Gastrointestinal Endoscopy ( IF 7.7 ) Pub Date : 2018-11-29 , DOI: 10.1016/j.gie.2018.11.023 Lobke Desomer , David J. Tate , Farzan F. Bahin , Halim Awadie , Brian Chiang , Bronte Holt , Karen Byth , Michael J. Bourke
|
Background and Aims
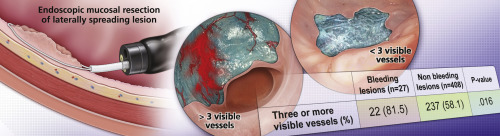
Clinically significant post-EMR bleeding (CSPEB) is the most-frequent serious adverse event after EMR of large laterally spreading colonic lesions (LSLs). There is no proven prophylactic therapy, and it remains a significant drawback of EMR. We aimed to systematically describe and evaluate the features of the post-EMR mucosal defect (PED) and their relationship to CSPEB.
Methods
A prospective study of LSLs referred for EMR at a tertiary center was performed. PEDs without visible features were recorded as bland blue. Nonbland blue (NBB) PED features included size, number, and herniation of submucosal vessels and presence of submucosal hemorrhage, fibrosis, fat, and exposed muscle. NBB PEDs were analyzed for association with CSPEB, defined as bleeding occurring after completion of the procedure necessitating readmission or reintervention.
Results
From April 2012 to May 2017, 501 lesions in 501 patients were eligible for analysis. The frequency of CSPEB was 30 of 501 (6.0%). More than or equal to 3 visible vessels was a significant predictor of CSPEB (P = .016). None of the following showed a significant correlation with CSPEB: presence of visible vessels, their diameter, herniation, or other nonvascular PED features. Submucosal vessels were more common in the left-sided colon segment (88.6% vs 78.3%, P = .004) and were significantly larger (20.8% vs 12.1% ≥1 mm, P = .037), more numerous (median 4 vessels [interquartile range, 2-7] vs 2 vessels [interquartile range, 1-4], P < .001), and more often herniated (32% vs 22.2%, P = .022).
Conclusions
More than or equal to 3 visible vessels within the PED may be predictive for CSPEB and may define a target group for real-time prophylactic intervention. No other endoscopically visible features of the PEDs were predictive of CSPEB. (Clinical trial registration number: NCT03117400.)
中文翻译:

对EMR后缺陷的系统描述,以识别结肠内EMR后临床上具有重大临床意义的出血的危险因素
背景和目标
具有临床意义的EMR后大出血(CSPEB)是大横向扩散结肠病变(LSL)EMR之后最常见的严重不良事件。没有经过验证的预防性治疗,它仍然是EMR的重大缺陷。我们旨在系统地描述和评估EMR后黏膜缺损(PED)的特征及其与CSPEB的关系。
方法
对在第三中心进行EMR的LSL进行了前瞻性研究。没有可见特征的PED被记录为淡蓝色。浓淡蓝(NBB)PED功能包括粘膜下血管的大小,数量和突出,以及粘膜下出血,纤维化,脂肪和裸露的肌肉。分析了NBB PED与CSPEB的相关性,CSPEB定义为在需要再次入院或再次干预的程序完成后发生的出血。
结果
从2012年4月至2017年5月,有501例患者的501个病灶符合分析条件。CSPEB的频率为501(6.0%)中的30。大于或等于3个可见血管是CSPEB的重要预测因子(P = .016 )。以下各项均未显示与CSPEB显着相关:可见血管的存在,它们的直径,疝或其他非血管性PED特征。粘膜下血管在左侧结肠段更常见(88.6%vs 78.3%,P = .004),并且明显更大(20.8%vs 12.1%≥1mm,P = .037),数量更多(中位数4个血管) [四分位间距2-7]比2血管[四分位间距1-4],P <.001),并且更常出现疝(32%比22.2%,P = .022)。
结论
PED内大于或等于3个可见血管可预测CSPEB,并可为实时预防性干预定义目标人群。PED的其他内窥镜可见特征均不能预测CSPEB。(临床试验注册号:NCT03117400。)



























 京公网安备 11010802027423号
京公网安备 11010802027423号