Abstract
Background
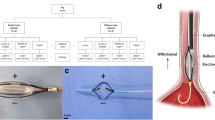
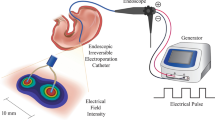
Irreversible electroporation (IRE) is an emerging tissue ablation technique, which is safe for sites where thermal-basis techniques are not suitable. The aim of this study is to evaluate the safety and efficacy of magnetic anchoring electrode (MAE)-assisted IRE for normal gastric tissue ablation in a rabbit model.
Methods
IRE (500 V, 100 μs, 99 pulses, 1 Hz) of the gastric wall was performed in 24 adult New Zealand rabbits with a novel catheter-mounted MAE with fluoroscopy and a surgical approach. Procedure time, procedure-related bleeding, perforation, and other complications were recorded. Animals were sacrificed at 30 min, 1 day, 3 days, 7 days, 14 days, and 28 days post-IRE. The stomach was removed en bloc, and the diameter of each lesion was measured. Histopathological analyses by Hematoxylin–Eosin (H&E), masson trichrome, alpha-smooth muscle action (α-SMA), and terminal-deoxynucleotidyl transferase mediated nick end labeling (TUNEL) were performed.
Results
Gastric tissue ablation with MAE-assisted IRE was successfully performed without any interruption. No perforation or bleeding was observed during IRE or throughout the follow-up period. A demarcated hemorrhage was found in the ablated area upon gross examination. H&E staining showed complete cell death with inflammatory infiltration, edema, and hemorrhaging. TUNEL presented diffuse positive cells in the ablated area. The tissue scaffold was well preserved without damage as indicated by Masson trichrome staining. Ulceration was observed starting from 3 days post-IRE. The mucosal layer was gradually recovered and regenerated within 14–28 days. No other complication was observed post-IRE.
Conclusions
MAE-assisted IRE is safe and effective for normal gastric tissue ablation and the gastric wall recovered in 14–28 days post-IRE.






Similar content being viewed by others
References
Charalampakis N, Economopoulou P, Kotsantis I, Tolia M, Schizas D, Liakakos T, Elimova E, Ajani JA, Psyrri A (2018) Medical management of gastric cancer: a 2017 update. Cancer Med 7:123–133. https://doi.org/10.1002/cam4.1274
Shen L, Shan YS, Hu HM, Price TJ, Sirohi B, Yeh KH, Yang YH, Sano T, Yang HK, Zhang X, Park SR, Fujii M, Kang YK, Chen LT (2013) Management of gastric cancer in Asia: resource-stratified guidelines. Lancet Oncol 14:e535–e547. https://doi.org/10.1016/S1470-2045(13)70436-4
Lim KT (2017) Surgical treatment of gastrointestinal stromal tumors of the stomach: current status and future perspective. Transl Gastroenterol Hepatol 2:104. https://doi.org/10.21037/tgh.2017.12.01
Virgilio E, Balducci G, Mercantini P, Giarnieri E, Giovagnoli MR, Montagnini M (2018) Laparoscopic intragastric surgery for treating early gastric cancer. Anticancer Res 38:1911–1916. https://doi.org/10.21873/anticanres.12428
Berlth F, Yang HK (2018) Minimal-invasive gastrectomy: what the west can learn from the east? Updates Surg 70:181–187. https://doi.org/10.1007/s13304-018-0547-z
Maple JT, Abu Dayyeh BK, Chauhan SS, Hwang JH, Komanduri S, Manfredi M, Konda V, Murad FM, Siddiqui UD, Banerjee S (2015) Endoscopic submucosal dissection. Gastrointest Endosc 81:1311–1325. https://doi.org/10.1016/j.gie.2014.12.010
Feng K, Yan J, Li X, Xia F, Ma K, Wang S, Bie P, Dong J (2012) A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 57:794–802. https://doi.org/10.1016/j.jhep.2012.05.007
Strauss AC, Agoston AT, Dulai PS, Srivastava A, Rothstein RI (2014) Radiofrequency ablation for Barrett’s-associated intramucosal carcinoma: a multi-center follow-up study. Surg Endosc 28:3366–3372. https://doi.org/10.1007/s00464-014-3629-0
Steel AW, Postgate AJ, Khorsandi S, Nicholls J, Jiao L, Vlavianos P, Habib N, Westaby D (2011) Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endosc 73:149–153. https://doi.org/10.1016/j.gie.2010.09.031
Srimathveeravalli G, Cornelis F, Wimmer T, Monette S, Kimm SY, Maybody M, Solomon SB, Coleman JA, Durack JC (2017) Normal porcine ureter retains lumen wall integrity but not patency following catheter-directed irreversible electroporation: imaging and histologic assessment over 28 days. J Vasc Interv Radiol 28:913–919.e1. https://doi.org/10.1016/j.jvir.2017.02.032
Davalos RV, Mir LM, Rubinsky B (2005) Tissue ablation with irreversible electroporation. Ann Biomed Eng 33:223–231. https://doi.org/10.1007/s10439-005-8981-8
Rubinsky B, Onik G, Mikus P (2007) Irreversible electroporation: a new ablation modality—clinical implications. Technol Cancer Res Treat 6:37–48. https://doi.org/10.1177/153303460700600106
Phillips M, Maor E, Rubinsky B (2011) Principles of tissue engineering with nonthermal irreversible electroporation. J Heat Transfer 133:011004. https://doi.org/10.1115/1.4002301
Faroja M, Ahmed M, Appelbaum L, Ben-David E, Moussa M, Sosna J, Nissenbaum I, Goldberg SN (2013) Irreversible electroporation ablation: is all the damage nonthermal? Radiology 266:462–470. https://doi.org/10.1148/radiol.12120609
Ueshima E, Schattner M, Mendelsohn R, Gerdes H, Monette S, Takaki H, Durack JC, Solomon SB, Srimathveeravalli G (2018) Transmural ablation of the normal porcine common bile duct with catheter-directed irreversible electroporation is feasible and does not affect duct patency. Gastrointest Endosc 87:300.e1–300.e6. https://doi.org/10.1016/j.gie.2017.05.004
Neven K, Van Es R, Van Driel V, Van Wessel H, Fidder H, Vink A, Doevendans P, Wittkampf F (2017) Acute and long-term effects of full-power electroporation ablation directly on the porcine esophagus. Circ Arrhythmia Electrophysiol 10:1–8. https://doi.org/10.1063/1.4985091
Maor E, Ivorra A, Mitchell JJ, Rubinsky B (2010) Vascular smooth muscle cells ablation with endovascular nonthermal irreversible electroporation. J Vasc Interv Radiol 21:1708–1715. https://doi.org/10.1016/j.jvir.2010.06.024
Phillips MA, Narayan R, Padath T, Rubinsky B (2012) Irreversible electroporation on the small intestine. Br J Cancer 106:490–495. https://doi.org/10.1038/bjc.2011.582
Srimathveeravalli G, Silk M, Wimmer T, Monette S, Kimm S, Maybody M, Solomon SB, Coleman J, Durack JC (2015) Feasibility of catheter-directed intraluminal irreversible electroporation of porcine ureter and acute outcomes in response to increasing energy delivery. J Vasc Interv Radiol 26:1059–1066. https://doi.org/10.1016/j.jvir.2015.01.020
Srimathveeravalli G, Wimmer T, Monette S, Gutta NB, Ezell PC, Maybody M, Weiser MR, Solomon SB (2013) Evaluation of an endorectal electrode for performing focused irreversible electroporation ablations in the swine rectum. J Vasc Interv Radiol 24:1249–1256. https://doi.org/10.1016/j.jvir.2013.04.025
Stillström D, Nilsson H, Jesse M, Peterhans M, Jonas E, Freedman J (2017) A new technique for minimally invasive irreversible electroporation of tumors in the head and body of the pancreas. Surg Endosc 31:1982–1985. https://doi.org/10.1007/s00464-016-5173-6
Wang HY, Bhunia AK, Lu C (2006) A microfluidic flow-through device for high throughput electrical lysis of bacterial cells based on continuous dc voltage. Biosens Bioelectron 22:582–588. https://doi.org/10.1016/j.bios.2006.01.032
Lee JM, Choi HS, Chun HJ, Kim ES, Keum B, Seo YS, Jeen YT, Lee HS, Um SH, Kim CD, Kim HB (2019) EUS-guided irreversible electroporation using endoscopic needle-electrode in porcine pancreas. Surg Endosc 33:658–662. https://doi.org/10.1007/s00464-018-6425-4
Sánchez-Velázquez P, Castellví Q, Villanueva A, Quesada R, Pañella C, Cáceres M, Dorcaratto D, Andaluz A, Moll X, Trujillo M, Burdió JM, Berjano E, Grande L, Ivorra A, Burdió F (2016) Irreversible electroporation of the liver: is there a safe limit to the ablation volume? Sci Rep 6:23781. https://doi.org/10.1038/srep23781
Martin RCG, Durham AN, Besselink MG, Iannitti D, Weiss MJ, Wolfgang CL, Huang KW (2016) Irreversible electroporation in locally advanced pancreatic cancer: a call for standardization of energy delivery. J Surg Oncol 114:865–871. https://doi.org/10.1002/jso.24404
Dobashi A, Storm AC, Wong Kee Song LM, Gostout CJ, Deters JL, Miller CA, Knipschield MA, Rajan E (2019) Efficacy and safety of an internal magnet traction device for endoscopic submucosal dissection: ex vivo study in a porcine model (with video). Surg Endosc 33:663–668. https://doi.org/10.1007/s00464-018-6486-4
Dobashi A, Wu SW, Deters JL, Miller CA, Knipschield MA, Cameron GP, Lu L, Rajan E, Gostout CJ (2019) Endoscopic magnet placement into subadventitial tunnels for augmenting the lower esophageal sphincter using submucosal endoscopy: ex vivo and in vivo study in a porcine model (with video). Gastrointest Endosc 89:422–428. https://doi.org/10.1016/j.gie.2018.09.015
Shang Y, Guo H, Zhang D, Xue F, Yan X, Shi A, Dong D, Wang S, Ma F, Wang H, Li J, Liu X, Luo R, Wu R, Lv Y (2017) An application research on a novel internal grasper platform and magnetic anchoring guide system (MAGS) in laparoscopic surgery. Surg Endosc 31:274–280. https://doi.org/10.1007/s00464-016-4968-9
Matsuzaki I, Hattori M, Hirose K, Esaki M, Yoshikawa M, Yokoi T, Kobayashi M, Miyahara R, Hirooka Y, Goto H (2018) Magnetic anchor–guided endoscopic submucosal dissection for gastric lesions (with video). Gastrointest Endosc 87:1576–1580. https://doi.org/10.1016/j.gie.2018.01.015
On R, Technology E (2013) Magnets in the GI tract. Gastrointest Endosc 78:561–567. https://doi.org/10.1016/j.gie.2013.07.020
Rivas H, Robles I, Riquelme F, Vivanco M, Jiménez J, Marinkovic B, Uribe M (2018) Magnetic surgery: results from first prospective clinical trial in 50 patients. Ann Surg 267:88–93. https://doi.org/10.1097/SLA.0000000000002045
Kumar N, Aihara H, Thompson C, Ryou M, Ryan M (2014) A novel magnetic countertraction device for endoscopic submucosal dissection significantly reduces procedure time and minimizes technical difficulty. Endoscopy 46:422–425. https://doi.org/10.1055/s-0034-1364940
Kodama H, Vroomen LG, Ueshima E, Reilly J, Brandt W, Paluch LR, Monette S, Jones D, Solomon SB, Srimathveeravalli G (2018) Catheter-based endobronchial electroporation is feasible for the focal treatment of peribronchial tumors. J Thorac Cardiovasc Surg 155:2150–2159.e3. https://doi.org/10.1016/j.jtcvs.2017.11.097
Li J, Zeng J, Chen J, Shi J, Luo X, Fang G, Chai W, Zhang W, Liu T, Niu L (2017) Evaluation of the safety of irreversible electroporation on the stomach wall using a pig model. Exp Ther Med 14:696–702. https://doi.org/10.3892/etm.2017.4559
Acknowledgements
This work was supported by a grant of National Key R&D Project of China (No. 2018YFC0115300), National Natural Science Foundation of China (No. 81727802), and the Fundamental Research Funds for the Central Universities (No. SXJH012019076). In addition, we would like to thank Dr. Aihua Shi from National Local Joint Engineering Research Center for Precision Surgery and Regenerative Medicine, First Affiliated Hospital of Xi’an Jiaotong University for the fabrication of magnetic anchoring electrode.
Author information
Authors and Affiliations
Contributions
FGR, LSH, XPY, DKC, RQW, and YL designed the study; FGR, QSL, ZYG, JZ, WMG, ZZ, and PKC performed the animal study; FGR, QSL, XC, and DKC performed the data analysis and interpretation; FGR, QSL, LSH, and XPY drafted the manuscript; RQW and YL revised the manuscript; all authors approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
Fenggang Ren, Qingshan Li, Liangshuo Hu, Xiaopeng Yan, Zhongyang Gao, Jing Zhang, Weiman Gao, Zhe Zhang, Pengkang Chang, Xue Chen, Dake Chu, Rongqian Wu, and Yi Lv have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ren, F., Li, Q., Hu, L. et al. Safety and efficacy of magnetic anchoring electrode-assisted irreversible electroporation for gastric tissue ablation. Surg Endosc 34, 580–589 (2020). https://doi.org/10.1007/s00464-019-06800-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06800-3