Abstract
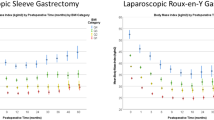
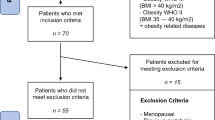
Over two-thirds of the United States is overweight or obese, and over 5% of the country is morbidly obese. Numerous public health preventative measures have been established to help battle this public health epidemic. Surgical obesity treatment, although now gaining popularity, has been an underutilized treatment option for obesity. Patients with a body mass index (BMI) of >40 or >35 kg m−2 with two or more comorbid conditions are eligible for bariatric surgery. Currently, the three most popular bariatric surgeries are Roux-en-y gastric bypass, sleeve gastrectomy and gastric banding procedures, all overwhelmingly performed laparoscopically. The purpose of this article is to discuss the heterogeneity of bariatric surgery. In our practice, among 834 patients operated over a 4-year period (2006–2010), patients were of an average age of 45 years (16–73 years), 80.4% were female patients, 82.5% had private insurance, 61% were White, 17% were Hispanic and 9% were Black. Patients had an average BMI of 46.2 kg m−2 (30.1–75.3 kg m−2), waist circumference of 133.6 cm (68.6–207.8 cm) and four preoperative comorbidities (0–11 comorbidities). Variation exists in surgeon practice patterns for preoperative weight-loss recommendations and complication rates based on surgery case volume. Despite variation in patient, surgeon and hospital characteristics, bariatric surgery outcomes are generally highly safe and effective.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
NIH, NHLBI Obesity Education Initiative. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Available online: http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf.
US Department of Health and Human Services. Overweight and obesity: a major public health issue. Prevent Rep 2001; 16.
Flegal KM, Graubard BI, Williamson DF, Gail MH . Cause-specific excess deaths associated with underweight, overweight, and obesity. J Am Med Assoc 2007; 298: 2028–2037.
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel HL et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007; 357: 741–752.
Weigle DS . Pharmacological therapy of obesity: past, present, and future. J Clin Endocrinol Metab 2003; 88: 2462–2469.
Farmer PE, Kim JY . Surgery and global health: a view from beyond the OR. World J Surg 2008; 32: 533–536.
Gastrointestinal surgery for severe obesity: Proceedings of a National Institutes of Health Consensus Development Conference. Am J Clin Nutr 1992; 55 (2 suppl): 487S–619S.
Santry HP, Gillen DL, Lauderdale DS . Trends in bariatric surgical procedures. JAMA 2005; 294: 1909–1917.
Livingston EH . Procedure incidence and in-hospital complication rates of bariatric surgery in the United States. Am J Surg 2004; 188: 105–110.
Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, Purnell JQ . Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 2002; 346: 1623–1630.
Leonetti F, Silecchia G, Iacobellis G, Ribaudo MC, Zappaterreno A, Tiberti C et al. Different plasma ghrelin levels after laparoscopic gastric bypass and adjustable gastric banding in morbid obese subjects. J Clin Endocrinol Metab 2003; 88: 4227–4231.
Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK . Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg 2008; 247: 401–407.
Langer FB, Reza Hoda MA, Bohdjalian A, Felberbauer FX, Zacherl J, Wenzl E et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg 2005; 15: 1024–1029.
Stoeckli R, Chanda R, Langer I, Keller U . Changes of body weight and plasma ghrelin levels after gastric banding and gastric bypass. Obes Res 2004; 12: 346–350.
Chopra A, Chao E, Etkin Y, Merklinger L, Lieb J, Delany H . Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg Endosc 2011; 26: 831–837.
Birkmeyer NJ, Dimick JB, Share D, Hawasli A, English WJ, Genaw J et al. Hospital complication rates with bariatric surgery in Michigan. JAMA 2010; 304: 435–442.
Flum DR, Salem L, Elrod JA, Dellinger EP, Cheadle A, Chan L . Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA 2005; 294: 1903–1908.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Farhbach K et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004; 292: 1724–1737.
Alami RS, Morton JM, Schuster R, Lie J, Sanchez BR, Peters A et al. Is there a benefit to preoperative weight loss in gastric bypass patients? A prospective randomized trial. Surg Obes Relat Dis 2007; 3: 141–145; discussion 145–146.
Van Nieuwenhove Y, Dambrauskas Z, Campillo-Soto A, van Dielen F, Wiezer R, Janssen I et al. Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: a randomized multicenter study. Arch Surg 2011; 146: 1300–1305.
Still CD, Benotti P, Wood GC, Gerhard GS, Petrick A, Reed M et al. Outcomes of preoperative weight loss in high-risk patients undergoing gastric bypass surgery. Arch Surg 2007; 142: 994–998; discussion 999.
Alvarado R, Alami RS, Hsu G, Safadi BY, Sanchez BR, Morton JM et al. The impact of preoperative weight loss in patients undergoing laparoscopic Roux-en-Y gastric bypass. Obes Surg 2005; 15: 1282–1286.
Cassie S, Menezes C, Birch DW, Shi X, Karmali S . Effect of preoperative weight loss in bariatric surgical patients: a systematic review. Surg Obes Relat Dis 2011; 7: 760–767; discussion 767.
Woodard GA, Peraza J, Bravo S, Toplosky L, Hernandez-Boussard T, Morton JM . One year improvements in cardiovascular risk factors: a comparative trial of laparoscopic Roux-en-Y gastric bypass vs adjustable gastric banding. Obes Surg 2010; 20: 578–582.
Benaiges D, Goday A, Ramon JM, Hernandez E, Pera M, Cano JF . Laparoscopic sleeve gastrectomy and laparoscopic gastric bypass are equally effective for reduction of cardiovascular risk in severely obese patients at one year of follow-up. Surg Obes Relat Dis 2011; 7: 575–580.
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012; 307: 56–65.
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD et al. Long-term mortality after gastric bypass surgery. N Engl J Med 2007; 357: 753–761.
Woodard GA, Downey J, Hernandez-Boussard T, Morton JM . Impaired alcohol metabolism after gastric bypass surgery: a case-crossover trial. J Am Coll Surg 2011; 212: 209–214.
Acknowledgements
Publication of this supplement was partially supported by Nutrilite Health Institute with an unrestricted educational contribution to Stanford Prevention Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lodhia, N., Morton, J. Weighing in on bariatric surgery: who and when?. Int J Obes Supp 2 (Suppl 1), S47–S50 (2012). https://doi.org/10.1038/ijosup.2012.12
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijosup.2012.12