Evaluation of pulmonary artery pressure in patients with juvenile systemic lupus erythematosus (jSLE)
DOI:
https://doi.org/10.17305/bjbms.2017.2178Keywords:
Doppler echocardiography, juvenile systemic lupus erythematosus, pulmonary artery pressure, pulmonary artery hypertension, right ventricle, jSLE, PAH, PAP, PASP, mPAPAbstract
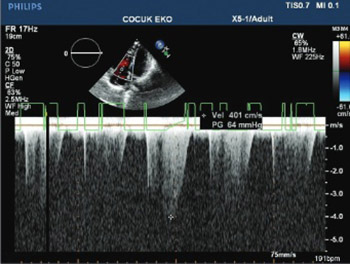
Juvenile systemic lupus erythematosus (jSLE) is a chronic multisystemic autoimmune disease. Previous studies among adults have shown impaired right ventricular (RV) function in patients with SLE. Also, these patients may develop pulmonary artery hypertension (PAH), which is one of the most threatening complications of SLE. Nevertheless, studies on PAH among jSLE patients are still rare. The aim of this study was to assess the RV function in jSLE patients by Doppler echocardiography (Echo Doppler). We also estimated pulmonary artery systolic pressure (PASP) and mean pulmonary artery pressure (mPAP) in these patients. A total of 38 jSLE patients and 40 sex- and age-matched controls were retrospectively analyzed. All patients underwent combined M-mode, cross-sectional echo, and Doppler Echo examination. The RV function was significantly impaired in jSLE patients compared to controls. PASP and mPAP were normal in 37 out of 38 patients (97.37%), however, the mean values of PASP and mPAP were significantly higher in jSLE patients compared to controls (26.90 mmHg versus 21.71 mmHg and 12.63 mmHg versus 9.89 mmHg, respectively) [p < 0.05]. Only one patient (2.6 %) had elevated mPAP (60 mmHg). The right cardiac catheterization confirmed PAH in this patient. Although PAH was detected only in one patient, there was a marked increase of PAP in our jSLE patients. Overall, PASP and mPAP were significantly higher in jSLE patients compared to healthy controls. Prospective studies with ethnically diverse cohorts could give more insight on the relevance of PAP and PHT in patients with jSLE.
Downloads
References
Borgia RE, Silverman ED. Childhood-onset systemic lupus erythematosus: An update. Curr Opin Rheumatol 2015;27(5):483-92. https://doi.org/10.1097/BOR.0000000000000208.
Kasparian A, Floros A, Gialafos E, Kanakis M, Tassiopoulos S, Kafasi N, et al. Raynaud's phenomenon is correlated with elevated systolic pulmonary arterial pressure in patients with systemic lupus erythematosus. Lupus 2007;16(7):505-8. https://doi.org/10.1177/0961203307080629.
Artim-Esen B, Sahin S, Çene E, Şahinkaya Y, Barut K, Adrovic A, et al. Comparison of disease characteristics, organ damage, and survival in patients with juvenile-onset and adult-onset systemic lupus erythematosus in a combined cohort from 2 tertiary centers in Turkey. J Rheumatol 2017;44(5):619-25. https://doi.org/10.3899/jrheum.160340.
Dedeoglu R, Sahin S, Koka A, Öztunç F, Adroviç A, Barut K, et al. Evaluation of cardiac functions in juvenile systemic lupus erythematosus with two-dimensional speckle tracking echocardiography. Clin Rheumatol 2016;35(8):1967-75. https://doi.org/10.1007/s10067-016-3289-7.
Huang C, Li M, Liu Y, Wang Q, Guo X, Zhao J, et al. Baseline characteristics and risk factors of pulmonary arterial hypertension in systemic lupus erythematosus patients. Medicine (Baltimore) 2016;95(10):e2761. https://doi.org/10.1097/MD.0000000000002761.
Qian J, Wang Y, Huang C, Yang X, Zhao J, Wang Q, et al. Survival and prognostic factors of systemic lupus erythematosus-associated pulmonary arterial hypertension: A PRISMA-compliant systematic review and meta-analysis. Autoimmun Rev 2016;15(3):250-7. https://doi.org/10.1016/j.autrev.2015.11.012.
Pérez-Peñate GM, Rúa-Figueroa I, Juliá-Serdá G, León-Marrero F, García-Quintana A, Ortega-Trujillo JR, et al. Pulmonary arterial hypertension in systemic lupus erythematosus: Prevalence and predictors. J Rheumatol 2016;43(2):323-9. https://doi.org/10.3899/jrheum.150451.
Thakkar V, Lau EM. Connective tissue disease-related pulmonary arterial hypertension. Best Pract Res Clin Rheumatol 2016;30(1):22-38. https://doi.org/10.1016/j.berh.2016.03.004.
Kamel SR, Omar GM, Darwish AF, Asklany HT, Ellabban AS. Asymptomatic pulmonary hypertension in systemic lupus erythematosus. Clin Med Insights Arthritis Musculoskelet Disord 2011;4:77-86. DOI: 10.4137/CMAMD.S7667.
Prabu A, Gordon C. Pulmonary arterial hypertension in SLE: What do we know? Lupus 2013;22(12):1274-85. https://doi.org/10.1177/0961203313505010.
Sahin S, Adrovic A, Barut K, Durmus S, Gelisgen R, Uzun H, et al. Pentraxin-3 levels are associated with vasculitis and disease activity in childhood-onset systemic lupus erythematosus. Lupus 2017;26(10):1089-94. https://doi.org/10.1177/0961203317699286.
Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997;40(9):1725. https://doi.org/10.1002/art.1780400928.
Jone PN, Ivy DD. Echocardiography in pediatric pulmonary hypertension. Front Pediatr 2014;2:124. https://doi.org/10.3389/fped.2014.00124.
Leal GN, Silva KF, França CM, Lianza AC, Andrade JL, Campos LM, et al. Subclinical right ventricle systolic dysfunction in childhood-onset systemic lupus erythematosus: Insights from two-dimensional speckle-tracking echocardiography. Lupus 2015;24(6):613-20. https://doi.org/10.1177/0961203314563135.
Min HK, Lee JH, Jung SM, Lee J, Kang KY, Kwok SK, et al. Pulmonary hypertension in systemic lupus erythematosus: An independent predictor of patient survival. Korean J Intern Med 2015;30(2):232-41. https://doi.org/10.3904/kjim.2015.30.2.232.