Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Intensification with dipeptidyl peptidase-4 inhibitor, insulin, or thiazolidinediones and risks of all-cause mortality, cardiovascular diseases, and severe hypoglycemia in patients on metformin-sulfonylurea dual therapy: A retrospective cohort study.
PLOS Medicine ( IF 15.8 ) Pub Date : 2019-12-26 , DOI: 10.1371/journal.pmed.1002999 Carlos K H Wong 1 , Kenneth K C Man 2, 3 , Margaret Shi 1 , Esther W Chan 2 , Chu Wa Ho 1 , Emily T Y Tse 1 , Ian C K Wong 2, 3 , Cindy L K Lam 1
PLOS Medicine ( IF 15.8 ) Pub Date : 2019-12-26 , DOI: 10.1371/journal.pmed.1002999 Carlos K H Wong 1 , Kenneth K C Man 2, 3 , Margaret Shi 1 , Esther W Chan 2 , Chu Wa Ho 1 , Emily T Y Tse 1 , Ian C K Wong 2, 3 , Cindy L K Lam 1
Affiliation
|
BACKGROUND
Although patients with type 2 diabetes mellitus (T2DM) may fail to achieve adequate hemoglobin A1c (HbA1c) control despite metformin-sulfonylurea (Met-SU) dual therapy, a third-line glucose-lowering medication-including dipeptidyl peptidase-4 inhibitor (DPP4i), insulin, or thiazolidinedione (TZD)-can be added to achieve this. However, treatment effects of intensification with the medications on the risk of severe hypoglycemia (SH), cardiovascular disease (CVD), and all-cause mortality are uncertain. Study aim was to compare the risks of all-cause mortality, CVD, and SH among patients with T2DM on Met-SU dual therapy intensified with DPP4i, insulin, or TZD.
METHODS AND FINDINGS
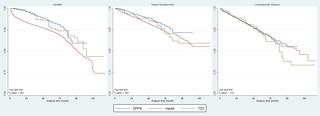
We analyzed a retrospective cohort data of 17,293 patients with T2DM who were free from CVD and on Met-SU dual therapy and who were intensified with DPP4i (n = 8,248), insulin (n = 6,395), or TZD (n = 2,650) from 2006 to 2017. Propensity-score weighting was used to balance out baseline covariates across groups. Hazard ratios (HRs) for all-cause mortality, CVD, and SH were assessed using Cox proportional hazard models. Mean age of all patients was 58.56 ± 11.41 years. All baseline covariates achieved a balance across the 3 groups. Over a mean follow-up period of 34 months with 49,299 person-years, cumulative incidences of all-cause mortality, SH, and CVD were 0.061, 0.119, and 0.074, respectively. Patients intensified with insulin had higher risk of all-cause mortality (HR = 2.648, 95% confidence interval [CI] 2.367-2.963, p < 0.001; 2.352, 95% CI 2.123-2.605, p < 0.001) than those intensified with TZD and DPP4i, respectively. Insulin users had the greatest risk of SH (HR = 1.198, 95% CI 1.071-1.340, p = 0.002; 1.496, 95% CI 1.342-1.668, p < 0.001) compared with TZD and DPP4i users, respectively. Comparing between TZDs and DPP4i, TZDs were associated with a higher risk of SH (HR = 1.249, 95% CI 1.099-1.419, p < 0.001) but not all-cause mortality (HR = 0.888, 95% CI 0.776-1.016, p = 0.084) or CVD (HR = 1.005, 95% CI 0.915-1.104, p = 0.925). Limitations of this study included the lack of data regarding lifestyle, drug adherence, time-varying factors, patients' motivation, and cost considerations. A limited duration of patients intensifying with TZD might also weaken the strength of study results.
CONCLUSIONS
Our results indicated that, for patients with T2DM who are on Met-SU dual therapy, the addition of DPP4i was a preferred third-line medication among 3 options, with the lowest risks of mortality and SH and posing no increased risk for CVD events when compared to insulin and TZD. Intensification with insulin had the greatest risk of mortality and SH events.
中文翻译:

二甲双胍-磺脲类双重疗法患者接受二肽基肽酶-4抑制剂,胰岛素或噻唑烷二酮类药物的强化治疗以及全因死亡率,心血管疾病和严重低血糖的风险:一项回顾性队列研究。
背景尽管尽管采用二甲双胍-磺脲类药物(Met-SU)双重治疗,但2型糖尿病(T2DM)患者可能无法实现足够的血红蛋白A1c(HbA1c)控制,但三线降糖药物包括二肽基肽酶4抑制剂可以添加DPP4i),胰岛素或噻唑烷二酮(TZD)来达到此目的。但是,用药物强化对严重低血糖(SH),心血管疾病(CVD)和全因死亡率的风险的治疗效果尚不确定。研究目的是比较接受DPP4i,胰岛素或TZD强化治疗的Met-SU双重治疗的T2DM患者的全因死亡率,CVD和SH的风险。方法和研究结果我们回顾性分析了17293例无CVD且接受Met-SU双重治疗且经DPP4i强化治疗的T2DM患者(n = 8)。248),胰岛素(n = 6,395)或TZD(n = 2,650)从2006年至2017年。倾向得分加权用于平衡各组之间的基线协变量。使用Cox比例风险模型评估了全因死亡率,CVD和SH的风险比(HRs)。所有患者的平均年龄为58.56±11.41岁。所有基线协变量在3组之间均达到了平衡。在平均随访期34个月(49,299人年)中,全因死亡率,SH和CVD的累积发生率分别为0.061、0.119和0.074。胰岛素强化患者的全因死亡率较高(HR = 2.648,95%置信区间[CI] 2.367-2.963,p <0.001; 2.352,95%CI 2.123-2.605,p <0.001)和DPP4i。胰岛素使用者发生SH的风险最大(HR = 1.198,95%CI 1.071-1.340,p = 0.002;与TZD和DPP4i用户相比,分别为1.496、95%CI 1.342-1.668,p <0.001)。与TZD和DPP4i进行比较,TZD与SH的风险更高(HR = 1.249,95%CI 1.099-1.419,p <0.001),但不是全因死亡率(HR = 0.888,95%CI 0.776-1.016,p = 0.084)或CVD(HR = 1.005,95%CI 0.915-1.104,p = 0.925)。该研究的局限性包括缺乏有关生活方式,药物依从性,时变因素,患者动机和成本考虑因素的数据。TZD强化患者的有限持续时间也可能削弱研究结果的强度。结论我们的结果表明,对于接受Met-SU双重治疗的T2DM患者,在3种选择中,首选DPP4i是三线药物,与胰岛素和TZD相比,具有最低的死亡和SH风险,并且不会增加CVD事件的风险。胰岛素强化具有最大的死亡和SH事件风险。
更新日期:2020-01-14
中文翻译:

二甲双胍-磺脲类双重疗法患者接受二肽基肽酶-4抑制剂,胰岛素或噻唑烷二酮类药物的强化治疗以及全因死亡率,心血管疾病和严重低血糖的风险:一项回顾性队列研究。
背景尽管尽管采用二甲双胍-磺脲类药物(Met-SU)双重治疗,但2型糖尿病(T2DM)患者可能无法实现足够的血红蛋白A1c(HbA1c)控制,但三线降糖药物包括二肽基肽酶4抑制剂可以添加DPP4i),胰岛素或噻唑烷二酮(TZD)来达到此目的。但是,用药物强化对严重低血糖(SH),心血管疾病(CVD)和全因死亡率的风险的治疗效果尚不确定。研究目的是比较接受DPP4i,胰岛素或TZD强化治疗的Met-SU双重治疗的T2DM患者的全因死亡率,CVD和SH的风险。方法和研究结果我们回顾性分析了17293例无CVD且接受Met-SU双重治疗且经DPP4i强化治疗的T2DM患者(n = 8)。248),胰岛素(n = 6,395)或TZD(n = 2,650)从2006年至2017年。倾向得分加权用于平衡各组之间的基线协变量。使用Cox比例风险模型评估了全因死亡率,CVD和SH的风险比(HRs)。所有患者的平均年龄为58.56±11.41岁。所有基线协变量在3组之间均达到了平衡。在平均随访期34个月(49,299人年)中,全因死亡率,SH和CVD的累积发生率分别为0.061、0.119和0.074。胰岛素强化患者的全因死亡率较高(HR = 2.648,95%置信区间[CI] 2.367-2.963,p <0.001; 2.352,95%CI 2.123-2.605,p <0.001)和DPP4i。胰岛素使用者发生SH的风险最大(HR = 1.198,95%CI 1.071-1.340,p = 0.002;与TZD和DPP4i用户相比,分别为1.496、95%CI 1.342-1.668,p <0.001)。与TZD和DPP4i进行比较,TZD与SH的风险更高(HR = 1.249,95%CI 1.099-1.419,p <0.001),但不是全因死亡率(HR = 0.888,95%CI 0.776-1.016,p = 0.084)或CVD(HR = 1.005,95%CI 0.915-1.104,p = 0.925)。该研究的局限性包括缺乏有关生活方式,药物依从性,时变因素,患者动机和成本考虑因素的数据。TZD强化患者的有限持续时间也可能削弱研究结果的强度。结论我们的结果表明,对于接受Met-SU双重治疗的T2DM患者,在3种选择中,首选DPP4i是三线药物,与胰岛素和TZD相比,具有最低的死亡和SH风险,并且不会增加CVD事件的风险。胰岛素强化具有最大的死亡和SH事件风险。

























 京公网安备 11010802027423号
京公网安备 11010802027423号