当前位置:
X-MOL 学术
›
JAMA Psychiatry
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Long-term Changes in Cognitive Functioning in Individuals With Psychotic Disorders: Findings From the Suffolk County Mental Health Project.
JAMA Psychiatry ( IF 25.8 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamapsychiatry.2019.3993 Anne-Kathrin J Fett 1, 2, 3 , Eva Velthorst 4, 5 , Abraham Reichenberg 2, 4, 5 , Camilo J Ruggero 6 , Jennifer L Callahan 6 , Laura J Fochtmann 7 , Gabrielle A Carlson 7 , Greg Perlman 7 , Evelyn J Bromet 7 , Roman Kotov 7
JAMA Psychiatry ( IF 25.8 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamapsychiatry.2019.3993 Anne-Kathrin J Fett 1, 2, 3 , Eva Velthorst 4, 5 , Abraham Reichenberg 2, 4, 5 , Camilo J Ruggero 6 , Jennifer L Callahan 6 , Laura J Fochtmann 7 , Gabrielle A Carlson 7 , Greg Perlman 7 , Evelyn J Bromet 7 , Roman Kotov 7
Affiliation
|
Importance
It remains uncertain whether people with psychotic disorders experience progressive cognitive decline or normal cognitive aging after first hospitalization. This information is essential for prognostication in clinical settings, deployment of cognitive remediation, and public health policy.
Objective
To examine long-term cognitive changes in individuals with psychotic disorders and to compare age-related differences in cognitive performance between people with psychotic disorders and matched control individuals (ie, individuals who had never had psychotic disorders).
Design, Setting, and Participants
The Suffolk County Mental Health Project is an inception cohort study of first-admission patients with psychosis. Cognitive functioning was assessed 2 and 20 years later. Patients were recruited from the 12 inpatient facilities of Suffolk County, New York. At year 20, the control group was recruited by random digit dialing and matched to the clinical cohort on zip code and demographics. Data were collected between September 1991 and July 2015. Analysis began January 2016.
Main Outcomes and Measures
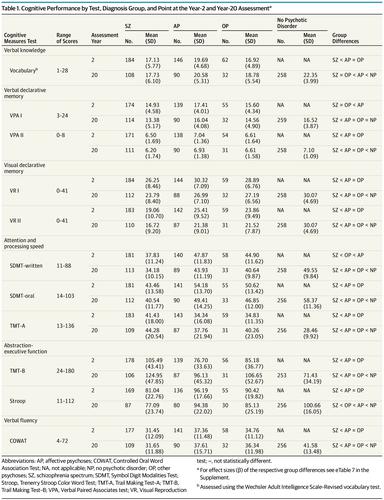
Change in cognitive functioning in 6 domains: verbal knowledge (Wechsler Adult Intelligence Scale-Revised vocabulary test), verbal declarative memory (Verbal Paired Associates test I and II), visual declarative memory (Visual Reproduction test I and II), attention and processing speed (Symbol Digit Modalities Test-written and oral; Trail Making Test [TMT]-A), abstraction-executive function (Trenerry Stroop Color Word Test; TMT-B), and verbal fluency (Controlled Oral Word Association Test).
Results
A total of 705 participants were included in the analyses (mean [SD] age at year 20, 49.4 [10.1] years): 445 individuals (63.1%) had psychotic disorders (211 with schizophrenia spectrum [138 (65%) male]; 164 with affective psychoses [76 (46%) male]; 70 with other psychoses [43 (61%) male]); and 260 individuals (36.9%) in the control group (50.5 [9.0] years; 134 [51.5%] male). Cognition in individuals with a psychotic disorder declined on all but 2 tests (average decline: d = 0.31; range, 0.17-0.54; all P < .001). Cognitive declines were associated with worsening vocational functioning (Visual Reproduction test II: r = 0.20; Symbol Digit Modalities Test-written: r = 0.25; Stroop: r = 0.24; P < .009) and worsening negative symptoms (avolition: Symbol Digit Modalities Test-written: r = -0.24; TMT-A: r = -0.21; Stroop: r = -0.21; all P < .009; inexpressivity: Stroop: r = -0.22; P < .009). Compared with control individuals, people with psychotic disrders showed age-dependent deficits in verbal knowledge, fluency, and abstraction-executive function (vocabulary: β = -0.32; Controlled Oral Word Association Test: β = -0.32; TMT-B: β = 0.23; all P < .05), with the largest gap among participants 50 years or older.
Conclusions and Relevance
In individuals with psychotic disorders, most cognitive functions declined over 2 decades after first hospitalization. Observed declines were clinically significant. Some declines were larger than expected due to normal aging, suggesting that cognitive aging in some domains may be accelerated in this population. If confirmed, these findings would highlight cognition as an important target for research and treatment during later phases of psychotic illness.
中文翻译:

精神病患者认知功能的长期变化:萨福克郡心理健康项目的发现。
重要性首次住院后,精神病患者是否会经历进行性认知功能减退或正常的认知衰老尚不确定。这些信息对于临床环境的预后,认知治疗的部署以及公共卫生政策至关重要。目的研究精神病患者的长期认知变化,比较精神病患者和相匹配的对照个体(即从未患过精神病的个体)在认知能力上与年龄相关的差异。设计,环境和参与者萨福克县精神卫生项目是对首次入院的精神病患者进行的一项队列研究。认知功能在2年和20年后进行评估。患者是从纽约萨福克县的12个住院机构招募的。在第20年,通过随机数字拨号招募了对照组,并与邮政编码和人口统计学的临床队列相匹配。数据收集于1991年9月至2015年7月之间。分析于2016年1月开始。主要结果和措施认知功能在6个领域的变化:口头知识(韦氏成人智力测验修订的词汇量测试),口头陈述性记忆(口头成对联想测验I和II),视觉声明式记忆(视觉再现测试I和II),注意力和处理速度(符号数字模态的书面和口头测试; Trail制作测试[TMT] -A),抽象执行功能(Trenerry Stroop彩色文字测试); TMT-B)和口语流利度(受控口语联想测试)。结果分析共纳入705名参与者(20岁时的平均[SD]年龄,49.4 [10.1]岁):445名患者(63.1%)患有精神病(211名精神分裂症患者[138名男性(65%))] ; 164例患有情感性精神病的患者[76(46%)男性]; 70例患有其他精神病的患者[43(61%)男性]);对照组中有260人(占36.9%)(50.5 [9.0]岁;男性134 [51.5%])。除2项测试外,精神病患者的认知均下降(平均下降:d = 0.31;范围为0.17-0.54;所有P <0.001)。认知能力下降与职业功能恶化有关(视觉再现测试II:r = 0.20;符号数字模态:书面试验:r = 0.25; Stroop:r = 0.24; P <.009)和消极症状(恶化:符号数字模态)经测试编写:r = -0.24; TMT-A:r = -0.21; Stroop:r = -0.21;全部P <.009; 表情不足:Stroop:r = -0.22;P <.009)。与对照组相比,精神病患者的语言知识,流利程度和抽象执行功能存在年龄依赖性缺陷(词汇:β= -0.32;受控口语联想测试:β= -0.32; TMT-B:β= 0.23;所有P <.05),在50岁或50岁以上的参与者中差距最大。结论与相关性在患有精神病的个体中,大多数的认知功能在首次住院后的20年中都下降了。观察到的下降具有临床意义。由于正常的衰老,一些下降比预期的要大,这表明该人群中某些领域的认知老化可能会加速。如果确认,
更新日期:2020-04-01
中文翻译:

精神病患者认知功能的长期变化:萨福克郡心理健康项目的发现。
重要性首次住院后,精神病患者是否会经历进行性认知功能减退或正常的认知衰老尚不确定。这些信息对于临床环境的预后,认知治疗的部署以及公共卫生政策至关重要。目的研究精神病患者的长期认知变化,比较精神病患者和相匹配的对照个体(即从未患过精神病的个体)在认知能力上与年龄相关的差异。设计,环境和参与者萨福克县精神卫生项目是对首次入院的精神病患者进行的一项队列研究。认知功能在2年和20年后进行评估。患者是从纽约萨福克县的12个住院机构招募的。在第20年,通过随机数字拨号招募了对照组,并与邮政编码和人口统计学的临床队列相匹配。数据收集于1991年9月至2015年7月之间。分析于2016年1月开始。主要结果和措施认知功能在6个领域的变化:口头知识(韦氏成人智力测验修订的词汇量测试),口头陈述性记忆(口头成对联想测验I和II),视觉声明式记忆(视觉再现测试I和II),注意力和处理速度(符号数字模态的书面和口头测试; Trail制作测试[TMT] -A),抽象执行功能(Trenerry Stroop彩色文字测试); TMT-B)和口语流利度(受控口语联想测试)。结果分析共纳入705名参与者(20岁时的平均[SD]年龄,49.4 [10.1]岁):445名患者(63.1%)患有精神病(211名精神分裂症患者[138名男性(65%))] ; 164例患有情感性精神病的患者[76(46%)男性]; 70例患有其他精神病的患者[43(61%)男性]);对照组中有260人(占36.9%)(50.5 [9.0]岁;男性134 [51.5%])。除2项测试外,精神病患者的认知均下降(平均下降:d = 0.31;范围为0.17-0.54;所有P <0.001)。认知能力下降与职业功能恶化有关(视觉再现测试II:r = 0.20;符号数字模态:书面试验:r = 0.25; Stroop:r = 0.24; P <.009)和消极症状(恶化:符号数字模态)经测试编写:r = -0.24; TMT-A:r = -0.21; Stroop:r = -0.21;全部P <.009; 表情不足:Stroop:r = -0.22;P <.009)。与对照组相比,精神病患者的语言知识,流利程度和抽象执行功能存在年龄依赖性缺陷(词汇:β= -0.32;受控口语联想测试:β= -0.32; TMT-B:β= 0.23;所有P <.05),在50岁或50岁以上的参与者中差距最大。结论与相关性在患有精神病的个体中,大多数的认知功能在首次住院后的20年中都下降了。观察到的下降具有临床意义。由于正常的衰老,一些下降比预期的要大,这表明该人群中某些领域的认知老化可能会加速。如果确认,


























 京公网安备 11010802027423号
京公网安备 11010802027423号