Abstract
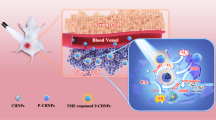
In this paper, a simple strategy is proposed to prepare a core-shell nanohybrid (PB@PCN) by the controllable coating of zirconium-porphyrin (PCN) shells on Prussian blue (PB) nanoparticles. By adjusting the thickness of the PCN shell, the PB@PCN nanohybrid with the best comprehensive performance was obtained for tumor treatment and imaging. The integrated nanosystem as a tandem catalyst is able to convert H2O2 to O2 through the PB core, and then the O2 is directly injected into the PCN framework, leading to a high quantum yield of singlet oxygen to kill tumor cells and attack heat shock proteins (HSPs). The nanohybrid was further camouflaged by a tumor cell membrane (PB@PCN@MEM) with good immune evasion and active targeting ability. Upon accumulation at the tumor site, PN@PCN@MEM showed an enhanced photodynamic therapeutic effect against hypoxic tumor cells. Furthermore, coupled with the photothermal therapy of PB, photothermal/photodynamic synergistic therapy of tumors can be realized. In addition, due to its excellent imaging performance, this core-shell nanohybrid can be employed for the multimodal image-guided therapy of tumors.
Similar content being viewed by others
Introduction
Tumors, as one of the deadliest diseases worldwide, seriously threaten the health of human beings. Engineering nanoparticles (NPs) that can selectively detect and efficiently destroy tumor cells in the body has been gaining momentum in the area of tumor therapy1,2,3. Driven by this, an increasing number of researchers have devoted themselves to developing multifunctional nanomaterials for tumor diagnosis and treatment4,5,6. Among them, core–shell nanohybrids have received tremendous attention due to the integration of multiple functionalities into the nanohybrid that go beyond the intrinsic limitations of individual components in the imaging and treatment of tumors7,8,9,10. Considering that the shell thickness will greatly affect the performance of the core–shell nanohybrid, it is of critical importance to control the shell structure while integrating functionality into nanohybrids11,12,13,14,15.
Light-driven therapeutics have attracted increasing attention due to their obvious advantages for tumor treatment, including negligible invasiveness, precise spatial-temporal selectivity, and a reduced number of side effects16,17,18,19,20. Photodynamic therapy (PDT) and photothermal therapy (PTT), as the most representative methods of phototherapy, have become powerful tools for tumor treatment, and growing efforts have been devoted to combining PTT and PDT to yield effective therapeutic synergism21. With the rapid development of nanotechnology, there is great interest in developing multifunctional core–shell nanohybrids with both photothermal and photodynamic properties22,23,24. However, in addition to the complex synthesis process, there are still several inherent limitations that need to be overcome. First, the hypoxic nature of the tumor microenvironment (TME) that is caused by the rapid proliferation of tumor cells and distorted tumor vessels, is highly detrimental to oxygen (O2)-dependent PDT25,26,27,28,29. Second, heat shock proteins (HSPs), which are upregulated after PTT, can enable tumor cells to resist heat-induced apoptosis, leading to actual performance compromise30,31,32. Therefore, how to effectively integrate multiple components on the nanometer scale to obtain core–shell nanohybrids with the capability of overcoming these impediments is of great significance in combined PDT/PTT tumor therapy.
To overcome the multiple limitations of combined PTT/PDT therapy and maximize the synergy between the core and the shell of the nanohybrid, a strategy for the controllable coating of a zirconium-porphyrin (PCN) shell on Prussian blue (PB) NPs has been proposed. Through a straightforward strategy, a series of PB@PCN nanohybrids with different shell thicknesses were prepared. The PB@PCN nanohybrid with the optimal shell thickness was further camouflaged by mouse colon cancer cell (CT26) membranes (PB@PCN@MEM) to endow the nanohybrid with good immune evasion and an active targeting ability33,34,35. As illustrated in Scheme 1, the PCN shell, with the advantages of facile diffusion of singlet oxygen (1O2), avoidable self-quenching and high photosensitizer (PS) loading, could efficiently convert O2 into highly toxic 1O2 to kill tumor cells by PDT and attack HSPs to promote the PTT effect36. In addition, the PB core could not only be used for PTT in tumors under near-infrared (NIR) irradiation but also convert the endogenous hydrogen peroxide (H2O2), which is overproduced in tumor cells, into O237. The generated O2 effectively relieves tumor hypoxia to enhance the therapeutic efficiency of PDT. In addition, PB@PCN@MEM could be used with multiple imaging techniques, including magnetic resonance imaging (MRI), fluorescence imaging (FL), photoacoustic imaging (PAI), and infrared imaging (IR), providing detailed information about the tumor and leading to improved PTT/PDT therapy.
Materials and methods
Materials and instrumentations
Dimethyl formamide (DMF), dimethyl sulfoxide (DMSO), K3[Fe(CN)6], hydrogen peroxide (H2O2), hydrochloric acid, and benzoic acid were purchased from Shanghai Reagent Chemical Co. (China). 4,4,4,4-(Porphine-5,10,15,20-tetrayl)tetrakis (H2TCPP) was obtained from Innochem (China). ZrOCl2·8H2O was purchased from Sigma-Aldrich (China), and polyvinylpyrrolidone (PVP) was purchased from Aladdin-Reagent Co. Ltd. (China). Ru(dpp)3Cl2 was obtained from Meryer Chemical Technology Co., Ltd. (Shanghai, China). Singlet oxygen sensor green (SOSG) was purchased from Invitrogen (USA). The membrane protein extraction kit, 2′,7′-dichlorofluorescin diacetate (DCFH-DA), Hoechst 33342, 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium-bromide (MTT) and propidium iodide (PI) were provided by the Beyotime Institute of Biotechnology (China). The calcein AM and annexin V-FITC/PI apoptosis and necrosis detection kit were obtained from Yeasen (Shanghai, China). The ROS-ID hypoxia/oxidative stress detection kit was purchased from Enzo Life Sciences (Switzerland). Antibodies were purchased from Abcam (China). Dulbecco’s modified Eagle’s medium (DMEM), Roswell Park Memorial Institute (RPMI) 1640 medium, penicillin-streptomycin, trypsin and fetal bovine serum (FBS) were purchased Gibco Invitrogen Corp (USA). All other solvents were of analytical grade and used as received. Polycarbonate porous membrane (400 nm) and Avanti mini extruder were purchased from Avanti Polar Lipids (USA). The syringe pump (Lead Fluid, TYD02-02, China) was used to deliver stock solutions. The morphology of NPs was detected by a transmission electron microscopy (TEM) (JEM-2100 microscope) and a field emission scanning electron microscope (SEM) (Zeiss SIGMA). The UV–vis absorbance was measured by a UV-vis spectrophotometer (Lambda Bio40, Perkin-Elmer) and fluorescence was detected by an LS55 luminescence spectrometer (Perkin-Elmer). Hydrodynamic size and zeta potential were measured by a Malvern Zetasizer Nano-ZS ZEM3600 (UK). All confocal laser microscopy images were collected by a confocal laser scanning microscopy (CLSM) (Nikon C1-Si TE2000, Japan). Fluorescence change was analyzed at cellular level by a flow cytometry (BD FACSAria™ III, USA). FL in vivo was performed on a small animal imaging system (PerkinElmer). The 660 nm and 808 nm NIR lasers (STONE Laser, China) were used for the PDT and PTT study, respectively. MTT assay was conducted on a microplate reader (BIO-RAD, Model 550, USA). MRI was conducted on a Bruker BioSpec 7 T/20 cm system (Bruker, Germany). The PAI system was built by Huazhong University of Science and Technology.
Preparation of PB NPs
In all, 1.1 g of K3[Fe(CN)6] and 24 g of PVP were dissolved in 300 mL of ultrapure water under sonication. Then, 270 μL of hydrochloric acid was added and the mixture was stirred at room temperature for 30 min. Next, the reaction was allowed to proceed at 80 °C for 20 h, and then the dark blue particles were collected by centrifugation (11,000 rpm, 15 min), followed by washing with ultrapure water once and DMF three times.
Controlled synthesis of core–shell PB@PCN NPs
A syringe pump was used to separately deliver metal (ZrOCl2∙8H2O) and ligand (TCPP) stock solutions at a controlled feed rate into the PB solution with stirring. In detail, controllable coating of the PCN shell on the PB core was carried out at 90 °C under atmospheric pressure in a DMF solvent system. First, 6 mg of PB and 222 mg of benzoic acid were dissolved in 40 mL of DMF in a three-neck bottle. Then, the ZrOCl2∙8H2O stock solution (in DMF, ZrOCl2 9.1 mM and benzoic acid 91 mM) and the TCPP stock solution (in DMF, 1.3 mM) were separately delivered into the three-neck bottle. In this process, PCN grew with PB as the core. The whole reaction process was carried out with stirring, and the feed rate was 0.5 mL h−1. By controlling the total feed (0.2 mL, 0.5 mL, 1 mL, 1.5 mL, 2 mL, 3 mL, 4 mL, or 6 mL), a series of PB@PCN NPs with different PCN shell thicknesses were obtained. Finally, the particles were collected by centrifugation and washed with DMF and ultrapure water.
Preparation of CT26 tumor cell membrane fragments
A membrane protein extraction kit was employed to extract the CT26 cell membrane. Briefly, the collected CT26 cells were dispersed in membrane protein extraction buffer solution and cooled at 4 °C for 15 min. Next, the cell suspension underwent three repeated freeze-thaw cycles. Then, the broken cell suspension was centrifuged (700 g, 10 min, 4 °C) to remove the precipitate, and the supernatant was further centrifuged (14,000 × g, 30 min) to obtain the precipitate.
Preparation of PB@PCN@MEM
The cell membrane coating process was conducted using an Avanti mini extruder. First, the prepared tumor cell membrane fragments and PB@PCN NPs (w/w = 1:1) were dispersed in ultrapure water, and the mixture was extruded through a polycarbonate porous membrane (400 nm) using an Avanti mini extruder. Then, PB@PCN@MEM was collected by centrifugation (8000 rpm, 15 min).
Photothermal effects of PB@PCN
To assess the photothermal performance, a series of concentrations (5, 10, 20, 50, and 100 mg L−1 in terms of PB) of PB@PCN was exposed to an 808 nm laser (1.0 W cm−2) for 600 s, with real-time monitoring of the temperature and recording of the image data. Moreover, PBS, PB (20 mg L−1) and PCN (10 mg L−1) were used as the control groups for PB@PCN (20 mg L−1 in terms of PB). To investigate the photostability of PB@PCN, the PB@PCN dispersion (20 mg L−1 in terms of PB) underwent four on/off cycles of 808 nm laser irradiation.
Detection of O2 generation in solution
[(Ru(dpp)3)]Cl2 was used as the O2 sensing probe, the fluorescence of which was reduced by molecular oxygen. To assess the influence of the PCN shell on the PB core catalytic efficiency, PB@PCN with three different PCN shell thicknesses (20 mg L−1 in terms of PB) were added to a 24-well plate with 3.0 wt% H2O2 and [(Ru(dpp)3)]Cl2 (10 mg L−1, 10 μL) and then incubated at 37 °C for 15 min. In addition, PBS, PB (20 mg L−1) and PB@PCN 3 mL + 808 nm irradiation were used as the control groups. After treatment, the fluorescence of [(Ru(dpp)3)]Cl2 was recorded by a small animal fluorescence imaging system (IVIS, λex = 488 nm, λem = 620 nm). Furthermore, the real-time production of O2 was measured via a DOG-3082 dissolved oxygen meter.
Detection of 1O2 generation in solution
The generation of 1O2 was monitored using a singlet oxygen sensor (SOSG) as a probe. First, the 1O2 generation in different solutions under 660 nm laser irradiation were compared to verify the enhanced 1O2 generation of PB@PCN. In simple terms, 10 μL of SOSG (500 μM in DMSO) was added to 990 μL of different solutions (PBS, H2O2, PB, PCN, PCN + H2O2, PB@PCN 3 mL, and PB@PCN 3 mL + H2O2 10 mg L−1 in terms of PCN and 0.3% H2O2). After irradiation (660 nm, 0.03 W cm−2) at different times, the fluorescence of the solutions at 530 nm was measured. The 1O2 generation ability was defined as (I–I0), where I0 is the initial fluorescence intensity.
Evaluation of intracellular O2 generation
CT26 cells were seeded and cultured for 24 h in a 24-well plate at 37 °C. Then, 10 μL of [(Ru(dpp)3)]Cl2 (10 mg L−1) was added into each well. Twelve hours later, the cells were washed with PBS, and 200 μL of 1640 medium was added. Then, PBS, PB or PB@PCN (final concentration: 20 mg L−1 in terms of PB) were added to the wells and further incubated for 24 h. After washing with PBS, the fluorescence of [(Ru(dpp)3)]Cl2 was recorded with a small animal fluorescence imaging system (λex = 488 nm, λem = 620 nm).
Detection of intracellular ROS
Intracellular ROS were measured by using DCFH-DA as the indicator. To detect intracellular ROS under normoxic conditions, CT26 cells were seeded and cultured for 24 h in a 6-well plate at 37 °C in 21% O2. Following treating CT26 cells with PBS, PB, PCN, or PB@PCN (PB 30 mg L−1, PCN 15 mg L−1) for 6 h, the medium was changed to the well-prepared DCFH-DA staining solution (1 × 10−6 M) and further incubated for 30 min. Next, the cells were washed three times with PBS and treated with a 660-nm laser irradiation (0.03 W cm−2) for 3 min. After the different treatments, the cells were observed by CLSM and detected by flow cytometry. All cells were cultured under normoxic conditions (21% O2) throughout the process. Furthermore, we detected the intracellular ROS levels under hypoxic conditions (1% O2). This operation was the same as above except that the CT26 cells were cultured under hypoxia.
Detection of intracellular hypoxia
To assess the ability of PB@PCN to relieve tumor intracellular hypoxia, the fluorogenic probe ROS-ID was used as a hypoxic sensor and detected by CLSM. CT26 cells were treated with PBS, PB, PB@PCN (40 mg L−1 in terms of PB), or a high concentration of PB@PCN (80 mg L−1 in terms of PB) for 6 h, the previous medium was removed and the cells were washed with PBS twice. Then, the cells were stained with ROS-ID and Hoechst 33342 (a nuclear dye) for 30 min. Finally, the cells were washed with PBS and observed by CLSM (λex = 543 nm, λem = 570–620 nm) and detected by flow cytometry. During the whole experiment, cells were cultured in hypoxic (1% O2) and dark conditions.
Evaluation of cellular HSP70 content
CT26 cells were seeded and cultured for 24 h under normoxic conditions (21% O2) in 6-well plates. Then, CT26 cells were incubated for 4 h at 37 °C in medium containing different NPs: PBS, PCN, PB@PCN (20 mg L−1 in terms of PCN) and a high concentration of PB@PCN (30 mg L−1 in terms of PCN). Subsequently, all cells were cultured at 43 °C for 1 h to induce high expression of HSP70. After washing with PBS, the cells were irradiated with a 660-nm laser for 5 min and cultured for another 24 h. Finally, cellular HSP70 expression was analyzed by western blot analysis.
Evaluation of cytotoxicity
Cytotoxicity was evaluated by the MTT assay. CT26 cells were seeded and cultured for 24 h in a 96-well plate at 37 °C. Following treatment with gradient concentrations of PB, PCN, or PB@PCN for 4 h, the medium was removed, fresh medium was added, and then CT26 cells were subjected to different light conditions (black, 808 nm (1.5 W cm−2, 5 min), 660 nm (0.03 W cm−2, 5 min) or 660 + 808 nm). After further incubation for 24 h, 20 μL of MTT (5 mg L−1) was added to each well and cultured for another 4 h. Afterwards, the medium containing MTT was replaced with 150 μL of DMSO. After the 96-well plates were shaken for 15 min, the optical density (OD) was recorded at 570 nm on a microplate reader. The relative cell viabilities were calculated by the following formula: cell viability (%) = OD(sample) × 100/OD(control), where OD(control) and OD(sample) are the absorbance at 570 nm in the absence and presence of sample, respectively. All cells were cultured under normoxic conditions (21% O2) throughout this process.
To verify that PB@PCN can overcome the hypoxic limitations of PDT, we further analyzed CT26 cytotoxicity under hypoxic conditions (1% O2). The process of cell treatment was the same as above except that the cells were cultured under hypoxic conditions.
Imaging in vivo
CT26 tumor-bearing BALB/c mice with a tumor volume of ∼300 mm3 were injected intravenously with PB@PCN or PB@PCN@MEM (7.5 mg kg−1 in terms of PB, 3.25 mg kg−1 in terms of PCN). At the scheduled time after injection (0 h, 4 h, 8 h, 12 h, 24 h, and 36 h), tumor imaging was carried out with a small animal imaging system (λex = 640 nm; λem = 680 nm). Moreover, mice were killed at 36 h, and the main tissues and tumors were obtained. The fluorescence distribution in the main tissues and tumors at 36 h were recorded on a small animal imaging system. For MRI, the mice were observed at 0 h, 2 h, and 12 h. For PA imaging, the tumor sites were scanned with a PA imaging system to obtain PA signals before and after injection (744 nm laser). During the imaging process, mice were anesthetized by intraperitoneal injection of 5% chloral hydrate solution. Specifically, PA imaging of blood vessels at the tumor sites in mice was conducted with a 523 nm laser.
Antitumor study and histochemical analysis
CT26 tumor-bearing BALB/c mice with a tumor volume of ∼100 mm3 were randomly divided into 6 groups (6 mice in each group): PBS, PBS+, PB+, PCN+, PB@PCN+, and PB@PCN@MEM+. First, 100 μL of each different sample solution was injected into each group of mice via the tail vein. Twelve hours after injection, all mice except those in the PBS group were irradiated with an 808 nm laser (1.5 W cm−2) for 4 min and a 660-nm laser (0.22 W cm−2) for 4 min. During treatment, the tumor sizes and body weights were recorded daily. The tumor volume (V) was calculated according to the following formula: V = 0.5 × L × W2, where L and W represent the shortest and longest diameter of the tumors, respectively. On day 14, all mice were killed, and the tumors were excised, weighed, photographed, and collected for histological analysis. In addition, the main organs (hearts, livers, spleens, lungs, and kidneys) were dissected and collected for histological analysis.
In vivo pharmacokinetics study
The pharmacokinetics of PB@PCN and PB@PCN@MEM were investigated using CT26 tumor-bearing mice with a tumor volume of ∼200 mm3. CT26 tumor-bearing mice were randomly divided into two groups with 3 mice in each group. One group was injected intravenously with PB@PCN@MEM, and the other group was injected intravenously with PB@PCN (both 7.5 mg kg−1 in terms of PB). Blood samples (10 μL) were extracted from the mouse tail veins at the scheduled time (0.5 h, 1 h, 2 h, 4 h, 8 h, and 24 h) and added to 490 μL of ultrapure water. Next, the solutions were subjected to ultrasound to obtain transparent solutions, and the NP concentrations were determined using an LS55 luminescence spectrometer. (λex = 420 nm, λem = 650 nm).
Blood biochemistry and routine blood examination
BALB/C mice were randomly divided into four groups of five mice and intravenously injected with 200 µL of PBS, PB, PB@PCN or PB@PCN@MEM solution (15 mg kg−1 in terms of PB). After 3 days, blood samples were collected in anticoagulation tubes via cardiac puncture and then analyzed by a blood biochemistry analyzer (MNCHIP Pointcare) and an auto hematology analyzer (MC-6200VET).
PDT in vivo
When the tumor volume reached ∼200 mm3, a mixture of SOSG (50 × 10−6 M, 25 μL), PB (25 μL), PCN (25 μL), PB@PCN (25 μL), or PB@PCN@MEM (25 μL) was directly injected into the tumors. The final concentration of TCPP was 25 mg/L. After 2 h, laser irradiation (660 nm, 0.22 W cm−2) was performed on each group for 4 min. Then, all the tumors were harvested and frozen-sectioned for examination.
In vivo hypoxia-inducible factor α detection
When the tumor volume reached ∼200 mm3, different samples were directly injected into the tumors. After 24 h, all mice were killed, and the tumors were collected for hypoxia-inducible factor α (HIF-α) immunohistochemical staining.
In vivo HSP70 detection
When the tumor volume reached ∼200 mm3, different samples were injected into the mice via the tail vein. After 12 h, all mice were subjected to an 808 nm laser (1.5 W cm−2) for 4 min and a 660-nm laser (0.22 W cm−2) for 4 min. After another 24 h, all mice were killed, and the tumors were collected for HSP70 immunohistochemical staining.
Statistical analysis
Significant differences were calculated via the two-tailed T-test. Statistical significance was noted as follows: *p < 0.05, **p < 0.01, ***p < 0.001.
Results and discussion
Controlled synthesis of PB@PCN
The process for the controllable synthesis of the PB@PCN nanohybrid is depicted in Fig. 1a. PB was first prepared via the one-pot method, and TEM (Fig. 1b) and SEM (Fig. S1) images of PB showed a monodisperse cube with a particle size of approximately 110 nm. The controlled synthesis of PB@PCN was achieved with the use of a syringe pump. Metal ion (Zr) and porphyrin (TCPP) ligand stock solutions were separately delivered into the PB solution under a controlled feed rate with stirring. By controlling the feed rate, the concentration of ligands in the reaction solution was controlled below the critical nucleation concentration of PCN to prevent the generation of the PCN nucleus, which was crucial for the growth of PCN with PB as the crystal nucleus. If the feeding speed was too fast (Fig. S2), the PCN nucleus would be generated in the reaction solution, and PCN would not grow with PB as the crystal nucleus. When the feeding speed was lower than the critical speed, PCN grew with PB as the nucleus. As a consequence, by controlling the amount of the feed, a series of PB@PCN nanohybrids with different PCN shell thicknesses were obtained, and the thickness of the PCN shell increased with the addition of ligands, as confirmed by the TEM and SEM images of PB@PCN (Fig. 1b, Fig. S1). The hydrodynamic size of PB@PCN increased gradually with increasing shell thickness (Fig. 1c), and as displayed in Table S1, with increasing PCN shell thickness, the size obtained from the TEM images gradually increased from 110 nm to 140 nm. The crystal phases of PB@PCN and PB were further confirmed by powder X-ray diffraction (PXRD) (Fig. S3). Then, the optical properties of the PB@PCN series were investigated by UV–vis and fluorescence spectroscopy. As shown in Fig. S4, PB@PCN had similar characteristic absorption peaks to those of PB at 720 nm and the same absorption peaks as PCN at 422, 518, 550, and 650 nm. As expected, as the PCN shell thickness increased, the characteristic absorption peaks shared with PCN were enhanced (Fig. 1d). Due to Förster resonance energy transfer (FRET) between PCN and PB, it was not surprising to observe the obvious fluorescence quenching of PB@PCN compared with that of PCN (Fig. S5).
a Schematic illustrations of the process for the controllable synthesis of the PB@PCN nanohybrid and then camouflage by the CT26 tumor cell membrane. b Hydrodynamic sizes of PB@PCN with different PCN shell thicknesses. c TEM images of PB@PCN with different PCN shell thicknesses (PB@PCN x mL means x mL ligand solutions were added into PB solution); scale bar: 100 nm. d UV–vis spectrum of PB@PCN with different PCN shell thicknesses. e STEM-HAADF image and the corresponding element mapping images of PB@PCN
Tumor cell membrane camouflage
Subsequently, to endow PB@PCN with good immune evasion and an active targeting ability, the CT26 tumor cell membrane was used to modify the surface of the NPs (PB@PCN@MEM). In Fig. S6, the TEM image of PB@PCN@MEM showed an uneven translucent layer around PB@PCN, which was thought to be cell membrane fragments. Comparing the hydrodynamic size and zeta potential of PB@PCN@MEM with those of PB@PCN (Table S2), coating of the cell membrane was further indicated Furthermore, to obtain more convincing evidence to demonstrate the successful coating with the tumor cell membrane, the protein ingredients of PB@PCN@MEM were analyzed using sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE, Fig. S7), and it was displayed that the tumor cell membrane proteins were extensively retained. Moreover, the multilayered structure of PB@PCN@MEM was detected by TEM mapping (Fig. 1e), and the distribution of the characteristic elements from inside to outside (Fe corresponding to PB, Zr to PCN, P and S to cell membrane) were very clear. In addition, infrared spectroscopy (FITC) further confirmed the multicomponent structure (Fig. S8). Finally, the PCN NPs were synthesized via a one-pot method and detected by SEM (Fig. S9).
Photothermal behavior, O2 generation and enhanced 1O2 generation in solution
Because shell thickness affects the diffusion rate of small molecules (such as O2, H2O2, and H2O) and PS loading, we speculated that the shell thickness had a great impact on the performance of the core–shell nanohybrid. An too thick shell would limit H2O2 contact with the PB core, but a too thin PCN shell would reduce PS loading and cause O2 to diffuse too quickly to be well utilized by PS, thus limiting the photodynamic effect. To select the PB@PCN nanohybrid with the optimal shell thickness, the abilities of the PB@PCN with different shell thicknesses to conduct photothermal O2 generation and enhanced 1O2 were compared in solution. The mechanism of PB@PCN nanohybrid-mediated photothermal O2 generation and enhanced PDT is shown in Fig. 2a. To evaluate the photothermal effects of PB@PCN, the temperature changes were recorded under 808 nm irradiation. As shown in Figs. S10 and S11, the PB@PCN solution temperature rose from 32 to 57 °C upon irradiation for 10 min, and PB@PCN maintained excellent photothermal conversion properties during four heating–cooling cycles. In addition, PB@PCN possessed a similar photothermal conversion ability as PB, which demonstrated that the PCN shell had little effect on the photothermal properties of the core (Fig. 2b). Furthermore, the photothermal effects of PB@PCN aqueous dispersions at various concentrations was detected, proving high concentrations corresponded to fast heating rates and high peak temperatures (Fig. 2c).
a Schematic illustration of PB@PCN-mediated photothermal O2 generation and enhanced PDT. b Temperature change as a function of time in the PBS, PCN, PB, and PB@PCN solutions irradiated with constant 808 nm laser power, and c PB@PCN solutions at different concentrations. d Detection of PB@PCN-catalyzed O2 generation with different concentrations of H2O2 (0 (1), 1.5 w% (2), 3 w% (3), and 6 w% (4)) by ([Ru(dpp)3]Cl2). e Detection of O2 generation in different solutions (PBS (1), PB@PCN 6 mL (2), PB@PCN 3 mL (3), PB@PCN 0.5 mL (4), PB (5), and PB@PCN 3 mL + 808 nm (6)). f Detection of O2 generation using a dissolved oxygen meter. g Fluorescence response of SOSG upon treatment with PB@PCN irradiated with 808 nm. h ROS generation under 660 nm light in different solutions. i 1O2 production efficiency of PB@PCN with different PCN shell thicknesses
Subsequently, the catalase-like activity of PB@PCN catalyzing H2O2 to produce O2 was evaluated. As shown in Fig. S12, after mixed solutions of PB (PB or PB@PCN with different shell thicknesses) and diluted H2O2 were incubated at 37 °C for 15 min, obvious bubbles were observed, while negligible bubbles were found in the PBS and PCN groups. To study the effect of the H2O2 concentration on PB@PCN-catalyzed O2 generation, the O2 levels in PB@PCN suspensions with different H2O2 concentrations were compared. Compared with the group without H2O2, the O2 levels in the groups with H2O2 increased significantly, and higher H2O2 concentration with higher oxygen concentration presented as the reduced fluorescence intensity of the O2 probe ([Ru(dpp)3]Cl2) (Fig. 2d, Fig. S13). To investigate the effects of the PCN shell thickness and photothermal effects on oxygen generation efficiency, both an O2 probe and a dissolved oxygen meter were used (Fig. 2e, f). They both demonstrated that the oxygen production efficiency was impeded by a PCN shell that was too thick (PB@PCN 6 mL) and was improved by photothermal treatment. We speculated that this result was caused by the PCN shell being too thick and limiting the diffusion of O2 and H2O2 instead of the thermal effect accelerating the decomposition of H2O2.
Finally, the 1O2 production capacity of PB@PCN was evaluated by the SOSG (a 1O2 probe). As shown in Fig. 2g, the fluorescence of SOSG was enhanced upon treatment with PB@PCN under 660 nm light irradiation, indicating the excellent ability of PB@PCN to produce 1O2. As shown in Fig. 2h, the presence of H2O2 made no difference in the 1O2 generation capacity of PCN, while H2O2 could observably enhance the 1O2 generation capacity of PB@PCN. The above result was ascribed to the catalase-like activity of the PB core that catalyzed H2O2 to produce O2, and this increase in O2 is beneficial for enhanced PDT. The 1O2 generation capacity of PB@PCN was obviously stronger than that of PCN in the absence of H2O2, which was possibly caused by the conjugated structure of the PB core that enhanced the light absorption and energy conversion efficiency of the PCN shell. In view of the too thick PCN shell bringing down the efficiency of O2 generation, the 1O2 generation capacity of PB@PCN with different shell thicknesses in the presence of H2O2 was studied. As shown in Fig. 2i, compared to the other two groups, the 1O2 generation efficiency in the PB@PCN 6 mL group was obviously lower, which decreased the O2-dependent 1O2 generation. However, PCN shells that are too thin would cause O2 to diffuse too quickly to be well utilized by PS, thus limiting 1O2 generation, just as the 1O2 generation efficiency in the PB@PCN 3 mL group was higher than that of the PB@PCN 0.5 mL group. Thus, to comprehensively conclude the above results, PB@PCN 3 mL had an optimal shell thickness for combined PTT/PDT therapy, which provided the best core–shell nanohybrid structure for the following experiments in vitro and in vivo. (In the subsequent studies, PB@PCN stands for PB@PCN 3 mL.)
We further studied the effect of cell membrane coating on the efficiency of heat and O2 generation. As shown in Fig. S14, PB@PCN@MEM and PB@PCN showed similar photothermal effects, demonstrating that the cell membrane coating had a negligible effect on the efficiency of heat generation. In contrast, as shown in Fig. S14, PB@PCN@MEM was less efficient than PB@PCN for O2 generation, illustrating that cell membrane coating weakens the O2 generation ability of NPs. This result was attributed to the cell membrane coating limiting the contact between H2O2 and the PB core. However, the effect on O2 generation was limited because the cell membranes were loosely and only partially coated on the NPs.
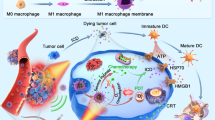
1O2 generation under normoxic and hypoxic conditions in vitro
The hypoxic TME is responsible for the limited therapeutic effect of PDT for solid tumors, as O2 is an essential element for PDT. Considering the higher level of H2O2 in the TME (100 μM to 1 mM) compared with that in normal tissues38, we then assessed the catalase-like activity of PB@PCN using [Ru(dpp)3]Cl2 to measure the intracellular O2 level. Compared with the control groups (PBS and PCN), the O2 level visibly increased when incubated with PB and PB@PCN (Fig. 3a, Fig. S15). In view of the above results, with great expectations, the 1O2 generation performance of PB@PCN in a 1% O2 atmosphere that mimics the hypoxic environment was studied33. As shown in Fig. 3b by flow analysis, after incubation with PBS, PCN and PB@PCN and then irradiation with a 660 nm laser, the fluorescence intensity of the CT26 cells in the PB@PCN group was nearly 23 greater than that of the control group, but the PCN group was only two times greater than that of the control group, implying that PB@PCN could overcome the hypoxic limitations of PDT to a certain extent. Accordingly, the PDT efficiency of PB@PCN and PCN were evaluated in the simulated hypoxic environment (1% O2 atmosphere). As illustrated in Fig. 3d, PB@PCN had a significantly higher cytotoxicity (nearly 40%) than PCN (nearly 12%) under hypoxic conditions. It was confirmed that hypoxia greatly weakened the effect of O2-dependent PDT, yet PB@PCN could effectively relieve hypoxia by triggering the decomposition of H2O2 to produce O2. Furthermore, to obtain more convincing evidence, ROS-ID was used as a fluorogenic probe for intracellular hypoxia evaluation and was detected by CLSM. As shown in Fig. 3c, PB and PB@PCN could effectively alleviate the anoxic environment in CT26 cells incubated in a 1% O2 atmosphere, and the higher the concentration of PB@PCN (HPB@PCN), the more obvious the effect of alleviation. In addition, this result was also obtained by flow cytometry analysis (Fig. S16).
a Mean fluorescence intensity (MFI) values of [Ru(dpp)3]Cl2 in cells. b Intracellular ROS detection with 660 nm irradiation under hypoxia by flow analysis. c CLSM images of intracellular hypoxia levels under 1% O2 with different treatments (blue, fluorescence of Hoechst 33342; red, fluorescence of ROS-ID hypoxia probe; overlay images). d Under hypoxia, viability of CT26 cells incubated with 660 nm irradiation. e Under normoxia, relative CT26 cell viabilities (PB 18 mg L−1, PCN 9 mg L−1). f Western blot demonstrating the HIF-α level and g the HSP level after various treatments (+ indicates the addition of 660 nm irradiation; HPB@PCN indicates the high concentration of PB@PCN). (Results are expressed as the mean ± SD of at least three independent experiments measured in triplicate. *p < 0.05, **p < 0.01, ***p < 0.001. Scale bar: 40 μm)
Then, we further investigated the effects of PB, PCN, and PB@PCN on the intracellular reactive oxygen (ROS) levels under 660 nm light irradiation using DCFH-DA (a ROS probe that emits green fluorescence after oxidation by ROS). Notably, the green fluorescence of the PBS, PCN, and PB@PCN groups was enhanced successively (Fig. S17). This phenomenon, ascribed to TCPP transferring light energy to O2, increased intracellular ROS levels directly, and PB@PCN could effectively trigger the production of O2 from H2O2 to elevate photoinduced 1O2 generation. However, it cannot be ignored that the green fluorescence of the PB group was obviously weaker than that of the PBS group, and this result can mainly be attributed to the H2O2 consumption by PB catalytic decomposition. To obtain more convincing evidence, CT26 cells were treated with different samples and analyzed by flow cytometry using DCFH-DA as a probe. We obtained consistent results without (Fig. S18) or with (Fig. S19) 660 nm laser irradiation.
Combined PTT/PDT therapy in vitro
Then, the in vitro combined PTT/PDT therapy effects of PB@PCN were investigated. First, the relative viabilities of CT26, murine embryonic fibroblast (3T3) and murine macrophage (RAW264.7) cells were evaluated by the MTT assay in the dark treated with PB, PCN, PB@PCN, and PB@PCN@MEM at different concentrations for 24 h. According to Fig. S20, the relative viabilities of all three cells remained over 90% even after incubation with high concentrations of the NPs, indicating good biocompatibility for hybrid NPs (PB@PCN and PB@PCN@MEM) and their components (PB and PCN) in the absence of light. Furthermore, considering the PDT-enhancing ability and good photothermal conversion effects of PB@PCN, the effects of PB@PCN on CT26 cell viability under different light conditions were studied (Fig. S21). First, after incubation with different NPs for 4 h, CT26 cells were treated with 808 nm or 660 nm light. Compared to PB (under 808 nm irradiation) and PCN (under 660 nm irradiation), PB@PCN showed slightly more cytotoxicity against CT26 cells, which demonstrated that PB@PCN had good PDT and PTT effects under a single light. The decreased cell viability effects under single-light irradiation resulted from catalytic O2 generation-enhanced PDT and the redshift of PB absorption by PCN shell-enhanced PTT. Second, in view of the above results, we had high expectations for PB@PCN for efficient combined PTT/PDT therapy. As expected, under 660 + 808 nm laser irradiation, compared with PB and PCN, PB@PCN presented obviously higher cytotoxicity. To further verify that combined PTT/PDT therapy could effectively improve the killing effects of PB@PCN on CT26 cells, the cytotoxicity of PB@PCN against CT26 cells under different light irradiation conditions were compared. As shown in Fig. 3e, the survival rate of cells treated with the dual laser (660 + 808 nm) was apparently lower than that of the cells treated with a single laser (660 nm or 808 nm); this result was exactly as expected. Additionally, flow cytometry with the dual fluorescence of annexin V-FITC/PI (Fig. S22) and fluorescence live/dead cell staining (Fig. S23) was performed, providing more sufficient proof for efficient combination of PTT/PDT.
Expression of HIF-α and HSP70 in vitro
We further analyzed the expression of HIF-α, which is overexpressed in hypoxic environments, after PBS, PB, and PB@PCN treatments in a 1% O2 atmosphere. As shown in Fig. 3f, Fig. S24, a marked decrease in HIF-α was observed after PB and PB@PCN treatment in the hypoxic environment, and a more significant decrease was observed after treatment with high concentrations of PB@PCN. This result was consistent with the above results, and we concluded that PB@PCN could regulate the hypoxic TME. As numerous studies have reported, HSPs are a molecular chaperone able to repair heat-denatured proteins, and their expression increases significantly upon exposure to hyperthermia to resist heat-induced apoptosis and affect the efficacy of PTT. As ROS are capable of attacking HSPs, producing ROS may be beneficial to overcome HSP-dependent tumor resistance and improve PTT efficacy. Based on this expectation, we examined the level of HSP70 in CT26 cells with different treatments via Western blotting (Fig. 3g, Fig. S24) to evaluate the impact of ROS production on the expression of HSP70. First, CT26 cells were incubated with PBS, PCN, and PB@PCN at 37 °C for 4 h and cultured for another hour at 43 °C to induce high expression levels of HSP70. Afterwards, PCN+ and PB@PCN+ were irradiated with a 660-nm laser to trigger ROS production. Compared with the cells in the absence of light, cells irradiated with light showed lower HSP70 expression levels, indicating that photoinduced ROS reduced the HSP70 content in cells.
Homotypic target and immune escape of PB@PCN@MEM
To prove the tumor cell self-recognition of PB@PCN@MEM by homologous tumor cells, the cellular internalization of PB@PCN and PB@PCN@MEM was studied by incubating the two NPs with two different cell lines, CT26 and the nontumor cell line 3T3, followed by quantitative analysis by flow cytometry (Fig. 4a, b). As we expected, in CT26 cells, the PCN fluorescence intensity of PB@PCN@MEM was significantly higher than that of PB@PCN. In 3T3 cells, the TCPP fluorescence intensity of PB@PCN@MEM was slightly lower than that of PB@PCN. This result was attributed to the decrease in the surface charge of the NPs after cell membrane coating; thus, 3T3 cells endocytosis decreased. However, since the effects of homology targeting are stronger than that of surface charge change, CT26 cells endocytosis increased. To obtain a visible result, the study of cellular internalization of the NPs was conducted with CLSM, and a consistent result was confirmed (Fig. 4c, Fig. S25). In addition, it cannot be ignored that the cell membrane coating decreased the endocytosis of the NPs into the immune cells due to the specific protein and increased negative surface charge. The immune-evading ability of PB@PCN@MEM was first examined through antiphagocytosis against murine macrophages (RAW264.7). PB@PCN without the membrane coating was used for comparison. An obvious difference was found, and PB@PCN exhibited a 2-fold greater uptake by RAW264.7 cells than PB@PCN@MEN as determined by flow cytometry (Fig. 4a, b), demonstrating the good immune escapability of PB@PCN@MEM. In addition, the influence on cytotoxicity of the tumor membrane coating against CT26 and 3T3 cells was assessed by MTT assay (Fig. 4d). As predicted, compared with PB@PCN, PB@PCN@MEM showed higher cytotoxicity against CT26 cells, but lower cytotoxicity against 3T3 cells. The above results demonstrated that the tumor cell membrane coatings gave the NPs an inherent self-targeting ability. Finally, the blood retention of PB@PCN@MEM with the CT26 cell membrane coating was measured, and bare PB@PCN was used as a control. As shown in Fig. 4e, PB@PCN@MEM cleared more slowly than PB@PCN from the blood, proving that this coating promoted the longer circulation of PB@PCN@MEM, which was conducive to better enrichment of the NPs at the tumor site.
Multimodal imaging in vivo
In general, treatment outcomes can be more effective if light-driven therapeutics are performed when agents reach the greatest accumulation at the tumor site. NPs with imaging modalities can monitor their accumulation in tumor sites during real-time systemic administration and provide guidance for treatment39. In most cases, the combination of multiple imaging modalities provides more detailed and accurate information for tumor diagnosis and treatment monitoring. Inspired by the superior ability of PB@PCN in solution, the in vivo multimodal imaging behavior of PB@PCN@MEM was further evaluated toward CT26 tumor-bearing mice. First, a FL study was performed on a small animal imaging system. As shown in Fig. 5a, an obvious fluorescence signal in the tumor region was observed 4 h after intravenous (i.v.) injection of PB@PCN@MEM. The PB@PCN@MEM fluorescence intensity reached its maximum after 8 h and remained at its maximum until 24 h, indicating that PB@PCN@MEM had a good retention effect in tumors. Subsequently, the fluorescence in the tumor site gradually decreased from 24 h to 36 h. Although PB@PCN accumulated to a certain extent in the tumor region due to the enhanced permeability and retention (EPR) effect, this accumulation was significantly weaker than that of PB@PCN@MEM. This result was ascribed to the biologically derived coating of PB@PCN@MEM, which enabled the NPs to evade the immune system and possess an intrinsic self-targeting ability, achieving a long blood circulation time and homologous tumor cell targeting simultaneously. The mice were killed at 48 h postinjection, and the major organs were harvested for ex vivo imaging, and similar trends were observed (Fig. 5a, b). In addition, the tumor-specific accumulation of PB@PCN@MEM was verified by the 3D reconstructed transillumination fluorescent image (Fig. 5c). Then, we evaluated the MRI contrast capability of PB@PCN@MEM. As shown in Fig. S26, with increasing NP concentrations, the T2-weighted signals of the PB@PCN@MEM solution gradually darkened. Next, the mice bearing CT26 tumors were i.v. injected with PB@PCN@MEM and imaged under a 4.7 T MR imager. The T2-weighted MR signal became obviously darker at the tumor site over time, suggesting the significant accumulation of NPs in the tumor upon systemic administration (Fig. 5d). Owing to the NIR photothermal effect of PB@PCN@MEM, we explored its potential for in vivo PAI and IR. Figure 5e shows the PA signal of PB@PCN@MEM at different concentrations in tubes. In vivo PAI was carried out for CT26 tumor-bearing mice after i.v. injection with PB@PCN@MEM (Fig. 5f). Due to the tumor retention of PB@PCN@MEM, the PA signals, which were detected under 744 nm irradiation in the tumor region after 12 h (Fig. 5f2), were significantly enhanced compared with those at 0 h (Fig. 5f1), and the PA signal at 12 h was approximately five times as strong as that at 0 h (Fig. S27). Surprisingly, but completely understandably, the PA signal under 744 nm laser irradiation almost coincided with that under 523 nm irradiation (Fig. 5f3, imaging of vessel). This proved that systemically administered PB@PCN@MEM though the blood circulation system entered the tumor site and penetrated into the tumor tissue by the blood vessels of the tumor site. In addition, the IR in the tumor site after i.v. injection was detected (Fig. S28), indicating that PB@PCN@MEM could accumulate in the tumor region and achieve a good IR effect. All of the above results suggested that PB@PCN@MEM has excellent tumor targeting and in vivo bioimaging ability.
a The in vivo and ex vivo fluorescence images of CT26 tumor-bearing mice after intravenous (i.v.) injection of PB@PCN or PB@PCN@MEM for various time intervals. He, Li, Sp, Lu, Ki, and Tu stand for the heart, liver, spleen, lung, kidney, and tumor, respectively. b MFI analysis of the major organs and tumors 36 h after i.v. injection. (n = 3). c In vivo 3D reconstructed transillumination fluorescence imaging 12 h after intravenous injection of PB@PCN@MEM. d T2-weighted MR images of CT26 tumor-bearing mice taken at different time points after i.v. injection of PB@PCN@MEM. e In vitro PA signal images (inset) of PB@PCN solutions with different concentrations under 744 nm laser irradiation and the corresponding PA signal intensity. f In vivo PAI of tumor tissue before (f1) and 12 h after (f2) intravenous injection of PB@PCN@MEM under 744 nm laser irradiation, and (f3) imaging of vessel in the tumor site under 523 nm laser irradiation
Biocompatibility
Biocompatibility and biosafety are critical to the application of nanomaterials in the biomedical field. Therefore, the biocompatibility and biosafety of PB@PCN and PB@PCN@MEM were evaluated through a series of characterizations. Since the stability of the NPs under physiological conditions is very important for the biomedical application of NPs in vivo, the stability of the NPs in PBS was studied before the biocompatibility study of the NPs. As shown in Fig. S29, PB@PCN@MEM was proved to have good stability and dispersion. Next, the hemocompatibility of the NPs was evaluated by the hemolysis test. From Fig. 6a, we can conclude that PB, PB@PCN and PB@PCN@MEM hardly caused hemolysis at high concentrations. Furthermore, the whole blood biochemical examination indicated that PB, PB@PCN and PB@PCN@MEM treatments had no significant effect on liver or kidney functions compared to the PBS group (Fig. 6b), and the main hematological parameters did not change significantly (Table S3). In addition, as shown in Fig. 6c, after 14 days of treatments, there was negligible variation in the average weights in the different treatment groups, except for the PBS group, which displayed significantly larger tumors causing the mice to gain weight, which indicated that our treatments barely affected the health of the mice. We also studied the effects of different treatments on the major organs. The major organs of the different treatment groups were collected after 14 days of treatment, and hematoxylin and eosin (H&E) staining was conducted (Fig. S30). There appeared to be no obvious physiological abnormalities in the major organs, including the hearts, livers, spleens, lungs, and kidneys. Collectively, these in vivo results demonstrated the good biocompatibility and low systemic toxicity of our nanomaterials.
a Hemolysis quantification of RBCs. b Heatmap of blood biochemical analysis of mice after i.v. injection with different samples. (n = 5). c The body weights and d relative tumor volumes of CT26 tumor-bearing mice with different treatments (*p < 0.05, **p < 0.01, and ***p < 0.001 were calculated by Student’s t test). e Photos of the tumors and f average tumor weights on the 14th day after treatments. g Schematic illustration of the therapeutic procedure. h H&E staining of CT26 tumors after 14 days of treatments and i apoptotic cell detection by TUNEL (green) immunofluorescent staining of CT26 tumors. (scale bar, 100 μm). j SOSG staining of the CT26 tumors for 1O2 detection (scale bar, 100 μm) after treatment with different samples and irradiation with a 660-nm laser. ( + stands for with light irradiation)
Antitumor effects
Motivated by the above study of biocompatibility in vivo, the therapeutic effect of our nanomaterials was further assessed in CT26 tumor-bearing mice. The therapeutic procedure is shown in Fig. 6g. CT26 tumor-bearing mice were randomly divided into six groups (6 mice per group): PBS, PBS+, PB+, PCN+, PB@PCN+, PB@PCN@MEM (where + stands for with 660 nm and 808 nm light irradiation). Under the guidance of the multimodal imaging studies in vivo, at 12 h post i.v. injection of the corresponding therapeutic agent, the mice in the groups with light were exposed to 808 nm and 660 nm light for 5 and 4 min, respectively. The tumor sizes were measured over the following 2 weeks (Fig. 6d), and the tumors of all mice were collected (Fig. 6e) and weighed (Fig. 6f) on the 14th day. As revealed in these results, compared with the PBS/PBS + groups, the PB + /PCN + groups exhibited a certain extent of tumor inhibition capacity mainly because of the EPR ability and PTT/PDT effects. Notably, due to the synergistic effects of PTT and enhanced PDT, the mice treated with PB@PCN + showed an excellent tumor growth inhibition effect, which was better than the PB + and PCN + treatment groups. As expected, the PB@PCN@MEM + group had the best therapeutic effect, and some tumors were even completely eliminated, which was ascribed to the tumor cell membrane coating endowing the NPs with the biological properties of homologous adhesion and immune escape. In addition to the analysis of the tumor size changes, the extracted tumors were sliced into sections for immunohistochemical assays. As revealed by H&E staining (Fig. 6h), the most severe tumor damage (including vacuoles, condensed nuclei and changed cell shapes) was displayed in the PB@PCN@MEM + group. Furthermore, immunofluorescence staining showed the greatest cell apoptosis signal (Tunnel, Fig. 6i) and the weakest cell proliferation signal (Ki67, Fig. S31) in this group.
Next, we carefully studied the detailed mechanism of the effective combined PDT/PTT therapy in vivo. To prove that PB@PCN and PB@PCN@MEM catalyze O2 production to relieve the tumor hypoxic microenvironment, HIF-α immunofluorescence staining was carried out. As illustrated in Fig. S32, a significantly reduced red fluorescence (HIF-α expression) was observed in the tumor tissues after the intratumor injection of either PB, PB@PCN, or PB@PCN@MEM. Next, the in vivo 1O2 generation was evaluated from the frozen sections of the tumor tissue after intratumoral injection of the mixtures of SOSG with PB, PCN, PB@PCN, and PB@PCN@MEM. After 660 nm laser irradiation, tumors treated with PB@PCN and PB@PCN@MEM displayed stronger green fluorescence than the tumors treated with PCN, while tumors treated with PB displayed almost no fluorescence (Fig. 6j), proving that PB@PCN and PB@PCN@MEM enhanced 1O2 generation at the tumor site. Finally, according to the results of the above cell experiments, light-induced 1O2 was capable of attacking HSPs, and the HSP70 expression levels in the tumors after different treatments were evaluated by immunofluorescent staining. As shown in Fig. S33, HSP70 expression obviously increased in the tumor after 808 + 660 nm irradiation in mice receiving an i.v. injection of PB, indicating that PB was enriched at the tumor site and PTT was conducted. In marked contrast, a much lower tumor HSP70 expression level was detected after 808 + 660 nm irradiation with PB@PCN or PB@PCN@MEM treatment, owing to the light-induced 1O2-attacked HSP70. All of these results collectively showed that PB@PCN and PB@PCN@MEM treatments not only alleviated hypoxia in the TME and improved PDT efficiency but also reduced HSPs, which are upregulated after PTT.
Conclusion
In summary, a straightforward and convenient approach for the controlled construction of heterogeneous core/shell PB@PCN nanohybrids was developed. A series of PB@PCNs with different shell thicknesses were prepared, and PB@PCN nanohybrids with the optimal thickness was used for efficient multi-image-guided combined PTT/PDT therapy of tumors. This PB@PCN nanohybrid effectively combined the advantages of both the PB core and PCN shell to access collective properties beyond the intrinsic limitations of the individual components. This nanohybrid was able to overcome the limitation of hypoxia after PDT and HSP after PTT. After further coating with a homologous tumor cell membrane, the PB@PCN@MEM nanohybrid demonstrated homotypic targeting and immune-evading capacity. Monitored by multiple imaging techniques, PB@PCN@MEM could preferentially accumulate in the tumor after injection into the tail vein. This multifunctional nanohybrid with multimodal imaging ability for the combined PTT and PDT effects will find great potential for tumor treatment.
References
Park, J., Jiang, Q., Feng, D., Mao, L. & Zhou, H. C. Size-controlled synthesis of porphyrinic metal-organic framework and functionalization for targeted photodynamic therapy. J. Am. Chem. Soc. 138, 3518–3525 (2016).
Song, G., Cheng, L., Chao, Y., Yang, K. & Liu, Z. Emerging nanotechnology and advanced materials for cancer radiation therapy. Adv. Mater. 29, 1700996 (2017).
Fan, W., Yung, B., Huang, P. & Chen, X. Nanotechnology for multimodal synergistic cancer therapy. Chem. Rev. 117, 13566–13638 (2017).
Shi, J., Kantoff, P. W., Wooster, R. & Farokhzad, O. C. Cancer nanomedicine: progress, challenges and opportunities. Nat. Rev. Cancer 17, 20–37 (2017).
Pi, F. et al. Nanoparticle orientation to control RNA loading and ligand display on extracellular vesicles for cancer regression. Nat. Nanotechnol. 13, 82–89 (2018).
He, X. Y. et al. Functional polymer/inorganic hybrid nanoparticles for macrophage targeting delivery of oligodeoxynucleotides in cancer immunotherapy. Mater. Today Chem. 4, 106–116 (2017).
Zhu, X. et al. Upconversion nanocomposite for programming combination cancer therapy by precise control of microscopic temperature. Nat. Commun. 9, 2176 (2018).
Wang, S. et al. H. A facile one-pot synthesis of a two-dimensional MoS2 /Bi2S3 composite theranostic nanosystem for multi-modality tumor imaging and therapy. Adv. Mater. 27, 2775–2782 (2015).
He, X. et al. Redox-active AIEgen-derived plasmonic and fluorescent core@shell nanoparticles for multimodality bioimaging. J. Am. Chem. Soc. 140, 6904–6911 (2018).
Wang, H. et al. A biomimetic hybrid nanoplatform for encapsulation and precisely controlled delivery of theranostic agents. Nat. Commun. 6, 10081 (2015).
Yang, Q. et al. Regulating the spatial distribution of metal nanoparticles within metal-organic frameworks to enhance catalytic efficiency. Nat. Commun. 8, 14429 (2017).
Zhang, W. et al. Mesoporous metal-organic frameworks with size-, shape-, and space-distribution-controlled pore structure. Adv. Mater. 27, 2923–2929 (2015).
Ma, X. et al. Single gold-bridged nanoprobes for identification of single point DNA mutations. Nat. Commun. 10, 836 (2019).
Lu, G. et al. Imparting functionality to a metal-organic framework material by controlled nanoparticle encapsulation. Nat. Chem. 4, 310–316 (2012).
Bin, D. S. et al. Controlling the compositional chemistry in single nanoparticles for functional hollow carbon nanospheres. J. Am. Chem. Soc. 139, 13492–13498 (2017).
Gai, S. et al. Recent advances in functional nanomaterials for light–triggered cancer therapy. Nano Today 19, 146–187 (2018).
Qi, J. et al. Light-driven transformable optical agent with adaptive functions for boosting cancer surgery outcomes. Nat. Commun. 9, 1848 (2018).
Chechetka, S. A. et al. Light-driven liquid metal nanotransformers for biomedical theranostics. Nat. Commun. 8, 15432 (2017).
Yu, X. et al. CT/MRI-guided synergistic radiotherapy and X-ray inducible photodynamic therapy using Tb-doped Gd-W-nanoscintillators. Angew. Chem. Int. Ed. 58, 2017–2022 (2019).
Ni, D. et al. Magnetic targeting of nanotheranostics enhances cerenkov radiation-induced photodynamic therapy. J. Am. Chem. Soc. 140, 14971–14979 (2018).
Zhu, H., Cheng, P., Chen, P. & Pu, K. Recent progress in the development of near-infrared organic photothermal and photodynamic nanotherapeutics. Biomater. Sci. 6, 746–765 (2018).
Guo, W., Guo, C., Zheng, N., Sun, T. & Liu, S. Csx WO3 nanorods coated with polyelectrolyte multilayers as a multifunctional nanomaterial for bimodal imaging-guided photothermal/photodynamic cancer treatment. Adv. Mater. 29, 1604157 (2017).
Cai, Y. et al. Diketopyrrolopyrrole-triphenylamine organic nanoparticles as multifunctional reagents for photoacoustic imaging-guided photodynamic/photothermal synergistic tumor therapy. ACS Nano. 11, 1054–1063 (2017).
Goel, S. et al. Activatable hybrid nanotheranostics for tetramodal imaging and synergistic photothermal/photodynamic therapy. Adv. Mater. 30, 1704367 (2018).
Liu, Y. et al. Modulating hypoxia via nanomaterials chemistry for efficient treatment of solid tumors. Acc. Chem. Res. 51, 2502–2511 (2018).
Yang, G. et al. Hollow MnO2 as a tumor-microenvironment-responsive biodegradable nano-platform for combination therapy favoring antitumor immune responses. Nat. Commun. 8, 902 (2017).
Liu, W. L. et al. Aggressive man-made red blood cells for hypoxia-resistant photodynamic therapy. Adv. Mater. 30, e1802006 (2018).
Kim, J. et al. Continuous O2-evolving MnFe2O4 nanoparticle-anchored mesoporous silica nanoparticles for efficient photodynamic therapy in hypoxic cancer. J. Am. Chem. Soc. 139, 10992–10995 (2017).
Lan, G. et al. Nanoscale metal-organic framework overcomes hypoxia for photodynamic therapy primed cancer immunotherapy. J. Am. Chem. Soc. 140, 5670–5673 (2018).
Chen, W. H. et al. Overcoming the heat endurance of tumor cells by interfering with the anaerobic glycolysis metabolism for improved photothermal therapy. ACS Nano. 11, 1419–1431 (2017).
Chu, K. F. & Dupuy, D. E. Thermal ablation of tumours: biological mechanisms and advances in therapy. Nat. Rev. Cancer 14, 199–208 (2014).
Yang, Y. et al. 1D Coordination polymer nanofibers for low-temperature photothermal therapy. Adv. Mater. 29, 199 (2017).
Li, S. Y. et al. Cancer cell membrane camouflaged cascade bioreactor for cancer targeted starvation and photodynamic therapy. ACS Nano. 11, 7006–7018 (2017).
Xie, W. et al. Cancer cell membrane camouflaged nanoparticles to realize starvation therapy together with checkpoint blockades for enhancing cancer therapy. ACS Nano. 13, 2849–2857 (2019).
Parodi, A. et al. Synthetic nanoparticles functionalized with biomimetic leukocyte membranes possess cell-like functions. Nat. Nanotechnol. 8, 61–68 (2013).
Tang, Z. et al. Pyroelectric nanoplatform for NIR-II-triggered photothermal therapy with simultaneous pyroelectric dynamic therapy. Mater. Horiz. 5, 946–952 (2018).
Chen, H., Tian, J., He, W. & Guo, Z. H2O2-activatable and O2-evolving nanoparticles for highly efficient and selective photodynamic therapy against hypoxic tumor cells. J. Am. Chem. Soc. 137, 1539–1547 (2015).
Liu, Y. et al. One-dimensional Fe2P acts as a fenton agent in response to NIR II light and ultrasound for deep tumor synergetic theranostics. Angew. Chem. Int. Ed. 58, 2407–2412 (2019).
Liu, Y., Bhattarai, P., Dai, Z. & Chen, X. Photothermal therapy and photoacoustic imaging via nanotheranostics in fighting cancer. Chem. Soc. Rev. 48, 2053–2108 (2019).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (51833007, 51873161, and 51690152). All of the animal experiments were conducted under protocols approved by the Institutional Animal Care and Use Committee (IACUC) of the Animal Experiment Center of Wuhan University (Wuhan, China).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheng, Q., Li, ZH., Sun, YX. et al. Controlled synthesis of a core-shell nanohybrid for effective multimodal image-guided combined photothermal/photodynamic therapy of tumors. NPG Asia Mater 11, 63 (2019). https://doi.org/10.1038/s41427-019-0164-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41427-019-0164-4
This article is cited by
-
Near-infrared photodynamic and photothermal co-therapy based on organic small molecular dyes
Journal of Nanobiotechnology (2023)
-
Mitochondria-targeting multifunctional nanoplatform for cascade phototherapy and hypoxia-activated chemotherapy
Journal of Nanobiotechnology (2022)
-
Synergistic photothermal-photodynamic-chemotherapy toward breast cancer based on a liposome-coated core–shell AuNS@NMOFs nanocomposite encapsulated with gambogic acid
Journal of Nanobiotechnology (2022)
-
Aza-BODIPY-based phototheranostic nanoagent for tissue oxygen auto-adaptive photodynamic/photothermal complementary therapy
Nano Research (2022)