choi DJ, On behalf of the SUGAR Study. Survey of guideline adherence for treatment of systolic heart failure in real world (SUGAR): a multi-center, retrospective, observational study. PLoS One. 2014;9:e86596.
Komajda M, Cowie MR, Tavazzi L, Ponikowski P, Anker SD, Filippatos GS. QUALIFY Investigators. Physicians’ guideline adherence is associated with better prognosis in outpatients with heart failure with reduced ejection fraction: the QUALIFY international registry. Eur J Heart Fail. 2017;19:1414–23.
Komajda M, Anker SD, Cowie MR, Filippatos GS, Mengelle B, Ponikowski P, Tavazzi L. QUALIFY Investigators. Physicians’ adherence to guideline-recommended medications in heart failure with reduced ejection fraction: data from the QUALIFY global survey. Eur J Heart Fail. 2016;18:514–22.
Karve S, Cleve MA, Helm M, Hudson TJ, West DS, Martin BC. Prospective validation of eight different adherence measures for use with administrative claims data among patients with schizophrenia. Value Health. 2009;25:2303–10.
Andrade SE, Kahler KH, Frech F, Chan FA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15:565–74.
Arnet I, Greenland M, Knuiman MW, Rankin JM, Hung J, Nedkoff L, Briffa TG, Sanfilippo FM. Operationalization and validation of a novel method to calculate adherence to polypharmacy with refill data from the australian pharmaceutical benefits scheme (Pbs) database. Clin Epidemiol. 2018;10:1181–94.
Forbes CA, Deshpande S, Sorio-Vilela F, Kutikova L, Duffy S, Gouni-Berthold I, Hagström E. A systematic literature review comparing methods for the measurement of patient persistence and adherence. Curr Med Res Opin. 2018;34(9):1613–25.
Giardini A, Martin MT, Cahir C, et al. Toward appropriate criteria in medication adherence assessment in older persons: position paper. Aging Clin Exp Res. 2016;28:371–81.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Gasperoni F, Ieva F, Barbati G, Scagnetto A, Iorio A, Sinagra G, Di Lenarda A. Multi-state modelling of heart failure care path: a population-based investigation from Italy. PLoS One. 2017;12:1–15.
AIFA—Agenzia Italiana del Farmaco. Banca Dati Farmaci, Ricerca per Principio Attivo. https://farmaci.agenziafarmaco.gov.it/bancadatifarmaci/cerca-per-principio-attivo. Accessed 8 Sept 2018.
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, Dobbels F, Fargher E, Morrison V, Lewek P, Matyjaszczyk M, Mshelia C, Clyne W, Aronson JK, Urquhart J, ABC Project Team. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705.
R Core Team. R: a language and environment for statistical computing; 2015. Available from: https://www.R-project.org/.
Therneau T. A package for survival analysis in S. 2015. Version 2.38; 2015. Available from: https://CRAN.R-project.org/package=survival.
Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. Berlin: Springer Science & Business Media; 2000.
Maggioni AP, Anker SD, Dahlström U, Filippatos G, Ponikowski P, Zannad F, Amir O, Chioncel O, Leiro MC, Drozdz J, Erglis A, Fazlibegovic E, Fonseca C, Fruhwald F, Gatzov P, Goncalvesova E, Hassanein M, Hradec J, Kavoliuniene A, Lainscak M, Logeart D, Merkely B, Metra M, Persson H, Seferovic P, Temizhan A, Tousoulis D, Tavazzi L, Heart Failure Association of the ESC. Are hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2013;15:1173–84.
Iorio A, Senni M, Barbati G, Greene SJ, Poli S, Zambon E, Di Nora C, Cioffi G, Tarantini L, Gavazzi A, Sinagra G, Di Lenarda A. Prevalence and prognostic impact of non-cardiac co-morbidities in heart failure outpatients with preserved and reduced ejection fraction: a community-based study. Eur J Heart Fail. 2018;20(9):1257–66.
Iorio A, Rea F, Barbati G, Scagnetto A, Peruzzi E, Garavaglia A, Corrao G, Sinagra G, Di Lenarda A. HF progression among outpatients with HF in a community setting. Int J Cardiol. 2019;277:140–6.
Ouwerkerk W, Voors AA, Anker SD, Cleland JG, Dickstein K, Filippatos G, van der Harst P, Hillege HL, Lang CC, Ter Maaten JM, Ng LL, Ponikowski P, Samani NJ, van Veldhuisen DJ, Zannad F, Metra M, Zwinderman AH. Determinants and clinical outcome of uptitration of ACE-inhibitors and beta-blockers in patients with heart failure: a prospective European study. Eur Heart J. 2017;38:1883–90.
Martin BC, Wiley-Exley EK, Richards S, Domino ME, Carey TS, Sleath BL. Contrasting measures of adherence with simple drug use, medication switching, and therapeutic duplication. Ann Pharmacother. 2009;43:36–44.
World Health Organization, WHO International Working Group for Drug, Statistics Methodology, WHO Collaborating Centre for Drug Statistics Methodology, WHO Collaborating Centre for Drug Utilization Research and Clinical Pharmacological Service. Introduction to Drug Utilization Research. WHO Library Cataloguing-in-Publication Data; 2003. p. 9.
Grimmsmann T, Himmel W. Discrepancies between prescribed and defined daily doses: a matter of patients or drug classes? Eur J Clin Pharmacol. 2011;67:847–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Conflict of interest
Marta Spreafico, Francesca Gasperoni, Giulia Barbati, Francesca Ieva, Arjuna Scagnetto, Loris Zanier, Annamaria Iorio, Gianfranco Sinagra, and Andrea Di Lenarda have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Spreafico, M., Gasperoni, F., Barbati, G. et al. Adherence to Disease-Modifying Therapy in Patients Hospitalized for HF: Findings from a Community-Based Study. Am J Cardiovasc Drugs 20, 179–190 (2020). https://doi.org/10.1007/s40256-019-00367-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-019-00367-z