Abstract
Vascular tissue engineering of the middle layer of natural arteries requires contractile smooth muscle cells (SMC) which can be differentiated from adipose-derived mesenchymal stem cells (ASC) by treatment with transforming growth factor-β, sphingosylphosphorylcholine and bone morphogenetic protein-4 (TSB). Since mechanical stimulation may support or replace TSB-driven differentiation, we investigated its effect plus TSB-treatment on SMC orientation and contractile protein expression. Tubular fibrin scaffolds with incorporated ASC or pre-differentiated SMC were exposed to pulsatile perfusion for 10 days with or without TSB. Statically incubated scaffolds served as controls. Pulsatile incubation resulted in collagen-I expression and orientation of either cell type circumferentially around the lumen as shown by alpha smooth muscle actin (αSMA), calponin and smoothelin staining as early, intermediate and late marker proteins. Semi-quantitative Westernblot analyses revealed strongly increased αSMA and calponin expression by either pulsatile (12.48-fold; p < 0.01 and 38.15-fold; p = 0.07) or static incubation plus TSB pre-treatment (8.91-fold; p < 0.05 and 37.69-fold; p < 0.05). In contrast, contractility and smoothelin expression required both mechanical and TSB stimulation since it was 2.57-fold increased (p < 0.05) only by combining pulsatile perfusion and TSB. Moreover, pre-differentiation of ASC prior to pulsatile perfusion was not necessary since it could not further increase the expression level of any marker.







Similar content being viewed by others
References
Aper, T., M. Wilhelmi, C. Gebhardt, K. Hoeffler, N. Benecke, A. Hilfiker, and A. Haverich. Novel method for the generation of tissue-engineered vascular grafts based on a highly compacted fibrin matrix. Acta Biomater 29:21–32, 2016.
Birukov, K. G., N. Bardy, S. Lehoux, R. Merval, V. P. Shirinsky, and A. Tedgui. Intraluminal pressure is essential for the maintenance of smooth muscle caldesmon and filamin content in aortic organ culture. Arterioscler Thromb Vasc Biol 18:922–927, 1998.
Dan, P., E. Velot, V. Decot, and P. Menu. The role of mechanical stimuli in the vascular differentiation of mesenchymal stem cells. J Cell Sci 128:2415–2422, 2015.
Finney, A. C., K. Y. Stokes, C. B. Pattillo, and A. W. Orr. Integrin signaling in atherosclerosis. Cell Mol Life Sci 74:2263–2282, 2017.
Gui, L., M. J. Boyle, Y. M. Kamin, A. H. Huang, B. C. Starcher, C. A. Miller, M. J. Vishnevetsky, and L. E. Niklason. Construction of tissue-engineered small-diameter vascular grafts in fibrin scaffolds in 30 days. Tissue Eng Part A 20:1499–1507, 2014.
Haruguchi, H., and S. Teraoka. Intimal hyperplasia and hemodynamic factors in arterial bypass and arteriovenous grafts: a review. J Artif Organs 6:227–235, 2003.
Hruska, K. A., S. Mathew, and G. Saab. Bone morphogenetic proteins in vascular calcification. Circ Res 97:105–114, 2005.
Isenberg, B. C., C. Williams, and R. T. Tranquillo. Endothelialization and flow conditioning of fibrin-based media-equivalents. Ann Biomed Eng 34:971–985, 2006.
Jufri, N. F., A. Mohamedali, A. Avolio, and M. S. Baker. Mechanical stretch: physiological and pathological implications for human vascular endothelial cells. Vasc Cell 7:8, 2015.
Lau, S. Strategies for the generation of fully autologous tissue-engineered fibrin-based vascular grafts resembling three-layered natural arteries. In: Department of Cardiothoracic, Transplant and Vascular Surgery. Hannover: Hannover Medical School, 2017, p. 143.
Lau, S., D. Eicke, M. Carvalho Oliveira, B. Wiegmann, C. Schrimpf, A. Haverich, R. Blasczyk, M. Wilhelmi, C. Figueiredo, and U. Boer. Low immunogenic endothelial cells maintain morphological and functional properties required for vascular tissue engineering. Tissue Eng. A 24:432–447, 2018.
Lau, S., M. Klingenberg, A. Mrugalla, F. Helms, D. Sedding, A. Haverich, M. Wilhelmi, and U. Boer. Biochemical myogenic differentiation of ASC is donor-dependent and requires sound characterization. Tissue Eng. A 2019
Lau, S., C. Schrimpf, M. Klingenberg, F. Helfritz, T. Aper, A. Haverich, M. Wilhelmi, and U. Böer. Evaluation of autologous tissue sources for the isolation of endothelial cells and adipose tissue-derived mesenchymal stem cells to pre-vascularize tissue-engineered vascular grafts. BioNanoMaterials 16:309–321, 2015.
Lee, W. C., T. M. Maul, D. A. Vorp, J. P. Rubin, and K. G. Marra. Effects of uniaxial cyclic strain on adipose-derived stem cell morphology, proliferation, and differentiation. Biomech Model Mechanobiol 6:265–273, 2007.
Lin, S., and K. Mequanint. Bioreactor-induced mesenchymal progenitor cell differentiation and elastic fiber assembly in engineered vascular tissues. Acta Biomater 59:200–209, 2017.
Low, E. L., A. H. Baker, and A. C. Bradshaw. TGFbeta, smooth muscle cells and coronary artery disease: a review. Cell Signal 2018.
Mack, L., B. Brill, N. Delis, and B. Groner. Endotoxin depletion of recombinant protein preparations through their preferential binding to histidine tags. Anal Biochem 466:83–88, 2014.
Mosesson, M. W., K. R. Siebenlist, and D. A. Meh. The structure and biological features of fibrinogen and fibrin. Ann N Y Acad Sci 936:11–30, 2001.
Nieponice, A., T. M. Maul, J. M. Cumer, L. Soletti, and D. A. Vorp. Mechanical stimulation induces morphological and phenotypic changes in bone marrow-derived progenitor cells within a three-dimensional fibrin matrix. J Biomed Mater Res A 81:523–530, 2007.
O’Cearbhaill, E. D., M. Murphy, F. Barry, P. E. McHugh, and V. Barron. Behavior of human mesenchymal stem cells in fibrin-based vascular tissue engineering constructs. Ann Biomed Eng 38:649–657, 2010.
Park, J. S., J. S. Chu, C. Cheng, F. Chen, D. Chen, and S. Li. Differential effects of equiaxial and uniaxial strain on mesenchymal stem cells. Biotechnol Bioeng 88:359–368, 2004.
Park, J. S., J. S. Chu, A. D. Tsou, R. Diop, Z. Tang, A. Wang, and S. Li. The effect of matrix stiffness on the differentiation of mesenchymal stem cells in response to TGF-beta. Biomaterials 32:3921–3930, 2011.
Patel, S., Y. Shi, R. Niculescu, E. H. Chung, J. L. Martin, and A. Zalewski. Characteristics of coronary smooth muscle cells and adventitial fibroblasts. Circulation 101:524–532, 2000.
Rensen, S. S. M., P. Doevendans, and G. van Eys. Regulation and characteristics of vascular smooth muscle cell phenotypic diversity. Netherlands Heart Journal 15:100–108, 2007.
Rousou, J. A. Use of fibrin sealants in cardiovascular surgery: a systematic review. J Card Surg 28:238–247, 2013.
Schwarz, H., M. Schmittner, A. Duschl, and J. Horejs-Hoeck. Residual endotoxin contaminations in recombinant proteins are sufficient to activate human CD1c + dendritic cells. PloS ONE 9:e113840, 2014.
Syedain, Z. H., J. S. Weinberg, and R. T. Tranquillo. Cyclic distension of fibrin-based tissue constructs: evidence of adaptation during growth of engineered connective tissue. Proc Natl Acad Sci USA 105:6537–6542, 2008.
Tatterton, M., S. P. Wilshaw, E. Ingham, and S. Homer-Vanniasinkam. The use of antithrombotic therapies in reducing synthetic small-diameter vascular graft thrombosis. Vasc Endovasc Surg 46:212–222, 2012.
Toma, I., and T. A. McCaffrey. Transforming growth factor-beta and atherosclerosis: interwoven atherogenic and atheroprotective aspects. Cell Tissue Res 347:155–175, 2012.
Wang, C., L. Cen, S. Yin, Q. Liu, W. Liu, Y. Cao, and L. Cui. A small diameter elastic blood vessel wall prepared under pulsatile conditions from polyglycolic acid mesh and smooth muscle cells differentiated from adipose-derived stem cells. Biomaterials 31:621–630, 2010.
Wilson, W. R., T. C. Bower, M. A. Creager, S. Amin-Hanjani, P. T. O’Gara, P. B. Lockhart, R. O. Darouiche, B. Ramlawi, C. P. Derdeyn, A. F. Bolger, M. E. Levison, K. A. Taubert, R. S. Baltimore, and L. M. Baddour. Vascular graft infections, mycotic aneurysms, and endovascular infections: a scientific statement from the American Heart Association. Circulation 134:e412–e460, 2016.
Zhang, D., M. B. Sun, J. Lee, A. A. Abdeen, and K. A. Kilian. Cell shape and the presentation of adhesion ligands guide smooth muscle myogenesis. J Biomed Mater Res A 104:1212–1220, 2016.
Acknowledgments
We thank S. Zippusch for her help with the fibrinogen isolation.
Funding
This work has been carried out as an integral part of the BIOFABRICATION FOR NIFE (2012) Initiative, which is financially supported by the Lower Saxonian Ministry for Science and Culture and the VolkswagenStiftung. (NIFE is the Lower Saxonian Center for Biomedical Engineering, Implant Research and Development—a joint translational research center of the Hannover Medical School, the Leibniz University Hannover, the Foundation University of Veterinary Medicine Hannover and the Laser Center Hannover).
Author Contributions
There were no contributions that do not justify authorship.
Conflict of interest
No conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Joel Stitzel oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
10439_2019_2234_MOESM1_ESM.tif
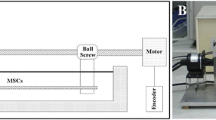
Supplemental Fig. S1: A: Composition of the vessel mold. The vessel mold consisted of two half-shells of polyether ether ketone (PEEK), two Teflon®-cuffs with drill holes for the application of the fibrinogen/thrombin-mixture and a tubular placeholder (I). The mold was fixed using a hose clamp and adhesion tape and brought into an upright position for initial static polymerization (II). The casted tubes were 10 cm in length with a luminal diameter of 4.75 mm and a wall thickness of 1.63 mm. B: Manufacturing setup of the rotation unit. The rotation unit consisted of a computer-controlled water-cooled electric motor and a rotation chamber (I) containing a rotating metal tube. After static polymerization, the vessel mold including the fibrin segment was placed in the metal tube, which contained drill holes to allow the outflow of excessive fluid during rotation and was closed with a sealing cap (II). Supplementary material 1 (TIFF 3961 kb)
10439_2019_2234_MOESM2_ESM.tif
Supplemental Fig. S2: Effect of fibrin compaction on biomechanical strength. Burst pressure or tensile strength was measured of uncompacted or compacted fibrin scaffolds. Shown are means ± SD of 6 scaffolds. **p < 0.01 and #p < 0.0001 by student’s T test. Supplementary material 2 (TIFF 103 kb)
10439_2019_2234_MOESM3_ESM.tif
Supplemental Fig. S3: Quantification of cyclic strain. Fibrin segments (n = 12, 3 runs) were exposed to pulsatile perfusion under video recordings. Images of segments under maximal (systolic) and minimal (diastolic) pressure were subsequently analyzed using the measurement-software “MB Ruler”©. Wall strain was calculated using the formula Strain (%) = (Diameter Systolic/Diameter Diastolic)*100–100. Supplementary material 3 (TIFF 7318 kb)
10439_2019_2234_MOESM4_ESM.tif
Supplemental Fig. S4: Live/dead staining for analyzing Zell viability after the compaction process and determine the optimal zell count per tube. Fibrin scaffolds where seeded with 0.5, 1 and 1.5 × 107 cells/tube and live/dead staining was performed on plane sections of 0.5 cm Rings on day 1, 5 and 8 after the compaction process. Living cells are stained green (Calcein) and dead cells are stained red (Ethidium-Homodimer). Scale bar = 100 µm. Supplementary material 4 (TIFF 4965 kb)
10439_2019_2234_MOESM5_ESM.tif
Supplemental Fig. S5: Impact of treatment with myogenic factors on scaffold calcification. Fibrin segments containing either adipose-derived mesenchymal stem cells (ASC) or pre-differentiated smooth muscle cells (SMC) were statically incubated or exposed to pulsatile perfusion for 10 days with or without the myogenic factors TGFβ1, SPC and BMP4 (TSB). Shown are cryo sections stained by Alizarin Red. No calcium deposits in either group (A-C) were observed as shown in the positive control (D; see purple arrows pointing to calcium crystals in calcified decellularized equine carotid artery as vascular graft in sheep as published in Böer et al., Int J Art Org, 2013, 36(3) 184). Scale bar: 100 µm. Supplementary material 5 (TIFF 26182 kb)
10439_2019_2234_MOESM6_ESM.tif
Supplemental Fig. S6: Expression of myogenic marker proteins in myogenic factor pre-differentiated ASC. Adipose-derived mesenchymal stem cells (ASC) cultured with 1 % FCS or differentiated towards the myogenic phenotype with TGFβ1, BMP4 and SPC for 8 days (n = 3 in both groups) were analyzed by Western blot analysis for the expression of α smooth muscle actin (αSMA), calponin and smoothelin prior to embedding into the fibrin graft. FCS = fetal calf serum, TGFβ1 = Transforming growth factor β1, BMP4 = Bone morphogenetic protein 4, SPC = Sphingosylphosphorylcholine. Supplementary material 6 (TIFF 5721 kb)
Rights and permissions
About this article
Cite this article
Helms, F., Lau, S., Klingenberg, M. et al. Complete Myogenic Differentiation of Adipogenic Stem Cells Requires Both Biochemical and Mechanical Stimulation. Ann Biomed Eng 48, 913–926 (2020). https://doi.org/10.1007/s10439-019-02234-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-019-02234-z