Abstract
Study design:
A review of the literature and three case reports.
Objectives:
Primary spinal melanoma (PSM) of extramedullary origin is a rare malignant condition with limited current literature in regards to its clinical course, magnetic resonance imaging (MRI) findings, treatment strategies and prognosis. We reported here three cases of PSM of extramedullary origin.
Setting:
China, Guangzhou.
Methods:
We report three cases of PSM of extramedullary origin. The clinical and radiological findings of these cases were retrospectively analyzed.
Results:
The three cases were all of males aged 39, 47 and 76 years, respectively. The duration of their symptoms was 3 weeks, 2 months and 11 months respectively. The extramedullary tumors were all well-defined solitary tumors and were located at C4-5, L2-3 and T9-10, respectively. In one case, involvement of the intervertebral foramen was found. Preoperative MRI showed hyperintense T1W signals and hypointense T2W signals in all three cases and all tumors were clinically misdiagnosed as schwannomas. The patients received total or subtotal resection surgery without radiotherapy or chemotherapy. Patients were alive at 18 months, 27 months and 36 months postoperative follow-up, respectively.
Conclusion:
PSM of extramedullary origin is a rare malignant tumor that shows characteristic findings on MRI. Surgical resection is the preferred treatment strategy.
Similar content being viewed by others
Introduction
Primary central nervous system (CNS) melanoma is a rare malignant condition, accounting for 1% of total CNS melanomas.1 Primary spinal melanoma (PSM) of extramedullary origin is an even rarer tumor; its diagnostic criteria are that there are no melanomas in locations other than the CNS (such as in the skin, mucosa or retina), and that melanoma is confirmed by histopathology.1 There are few published cases of PSM of extramedullary origin.
Case presentations
Case 1
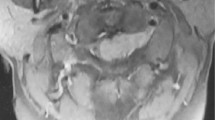
A 39-year-old male experienced 2 months of bilateral lower limb weakness from the hip with associated numbness and a 10-day history of ataxic gait. Neurological examination revealed high bilateral lower limb muscle tension with 4/5 power response in both legs and abnormal superficial sensation below T12. Magnetic resonance imaging (MRI) examination showed an extramedullary tumor at the T9-10 level, with measurements 1.9 cm×0.9 cm×1.2 cm. The well-defined mass was hyperintense on T1W images, hypointense on T2W images and homogeneously moderate enhancement after contrast administration (Figure 1). After exposing the dura, an oval-shaped black tumor was shown to be tightly adhered to the left T9 nerve root and spinal cord, and subsequently a subtotal resection of the tumor was performed. Diagnosis of melanoma was established histopathologically. No other melanoma foci were found after comprehensive postoperative examinations. The patient did not receive chemotherapy, radiotherapy or immunotherapy due to economic reasons. After 7 months of postoperative follow-up, the patient was still alive with improved neurological function.
Case 2
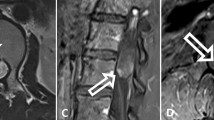
A 47-year-old male presented with an 11-month history of right finger numbness. Neurological examinations showed upper right limb hypoesthesia focusing on the dorsum of the right hand. Motor strength of the right upper limb was weakened (4/5 power response). Cervical MRI showed an extramedullary tumor at the C4-5 level, with measurements 1.3 cm×2.6 cm×1.5 cm. The tumor had spread to the right intervertebral foramen. It was hyperintense on T1W images, hypointense on T2W images and slightly enhanced after contrast administration. More hypointense patchy areas were found inside the tumor on T2W images (Figure 2). The patient underwent complete resection of the tumor with C5 nerve preservation. After the dura was opened, a solid black tumor growing along the right C5 nerve root was observed adherent to the spinal cord. Histopathology confirmed the tumor to be melanoma. No melanoma foci were discovered in any other parts of the body after comprehensive examination. The patient refused further postoperative radiotherapy, chemotherapy or immunotherapy, and was still alive with improved neurological function after 76 postoperative months.
A 47-year-old male with PSM of extramedullary origin at C4-5. MRI shows a hyperintense mass on sagittal T1W image (a), hypointense on sagittal T2W image at C4-5 (b) and homogeneously mild enhancement after contrast administration on axial image, which extends to the right intervertebral foramen (c).
Case 3
A 76-year-old male presented with a 3-week history of lower extremity weakness. Neurological examinations revealed 4/5 power response in the left lower extremity and 3/5 in the right lower extremity. Sensation was also reduced below the knee. Lumbar MRI revealed an extramedullary tumor located on the right anterior side of the spinal cord with a well-defined margin and measurements 1.3 cm×1.5 cm×5.0 cm. The tumor was slightly hyperintense on T1W images, primarily hypointense on T2W images and heterogeneous moderate enhancement after contrast administration (Figure 3). The patient underwent total resection of the tumor. After dural incision, a black-colored extramedullary tumor was observed with abundant blood supply. Histopathological examination revealed melanoma. No melanoma foci were observed in other parts of the body after comprehensive postoperative examinations. The patient refused further postoperative radiotherapy, chemotherapy or immunotherapy. The patient was alive with improved neurological function after 67 postoperative months.
A 76-year-old male with PSM of extramedullary origin at L2-3. MRI shows a slightly hyperintense mass on sagittal T1W image (a) and hypointense on sagittal T2W image (b). Hematoxylin and eosin staining shows a highly cellular malignant tumor with dense deposition of melanin granules (200×) (c) and immunohistochemical studies showed positivity for HMB-45 (200×) (d).
Discussion
The origin of PSM is still unclear; it may originate from melanoblasts accompanying the pia mater sheaths of vascular bundles or from neuroectodermal rest cells during embryogenesis.2,3
A systematic retrospective analysis of all the English literature on PSM of extramedullary origin published between 2000 and 2013 was performed. Papers were retrieved from PubMed using ‘primary melanoma’ and ‘spinal’ in ‘All fields’, ‘2000/01/01 to 2013/12/31’ in the ‘Date-Publication’ and ‘English’ in ‘Language’. A total of 24 patients with PSM of extramedullary origin have been summarized in a detailed table (Table 1).
This tumor can occur at any spinal segment; however, there were slightly more cases in the cervical segments (39.3%, 11/28). The patients were 16–82 years (mean: 47 years old) without gender preference. The majority of tumors were solitary and only one patient with multiple foci was reported.4 A few tumors originated from the nerve roots or had spinal nerve root involvement,5–9 which led to the enlargement of the intervertebral foramen, and even spread outside the intervertebral foramen2,10 or destruction of the vertebral pedicles.8,11
Signs and symptoms of this tumor were nonspecific and dependent on location.12 However, literature concerning the symptomatic bilateral papilledema induced by increased intracranial pressure 13 or the presence of subarachnoid hemorrhage-like symptoms have been reported, and thus clinicians should be aware of these rare presentations.14
PSM of extramedullary origin show typical changes on MRI. It presents with hyperintense T1W signals, hypointense T2W signals and varying enhancements. The characteristic MRI findings may be associated with melanin concentration and hemorrhages. The paramagnetic effect of stable, free radicals and blood products (methemoglobin) caused shortening of the T1 and T2 relaxation times in melanoma, consequently producing hyperintensity on T1W images and hypointensity on T2W images. Higher melanin concentration was associated with higher signal intensities on T1W images and lower signal intensities on T2W images.15 In CNS melanoma, this typical sign was observed in less than half of the patients;16 however, in our review of PSM of extramedullary origin, these typical changes were observed in 95% (20/21) of patients. Therefore, when an intraspinal extramedullary tumor shows hyperintense T1W and hypointense T2W signaling, melanoma should be suspected.2
Clinically, PSM of extramedullary origin may be misdiagnosed as a neurogenic tumor (schwannoma), ependymoma, metastatic tumor, hematoma or meningioma.3,5–7,9–11,17–19 Ninety percent of melanomas found in the CNS are metastatic tumors.8 A thorough physical examination is required to rule out melanoma in other organs outside of the spinal cord, before a diagnosis of PSM can be established. Spinal schwannoma or meningioma lacks the characteristic signals (hyperintensity on T1W and hypointensity on T2W) on MRI examination, even in pigmented schwannoma or meningioma.15 Spinal extramedullary hematoma usually presents with intense, ‘knife-like’ pain at the location of the hemorrhage (‘coup de poignard’) and subsequently progressive paralysis below the affected spinal level. These clinical features are different from those of primary melanoma.20
Although the treatment of PSM of extramedullary origin has not yet been standardized, most researchers recommend total surgical resection. Radiotherapy (from 30 to 60 Gy; median dose: 33.5 Gy) is effective for local control and is reserved for palliation of symptoms due to spinal cord compression or as an adjuvant to laminectomy.5,6,10,11,17,18,21 Melanoma is also refractory to most systemic chemotherapies. Currently, it has not been confirmed whether postoperative radiotherapy or chemotherapy (such as interferon, methotrexate and temozolomide) has a significant role in overall survival time.5,6,10,11,17,18,21 Although immunotherapy is the current paradigm shift in management of melanoma, the role of immunotherapy in these rare and particular cases have not yet been documented in the literature.
Metastasis was observed in the patients at diagnosis or after surgery and the locations included the brain, lung, bone, systemic metastasis or the intraspinal metastasis.3,8,17,21,22 Of the total 27 cases, only 2 cases had recurrence records.14,17 The survival time of PSM was between 2 weeks and 17 years (median time: 7 months). Six patients died during postoperative follow-up. Because of limited follow-up data, the exact survival rate is still unclear and a comparison of prognosis cannot be performed between patients with postoperative radiotherapy and those with postoperative chemotherapy.
Conclusion
In summary, PSM of extramedullary origin is very rare. The preoperative diagnosis is primarily based on typical MRI presentations. The primary treatment strategy for this tumor is surgery, and additional postoperative radiotherapy or chemotherapy may be implemented if necessary.
References
Jaiswal S, Vij M, Tungria A, Jaiswal AK, Srivastava AK, Behari S . Primary melanocytic tumors of the central nervous system: a neuroradiological and clinicopathological study of five cases and brief review of literature. Neurol India 2011; 59: 413–419.
Yan L, Chang Z, Liu Y, He BR, Hao DJ . Primary spinal melanoma: a case report and literature review. Chin Med J (Engl) 2012; 125: 4138–4141.
Yu J, Zhao DD, Chen S, Zhang JM, Xu J . Primary melanoma of the cervical spine with cerebral metastases: case report and review of the literature. J Int Med Res 2012; 40: 1207–1215.
Huang X, Pan X, Huang H, Zhan R . Multiple spinal cord melanoma: case report with emphasis on the difficult preoperative diagnosis. Turk Neurosurg 2013; 23: 534–538.
Naing A, Messina JL, Vrionis FR, Daud AI . Uncommon manifestations of common malignancies: case 3. Malignant melanoma arising from a spinal nerve root. J Clin Oncol 2004; 22: 3194–3195.
Kwon SC, Rhim SC, Lee DH, Roh SW, Kang SK . Primary malignant melanoma of the cervical spinal nerve root. Yonsei Med J 2004; 45: 345–348.
Lee NK, Lee BH, Hwang YJ, Sohn MJ, Chang S, Kim YH et al. Findings from CT, MRI, and PET/CT of a primary malignant melanoma arising in a spinal nerve root. Eur Spine J 2010; 19: S174–S178.
Ganiüsmen O, Özer FD, Mete M, Özdemir N, Bayol Ü . Slow progression and benign course of a primary malign melanoma of a lumbar nerve root. Clin Neurol Neurosurg 2012; 114: 166–168.
Sinha R, Rizvi TH, Chakraborti S, Ballal CK, Kumar A . Primary melanoma of the spinal cord: a case report. J Clin Diagn Res 2013; 7: 1148–1149.
Kanatas AN, Bullock MD, Pal D, Chakrabarty A, Chumas P . Intradural extramedullary primary malignant melanoma radiographically mimicking a neurofibroma. Br J Neurosurg 2007; 21: 39–40.
Jo KW, Kim SR, Kim SD, Park IS . Primary thoracic epidural melanoma: a case report. Asian Spine J 2010; 4: 48–51.
Kim MS, Yoon do H, Shin DA . Primary spinal cord melanoma. J Korean Neurosurg Soc 2010; 48: 157–161.
Kounin GK, Romansky KV, Traykov LD, Shotekov PM, Stoilova DZ . Primary spinal melanoma with bilateral papilledema. Clin Neurol Neurosurg 2005; 107: 525–527.
Montinaro A, Cantisani P, Punzi F, D'Agostino A . Cauda equina melanoma presenting with subarachnoid hemorrhage. A case report. J Neurosurg Sci 2004; 48: 139–141.
Smith AB, Rushing EJ, Smirniotopoulos JG . Pigmented lesions of the central nervous system: radiologic-pathologic correlation. Radiographics 2009; 29: 1503–1524.
Unal B, Castillo M . MRI features of a primary thoracic epidural melanoma: a case report. Clin Imaging 2007; 31: 273–275.
Freudenstein D, Wagner A, Bornemann A, Ernemann U, Bauer T, Duffner F . Primary melanocytic lesions of the CNS: report of five cases. Zentralbl Neurochi 2004; 65: 146–153.
Lee CH, Moon KY, Chung CK, Kim HJ, Chang KH, Park SH et al. Primary intradural extramedullary melanoma of the cervical spinal cord: case report. Spine (Phila Pa 1976) 2010; 35: E303–E307.
Cicuendez M, Paredes I, Munarriz PM, Hilario A, Cabello A, Lagares A . Primary melanoma of the cauda equina: Case report and review of the literature. Neurocirugia (Astur) 2012; 23: 112–115.
Kreppel D, Antoniadis G, Seeling W . Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev 2003; 26: 1–49.
Katalinic D, Anic B, Stern-Padovan R, Mayer M, Sentic M, Cikes N et al. Low back pain as the presenting sign in a patient with primary extradural melanoma of the thoracic spine—a metastatic disease 17 years after complete surgical resection. World J Surg Oncol 2011; 9: 150.
Schneider F, Putzier M . Primary leptomeningeal melanoma. Spine (Phila Pa 1976) 2002; 27: E545–E547.
Sanz-Trelles A, Arranz-Salas IM, Valenzuela-Serrano MI . Melanoma arising in and limited to a spinal nerve root of the cauda equina. Histopathology 2003; 43: 603–604.
Mekni A, Braham E, Nouira K, Ben Hammouda K, Bellil K, Haouet S et al. Primary central nervous system malignant melanoma: report of 5 cases. Pathologica 2007; 99: 71–75.
Vij M, Jaiswal S, Jaiswal AK, Behari S . Primary spinal melanoma of the cervical leptomeninges: report of a case with brief review of literature. Neurol India 2010; 58: 781–783.
Acknowledgements
We appreciate the help offered by Mr Charles Qian Wang (Prince of Wales Hospital, University of New South Wales, Sydney, Australia) for English editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, QY., Liu, AM., Li, HG. et al. Primary spinal melanoma of extramedullary origin: a report of three cases and systematic review of the literature. Spinal Cord Ser Cases 1, 15003 (2015). https://doi.org/10.1038/scsandc.2015.3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2015.3