Abstract
Introduction
The aim of this study is to determine whether 99mTc-MAA SPECT/CT-based dosimetry could predict the actual absorbed dose in hepatocellular carcinoma (HCC) or liver metastases, treated by glass or resin microspheres.
Material and methods
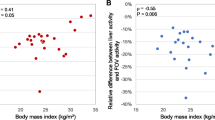
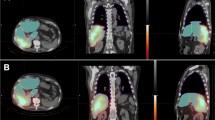
Fifty-seven patients who underwent selective internal radiation therapy (SIRT) were retrospectively included in the study, for a total of 59 treatments. Nineteen HCC were treated by resin microspheres (HCC-SIR), 20 HCC with glass microspheres (HCC-Thera), and 20 liver metastases with resin microspheres (Metastases-SIR). The mean absorbed doses in tumoral liver (Dm) and non-tumoral liver (DmNTL) were determined on the 99mTc-MAA SPECT/CT and the 90Y PET/CT, and compared with each other.
Results
DmNTL was < 50 Gy in the 3 groups, with a strong correlation in all population, albeit slightly lower in Metastases-SIR than HCC-SIR and HCC-Thera (CCC 0.8, 0.94 and 0.96, respectively). In tumoral liver, Dm was higher in HCC than metastases (159 ± 117 Gy versus 63 ± 31 Gy). 99mTc-MAA SPECT/CT proved to be a better indicator of Dm in HCC compared with metastases, with similar 99mTc-MAA-90Y concordance in resin and glass microspheres (CCC HCC-SIR 0.82, CCC HCC-Thera 0.82, and CCC Metastases-SIR 0.52).
Conclusion
99mTc-MAA SPECT/CT is a reasonably reliable tool for predicting the dose to the non-tumoral liver in both HCC and metastases, regardless of the type of microspheres. It is also fairly reliable for predicting the tumor dose in HCC, again regardless of the type of spheres, although individual variations are observed.








Similar content being viewed by others
References
Sangro B, Salem R, Kennedy A, et al. Radioembolization for hepatocellular carcinoma : a review of the evidence and treatment recommendations. Am J Clin Oncol. 2011;34:422–31.
Saxena A, Bester L, Shan L, et al. A systematic review on the safety and efficacy of yttrium-90 radioembolization for unresectable, chemorefractory colorectal cancer liver metastases. J Cancer Res Clin Oncol. 2014;140(4):537–47.
Fan KY, Wild AT, Halappa VG, et al. Neuroendocrine tumor liver metastases treated with yttrium-90 radioembolization. Contemp Clin Trials. 2016;50:143–9.
European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236.
Van Cutsem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27(8):1386–422.
Wasan HS, Gibbs P, Sharma NK, et al. First-line selective internal radiotherapy plus chemotherapy versus chemotherapy alone in patients with liver metastases from colorectal cancer (FOXFIRE, SIRFLOX, and FOXFIRE-Global): a combined analysis of three multicentre, randomised, phase 3 trials. Lancet Oncol. 2017;18(9):1159–71.
Vilgrain V, Pereira H, Assenat E, et al. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. Lancet Oncol. 2017;18:1624–36.
Chow PKH, Gandhi M, Tan S-B, et al. SIRveNIB: selective internal radiation therapy vs. sorafenib in Asia-Pacific patients with hepatocellular carcinoma. J Clin Oncol. 2018;36(19):1913–21.
Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2011;140:497–507.
Memon K, Kulik L, Lewandowski RJ, et al. Prospective evaluation of patients with early-/intermediate-stage hepatocellular carcinoma with disease progression following arterial locoregional therapy: candidacy for systemic treatment or clinical trials. J Vasc Interv Radiol. 2013;24(8):1189–97.
Salem R, Gilbertsen M, Butt Z, et al. Increased quality of life among hepatocellular carcinoma patients treated with radioembolization, compared with chemoembolization. Clin Gastroenterol Hepatol. 2013;11(10):1358–65.
Braat AJAT, Kappadath SC, Bruijnen RCG, et al. Adequate SIRT activity dose is as important as adequate chemotherapy dose. Lancet Oncol. 2017;18(11):e636.
Garin E, Rolland Y, Campillo-Gimenez B, et al. Negative phase 3 study of 90Y microspheres versus sorafenib in HCC. Lancet Oncol. 2018;19(2):e70.
Garin E, Lenoir L, Edeline J, et al. Boosted selective internal radiation therapy with 90Y-loaded glass microspheres (B-SIRT) for hepatocellular carcinoma patients: a new personalized promising concept. Eur J Nucl Med Mol Imaging. 2013;40(7):1057–68.
Garin E, Rolland Y, Pracht M, et al. High impact of macroaggregated albumin-based tumour dose on response and overall survival in hepatocellular carcinoma patients treated with 90 Y-loaded glass microsphere radioembolization. Liver Int. 2017;37(1):101–10.
Willowson KP, Hayes AR, Chan DLH, et al. Clinical and imaging-based prognostic factors in radioembolisation of liver metastases from colorectal cancer: a retrospective exploratory analysis. EJNMMI Res. 2017;7(1):46.
van den Hoven AF, Rosenbaum CENM, Elias SG, et al. Insights into the dose–response relationship of radioembolization with resin 90Y-microspheres: a prospective cohort study in patients with colorectal cancer liver metastases. J Nucl Med. 2016;57:1014–9.
Levillain H, Duran Derijckere I, Marin G, et al. 90Y-PET/CT-based dosimetry after selective internal radiation therapy predicts outcome in patients with liver metastases from colorectal cancer. EJNMMI Res. 2018;8(1):60.
Lam MG, Goris ML, Iagaru AH, et al. Prognostic utility of 90Y radioembolizationdosimetry based on fusion 99mTc-macroaggregated albumin-99mTc-sulfur colloid SPECT. J Nucl Med. 2013;54(12):2055–61.
Flamen P, Vanderlinden B, Delatte P, et al. Multimodality imaging can predict the metabolic response of unresectable colorectal liver metastases to radioembolization therapy with Yttrium-90 labeled resin microspheres. Phys Med Biol. 2008;53(22):6591–603 (Erratum in Phys Med Biol. 2014 May 21;59(10):2549–51).
Gnesin S, Canetti L, Adib S, et al. Partition model-based 99mTc-MAA SPECT/CT predictive dosimetry compared with 90Y TOF PET/CT posttreatment dosimetry in radioembolization of hepatocellular carcinoma: a quantitative agreement comparison. J Nucl Med. 2016;57(11):1672–8.
Haste P, Tann M, Persohn S, et al. Correlation of technetium-99m macroaggregated albumin and Yttrium-90 glass microsphere biodistribution in hepatocellular carcinoma: a retrospective review of pretreatment single photon emission CT and posttreatment positron emission tomography/CT. J Vasc Interv Radiol. 2017;28(5):722–30.
Kao YH, Steinberg JD, Tay YS, et al. Post-radioembolization yttrium-90 PET/CT - part 2: dose-response and tumor predictive dosimetry for resin microspheres. EJNMMI Res. 2013;3(1):57.
Dickinson NJ, Kalirai C, O'Connor RA, et al. Hepatic selective internal radiation therapy: how well does pretreatment 99mTc-macroaggregated albumin activity distribution and quantification agree with post-therapy bremsstrahlung imaging? Nucl Med Commun. 2018;39(9):809–17.
Pasciak A, Bourgeois A, Bradley Y. A comparison of techniques for 90Y PET/CT image-based dosimetry following radioembolization with resin microspheres. Front Oncol. 2014;4:121.
Allred JD, Niedbala J, Mikell JK, et al. The value of 99mTc-MAA SPECT/CT for lung shunt estimation in 90Y radioembolization: a phantom and patient study. EJNMMI Res. 2018;8(1):50.
Garin E, Rolland Y, Edeline J, et al. Personalized dosimetry with intensification using 90Y-loaded glass microsphere radioembolization induces prolonged overall survival in hepatocellular carcinoma patients with portal vein thrombosis. J Nucl Med. 2015;56(3):339–46.
Ho S, Lau WY, Leung TWT, et al. Clinical evaluation of the partition model for estimating radiation doses from yttrium-90 microspheres in the treatment of hepatic cancers. Eur J Nucl Med. 1997;24:293–8.
Chiesa C, Maccauro M, Romito R, et al. Need, feasibility and convenience of dosimetric treatment planning in liver selective internal radiation therapy with 90Y microspheres: the experience of the National Tumor Institute of Milan. Q J Nucl Med Mol Imaging. 2011;55(2):168–97.
Kao YH, Hock Tan AE, Burgmans MC, et al. Image-guided personalized predictive dosimetry by artery-specific SPECT/CT partition modeling for safe and effective 90Y radioembolization. J Nucl Med. 2012;53(4):559–66.
Wondergem M, Smits ML, Elschot M, et al. 99mTc-macroaggregated albumin poorly predicts the intrahepatic distribution of 90Y resin microspheres in hepatic radioembolization. J Nucl Med. 2013;54(8):1294–301.
Ulrich G, Dudeck O, Furth C, et al. Predictive value of intratumoral 99mTc-macroaggregated albumin uptake in patients with colorectal liver metastases scheduled for radioembolization with 90Y-microspheres. J Nucl Med. 2013;54(4):516–22.
Van de Wiele C, Maes A, Brugman E, et al. SIRT of liver metastases: physiological and pathophysiological considerations. Eur J Nucl Med Mol Imaging. 2012;39(10):1646–55.
Badiyan S, Bhooshan N, Chuong MD, et al. Correlation of radiation dose and activity with clinical outcomes in metastatic colorectal cancer after selective internal radiation therapy using yttrium-90 resin microspheres. Nucl Med Commun. 2018;39(10):915–20.
Spreafico C, Maccauro M, Mazzaferro V, et al. The dosimetric importance of the number of 90Y microspheres in liver transarterial radioembolization (TARE). Eur J Nucl Med Mol Imaging. 2014;41(4):634–8.
Chiesa C, Mira M, Maccauro M, et al. A dosimetric treatment planning strategy in radioembolization of hepatocarcinoma with 90Y glass microspheres. Q J Nucl Med Mol Imaging. 2012;56(6):503–8.
Garin E, Rolland Y, Laffont S, et al. Clinical impact of (99m)Tc-MAA SPECT/CT-based dosimetry in the radioembolization of liver malignancies with (90)Y-loaded microspheres. Eur J Nucl Med Mol Imaging. 2016;43(3):559–75.
Acknowledgments
We would like to express our gratitude toward the statistician (Laurence Seidel) and the referring physicians (Jean Delwaide, Anne Lamproye, Olivier Detry, Pierre Honoré, Marc Polus, Daniel Van Daele, Catherine Loly, Joelle Collignon, Elodie Gonne, Laurence Lousberg).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The CHU de Liège received speaker fees from Biocompatibles UK Ltd.
Ethical approval
All procedures were performed in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study design and exemption from informed consent were approved by the Institutional Review Board of Liege University Hospital.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology – Digestive tract
Electronic supplementary material
ESM 1
(PDF 431 kb)
Rights and permissions
About this article
Cite this article
Jadoul, A., Bernard, C., Lovinfosse, P. et al. Comparative dosimetry between 99mTc-MAA SPECT/CT and 90Y PET/CT in primary and metastatic liver tumors. Eur J Nucl Med Mol Imaging 47, 828–837 (2020). https://doi.org/10.1007/s00259-019-04465-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04465-7