Abstract
Purpose
The impact of supportive medications on patient-reported outcomes (PROs) has not been systematically evaluated. We describe the supportive medications used by treatment-naïve lung cancer patients and assess their association with PROs from MD Anderson Symptom Inventory (MDASI).
Methods
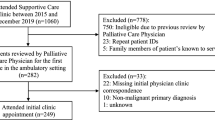
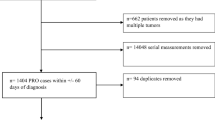
Treatment-naïve lung cancer patients who completed PROs from MDASI at the initial visit to MD Anderson Cancer Center were included. Medications from the initial visit were abstracted from the electronic medical records system and categorized into therapeutic classes based on U.S. Pharmacopeia v7.0. A chi-square or Mann-Whitney U test was conducted as appropriate.
Results
Among 459 patients, ~ 50% took any analgesics and 25% were on opioids. One-third of patients with moderate-severe pain were not on any analgesics. Patients taking opioids had significantly worse median pain scores (6 vs. 0) compared with those not taking any analgesics (p < 0.0001). Higher proportion of patients with moderate-severe pain took opioids compared with those with mild pain (52% vs. 16%, p < 0.0001). Patients on opioids also reported significantly worse scores for five other cancer-specific core symptoms and all six symptoms rating interference with daily life. Only 15% of patients with higher composite score for depression-related symptoms were on antidepressants. However, patients taking antidepressants did not significantly differ in any individual MDASI symptom scores compared with those not on antidepressants (p = 0.4858).
Conclusions
Our results suggest a need for better screening for pain and depression and optimization of pain management in treatment-naïve lung cancer patients since their poor functional status may result in suboptimal cancer therapy.
Similar content being viewed by others
References
Basch E (2016) Missing patients’ symptoms in cancer care delivery--the importance of patient-reported outcomes. JAMA Oncol 2:433–434
Kluetz PG, Slagle A, Papadopoulos EJ, Johnson LL, Donoghue M, Kwitkowski VE, Chen WH, Sridhara R, Farrell AT, Keegan P, Kim G, Pazdur R (2016) Focusing on core patient-reported outcomes in cancer clinical trials: symptomatic adverse events, physical function, and disease-related symptoms. Clin Cancer Res 22:1553–1558
Atkinson TM, Ryan SJ, Bennett AV, Stover AM, Saracino RM, Rogak LJ, Jewell ST, Matsoukas K, Li Y, Basch E (2016) The association between clinician-based common terminology criteria for adverse events (CTCAE) and patient-reported outcomes (PRO): a systematic review. Support Care Cancer 24:3669–3676
Basch E, Iasonos A, McDonough T, Barz A, Culkin A, Kris MG, Scher HI, Schrag D (2006) Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol 7:903–909
Basch E, Jia X, Heller G, Barz A, Sit L, Fruscione M, Appawu M, Iasonos A, Atkinson T, Goldfarb S, Culkin A, Kris MG, Schrag D (2009) Adverse symptom event reporting by patients vs clinicians: relationships with clinical outcomes. J Natl Cancer Inst 101:1624–1632
Basch E, Reeve BB, Mitchell SA, Clauser SB, Minasian LM, Dueck AC, Mendoza TR, Hay J, Atkinson TM, Abernethy AP, Bruner DW, Cleeland CS, Sloan JA, Chilukuri R, Baumgartner P, Denicoff A, St. Germain D, O'Mara AM, Chen A, Kelaghan J, Bennett AV, Sit L, Rogak L, Barz A, Paul DB, Schrag D (2014) Development of the National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). J Natl Cancer Inst 106:dju244
Fromme EK, Eilers KM, Mori M, Hsieh YC, Beer TM (2004) How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the quality-of-life questionnaire C30. J Clin Oncol 22:3485–3490
Iyer S, Roughley A, Rider A, Taylor-Stokes G (2014) The symptom burden of non-small cell lung cancer in the USA: a real-world cross-sectional study. Support Care Cancer 22:181–187
Lou VW, Chen EJ, Jian H et al (2017) Respiratory symptoms, sleep, and quality of life in patients with advanced lung cancer. J Pain Symptom Manag 53:250–256 e251
Lemonnier I, Baumann C, Jolly D, Arveux P, Woronoff-Lemsi MC, Velten M, Guillemin F (2011) Solitary pulmonary nodules: consequences for patient quality of life. Qual Life Res 20:101–109
Lheureux M, Raherison C, Vernejoux JM, Nguyen L, Nocent C, Tunon de Lara M, Taytard A (2004) Quality of life in lung cancer: does disclosure of the diagnosis have an impact? Lung Cancer 43:175–182
Montazeri A, Milroy R, Hole D, McEwen J, Gillis CR (2001) Quality of life in lung cancer patients: as an important prognostic factor. Lung Cancer 31:233–240
Blanco R, Maestu I, de la Torre MG, Cassinello A, Nuñez I (2015) A review of the management of elderly patients with non-small-cell lung cancer. Ann Oncol 26:451–463
Repetto L, Balducci L (2002) A case for geriatric oncology. Lancet Oncol 3:289–297
Cleeland CS, Allen JD, Roberts SA, Brell JM, Giralt SA, Khakoo AY, Kirch RA, Kwitkowski VE, Liao Z, Skillings J (2012) Reducing the toxicity of cancer therapy: recognizing needs, taking action. Nat Rev Clin Oncol 9:471–478
Yates JW (2001) Comorbidity considerations in geriatric oncology research. CA Cancer J Clin 51:329–336
Basch E (2013) Toward patient-centered drug development in oncology. N Engl J Med 369:397–400
Tirodkar MA, Acciavatti N, Roth LM, Stovall E, Nasso SF, Sprandio J, Tofani S, Lowry M, Friedberg MW, Smith-McLallen A, Chanin J, Scholle SH (2015) Lessons from early implementation of a patient-centered care model in oncology. J Oncol Pract 11:456–461
Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, Engstrom MC (2000) Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 89:1634–1646
Giuliani ME, Milne RA, Puts M et al (2016) The prevalence and nature of supportive care needs in lung cancer patients. Curr Oncol 23:258–265
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, Chirieac LR, Dacic S, Duhig E, Flieder DB, Geisinger K, Hirsch FR, Ishikawa Y, Kerr KM, Noguchi M, Pelosi G, Powell CA, Tsao MS, Wistuba I (2015) The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10:1243–1260
Cleeland CS, Zhao F, Chang VT, Sloan JA, O’Mara AM, Gilman PB, Weiss M, Mendoza TR, Lee JW, Fisch MJ (2013) The symptom burden of cancer: evidence for a core set of cancer-related and treatment-related symptoms from the eastern cooperative oncology group symptom outcomes and practice patterns study. Cancer 119:4333–4340
Mendoza TR, Wang XS, Lu C, Palos GR, Liao Z, Mobley GM, Kapoor S, Cleeland CS (2011) Measuring the symptom burden of lung cancer: the validity and utility of the lung cancer module of the M. D. Anderson Symptom Inventory. Oncologist 16:217–227
Jones D, Vichaya EG, Cleeland CS, Cohen L, Thekdi SM, Wang XS, Fisch MJ (2014) Screening for depressed mood in patients with cancer using the MD Anderson Symptom Inventory: investigation of a practical approach for the oncologist. J Oncol Pract 10:e95–e102
National Comprehensive Cancer Network. Adult cancer pain (version 1.2018). https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Accessed April 11
Cleeland CS, Nakamura Y, Mendoza TR, Edwards KR, Douglas J, Serlin RC (1996) Dimensions of the impact of cancer pain in a four country sample: new information from multidimensional scaling. Pain 67:267–273
Geisser ME, Cano A, Foran H (2006) Psychometric properties of the mood and anxiety symptom questionnaire in patients with chronic pain. Clin J Pain 22:1–9
Shacham S, Dar R, Cleeland CS (1984) The relationship of mood state to the severity of clinical pain. Pain 18:187–197
Collier R (2018) “Complainers, malingerers and drug-seekers” - the stigma of living with chronic pain. CMAJ 190:E204–E205
Jamison RN, Sheehan KA, Scanlan E et al (2014) Beliefs and attitudes about opioid prescribing and chronic pain management: survey of primary care providers. J Opioid Manag 10:375–382
Kanouse AB, Compton P (2015) The epidemic of prescription opioid abuse, the subsequent rising prevalence of heroin use, and the federal response. J Pain Palliat Care Pharmacother 29:102–114
Spitz A, Moore AA, Papaleontiou M, Granieri E, Turner BJ, Reid MC (2011) Primary care providers’ perspective on prescribing opioids to older adults with chronic non-cancer pain: a qualitative study. BMC Geriatr 11:35
Waugh OC, Byrne DG, Nicholas MK (2014) Internalized stigma in people living with chronic pain. J Pain 15:550 e551–550 e510
Centers for Disease C, Prevention (2011) Vital signs: overdoses of prescription opioid pain relievers---United States, 1999--2008. MMWR Morb Mortal Wkly Rep 60:1487–1492
Reuben DB, Alvanzo AA, Ashikaga T et al (2015) National Institutes of Health pathways to prevention workshop: the role of opioids in the treatment of chronic pain. Ann Intern Med 162:295–300
Paulozzi LJ, Mack KA, Hockenberry JM et al (2014) Vital signs: variation among states in prescribing of opioid pain relievers and benzodiazepines - United States. 2012 MMWR Morb Mortal Wkly Rep 63:563–568
Besson JM The complexity of physiopharmacologic aspects of pain(1997) La complexité des aspects physiopharmacologiques de la douleur. Drugs 53(Suppl 2):1–9
Peppin JF, Cheatle MD, Kirsh KL, McCarberg BH (2015) The complexity model: a novel approach to improve chronic pain care. Pain Med 16:653–666
Janberidze E, Hjermstad MJ, Brunelli C, Loge JH, Lie HC, Kaasa S, Knudsen AK, on behalf of EURO IMPACT (2014) The use of antidepressants in patients with advanced cancer--results from an international multicentre study. Psychooncology 23:1096–1102
Mitchell AJ, Yadegarfar M, Gill J, Stubbs B (2016) Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open 2:127–138
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 32 kb)
Rights and permissions
About this article
Cite this article
Hoang, J.M., Upadhyay, N., Dike, D.N. et al. Patient-reported outcomes in light of supportive medications in treatment-naïve lung cancer patients. Support Care Cancer 28, 1809–1816 (2020). https://doi.org/10.1007/s00520-019-05004-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05004-8