Abstract
Purpose
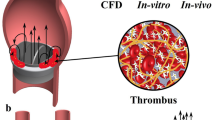
Thrombogenic complications are still a main issue in the general performance of cardiovascular implants, especially heart valves. To date, the thrombogenic potential of those prostheses is pre-clinically assessed in time consuming animal studies with questionable evidence.
Methods
In this study, we present a new in-vitro method to assess and compare deficiencies of heart valve substitutes concerning their thrombogenic performance and locate initial clot formation under physiological conditions using porcine blood. Therefore, an athrombogenic pulse duplicator (THIA3) was developed that simulates the anatomic and hemodynamic conditions in the vicinity of the aortic valve. Validation of this tester was carried out with regard to hemodynamics, reproducibility and using positive and negative control valves and by comparison of clot locations with literature data from chronic animal trials with sheep using a St. Jude bileaflet valve.
Results
Validation of the tester showed quasi-physiological hemodynamics and reproducible clot formation. Identical clot formations were found comparing findings in vitro with chronic animal trials.
Conclusion
The THIA 3 has proven its suitability for valid, reproducible evaluation of thrombogenic potential of heart valves in a short period of time.









Similar content being viewed by others
References
Arjunon, S., P. H. Ardana, N. Saikrishnan, S. Madhani, B. Foster, A. Glezer, and A. Yoganathan. Design of a pulsatile flow facility to evaluate thrombogenic potential of implantable cardic devices. JBME 137:045001, 2015.
Barstad, R. M., R. W. Stephens, M. J. Hamers, and K. S. Sakariassen. Protamine sulphate inhibits platelet membrane glycoprotein Ib-von willebrand factor activity. Thromb. Haemost. 83(2):334–337, 2000.
Baumgartner, H. R. The role of blood flow in platelet adhesion, fibrin deposition, and formation of mural thrombi. Microvasc. Res. 5(2):167–179, 1973.
Bellhouse, B. J., and F. H. Bellhouse. Mechanism of closure of the aortic valve. Nature 217(5123):86–87, 1968.
Bellhouse, B. J., and K. G. Reid. Fluid mechanics of the aortic valve. Br Heart J. 31(3):391, 1969.
Bluestein, D. Research approaches for studying flow-induced thromboembolic complications in blood recirculating devices. Expert Rev. Med. Devices. 1(1):65–80, 2004.
Bluestein, D., S. Einav, and M. J. Slepian. Device thrombogenicity emulation: a novel methodology for optimizing the thromboresistance of cardiovascular devices. J. Biomech. 46:338–344, 2013.
Bluestein, D., W. Yin, K. Affeld, and J. Jesty. Flow-induced platelet activation in mechanical heart valves. J. Heart Valve Dis. 13(3):501–508, 2004.
Bodnar, E. The medtronic parallel valve and the lessons learned. J. Heart Valve Dis. 5(6):572–573, 1996.
Cannegieter, S. C., F. R. Rosendaal, and E. Briët. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 89(2):635–641, 1994.
Chandran, K. B. Role of computational simulations in heart valve dynamics and design of valvular prostheses. Cardiovasc. Eng. Technol. 1(1):18–38, 2010.
Dodds, W. J. Joint report of the subcommittees on animal models of hemorrhagic and thrombotic diseases and on platelets. Thromb. Haemost. 48(1):106–107, 1982.
Ellis, J. T., B. R. Travis, and A. P. Yoganathan. An in vitro study of the hinge and near-field forward flow dynamics of the St. Jude Medical Regent bileaflet mechanical heart valve. Ann. Biomed. Eng. 28(5):524–532, 2000.
Grabowski, E. F., P. Didisheim, J. C. Lewis, J. T. Franta, and J. Q. Stropp. Platelet adhesion to foreign surfaces under controlled conditions of whole blood flow: human vs rabbit, dog, calf, sheep, pig, macaque, and baboon. Trans. Am. Soc. Artif. Intern. Organs. 23:141–151, 1977.
Hoehle P. Towards the transferability of endovascular animal trials: Differences in coagulation and fibrolysis of common animal models towards the human“. RWTH Aachen University, October 2000.
ISO 10993-4:2017. Biological evaluation of medical devices – Part 4: Selection of tests for interactions with blood.
ISO 5840-1:2015. Cardiovascular implants—Cardiac valve prostheses—Part 1: general requirements.
Kaeberich, A., I. Reindl, U. Raaz, L. Maegdefessel, A. Vogt, T. Linde, U. Steinseifer, E. Perzborn, B. Hauroeder, M. Buerke, K. Werdan, and A. Schlitt. Comparison of unfractionated heparin, low-molecular-weight heparin, low-dose and high-dose rivaroxaban in preventing thrombus formation on mechanical heart valves: results of an in vitro study. J. Thromb. Thrombolysis 32(4):417–425, 2011.
Kamat, S. G., A. D. Michelson, S. E. Benoit, J. L. Moake, D. Rajasekhar, J. D. Hellums, M. H. Kroll, and A. I. Schafer. Fibrinolysis inhibits shear stress-induced platelet aggregation. Circulation 92(6):1399–1407, 1995.
Keggen, L. A., M. M. Black, P. V. Lawford, D. R. Hose, and J. R. Strachan. The use of enzyme activated milk for in vitro simulation of prosthetic valve thrombosis. J. Heart Valve Dis. 5(1):74–83, 1996.
Kim, C. H., U. Steinseifer, and T. Schmitz-Rode. Thrombogenic evaluation of two mechanical heart valve prostheses using a new in-vitro test system. J. Heart Valve Dis. 18(2):207–213, 2009.
Kuetting, M., A. Sedaghat, M. Utzenrath, J. M. Sinning, C. Schmitz, J. Roggenkamp, N. Werner, T. Schmitz-Rode, and U. Steinseifer. In vitro assessment of the influence of aortic annulus ovality on the hydrodynamic performance of self-expanding transcatheter heart valve prostheses. J. Biomech. 47(5):957–965, 2014.
Lindblad, B., T. W. Wakefield, W. M. Whitehouse, and J. C. Stanley. The effect of protamine sulfate on platelet function. Scand. J. Thorac. Cardiovasc. Surg. 22(1):55–59, 1988.
Linde, T. Experimental and Numerical Evaluation of Thrombogenic Locations in Heart Valve Prostheses. Herzogenrath: Shaker, 2016.
Linde, T., K. F. Hamilton, C. Cuenca Navalon, T. Schmitz-Rode, and U. Steinseifer. Aortic root compliance influences hemolysis in mechanical heart valve prostheses: an in-vitro study. Int. J. Artif. Organs 35(7):495–502, 2012.
Maegdefessel, L., T. Linde, F. Krapiec, K. Hamilton, U. Steinseifer, J. van Ryn, U. Raaz, M. Buerke, K. Werdan, and A. Schlitt. In vitro comparison of dabigatran, unfractionated heparin, and low-molecular-weight heparin in preventing thrombus formation on mechanical heart valves. Thromb. Res. 126(3):e196–e200, 2010. https://doi.org/10.1016/j.thromres.2010.06.011.
Maegdefessel, L., T. Linde, T. Michel, K. F. Hamilton, U. Steinseifer, I. Friedrich, S. Schubert, B. Hauroeder, U. Raaz, M. Buerke, K. Werdan, and A. Schlitt. Argatroban and bivalirudin compared to unfractionated heparin in preventing thrombus formation on mechanical heart valves. Results of an in-vitro study. Thromb. Haemost. 101(6):1163–1169, 2009.
Martin, A. J., and J. R. Christy. An in-vitro technique for assessment of thrombogenicity in mechanical prosthetic cardiac valves: evaluation with a range of valve types. J. Heart Valve Dis. 13(3):509–520, 2004.
Martin, A. J., and J. R. Christy. Evaluation of an in-vitro thrombosis assessment procedure by application to the medtronic parallel and St. Jude medical valves. J. Heart Valve Dis. 13(4):667–675, 2004.
Meuris, B., E. Verbeken, and W. Flameng. Mechanical valve thrombosis in a chronic animal model: differences between monoleaflet and bileaflet valves. J. Heart Valve Dis. 14(1):96–104, 2005.
Nielsen, V. G. Protamine enhances fibrinolysis by decreasing clot strength: role of tissue factor-initiated thrombin generation. Ann. Thorac. Surg. 81(5):1720–1727, 2006.
Paul, R., O. Marseille, E. Hintze, L. Huber, H. Schima, H. Reul, and G. Rau. In vitro thrombogenicity testing of artificial organs. Int. J. Artif. Organs 21(9):548–552, 1998.
Reul, H., A. Vahlbruch, M. Giersiepen, T. Schmitz-Rode, V. Hirtz, and S. Effert. The geometry of the aortic root in health, at valve disease and after valve replacement. J. Biomech. 23(2):181–191, 1990.
Salzman, E. W., R. D. Rosenberg, M. H. Smith, J. N. Lindon, and L. Favreau. Effect of heparin and heparin fractions on platelet aggregation. J. Clin. Invest. 65(1):64–73, 1980.
Sonntag, S. J., T. A. S. Kaufmann, M. Büsen, M. Laumen, F. Graef, T. Linde, and U. Steinseifer. Numerical washout study of a pulsatile total artificial heart. Int. J. Artif. Organs. 37(3):241–252, 2014.
Turitto, V. T., and H. R. Baumgartner. Platelet interaction with subendothelium in flowing rabbit blood: effect of blood shear rate. Microvasc. Res. 17(1):38–54, 1979.
Weiss, H. J., H. R. Baumgartner, T. B. Tschopp, V. T. Turitto, and D. Cohen. Correction by factor viii of the impaired platelet adhesion to subendothelium in von willebrand disease. Blood 51(2):267–279, 1978.
Wieting D W, Dynamic Flow Characteristics of Heart Valves, PhD thesis, University of Texas Austin, 1969.
Acknowledgments
Parts of this research were funded by the German Research Foundation (DFG, SCHM1307/5-1). Both first authors contributed equally to this publication.
Funding
This study was funded by the German Research Foundation (DFG: Grant Number DFG, SCHM1307/5-1).
Conflict of interest
All authors declare that they have no conflict of interest. This article does not contain any studies with animals performed by any of the authors.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors. Presented animal data were taken from earlier studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Ajit P. Yoganathan oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Linde, T., Clauser, J., Meuris, B. et al. Assessing the Thrombogenic Potential of Heart Valve Prostheses: An Approach for a Standardized In-Vitro Method. Cardiovasc Eng Tech 10, 216–224 (2019). https://doi.org/10.1007/s13239-019-00408-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-019-00408-3