当前位置:
X-MOL 学术
›
JACC Cardiovasc. Inte.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Navigating the "Optimal Implantation Depth" With a Self-Expandable TAVR Device in Daily Clinical Practice.
JACC: Cardiovascular Interventions ( IF 11.3 ) Pub Date : 2019-12-05 , DOI: 10.1016/j.jcin.2019.07.048 Kerstin Piayda 1 , Katharina Hellhammer 1 , Verena Veulemans 1 , Horst Sievert 2 , Sameer Gafoor 3 , Shazia Afzal 1 , Inga Hennig 1 , Matthias Makosch 1 , Amin Polzin 1 , Christian Jung 1 , Ralf Westenfeld 1 , Malte Kelm 4 , Tobias Zeus 1
JACC: Cardiovascular Interventions ( IF 11.3 ) Pub Date : 2019-12-05 , DOI: 10.1016/j.jcin.2019.07.048 Kerstin Piayda 1 , Katharina Hellhammer 1 , Verena Veulemans 1 , Horst Sievert 2 , Sameer Gafoor 3 , Shazia Afzal 1 , Inga Hennig 1 , Matthias Makosch 1 , Amin Polzin 1 , Christian Jung 1 , Ralf Westenfeld 1 , Malte Kelm 4 , Tobias Zeus 1
Affiliation
|
OBJECTIVES
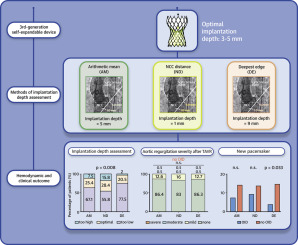
This study sought to predict whether different methods of calculating the implantation depth (ID) influence clinical and hemodynamic outcome reporting in patients undergoing transcatheter aortic valve replacement (TAVR) with a self-expandable device.
BACKGROUND
Different approaches exist to calculate the ID, which may influence uniform and reliable reporting because the updated Valve Academic Research Consortium (VARC-2) criteria do not provide specific instructions.
METHODS
The clinical and hemodynamic outcomes of 258 patients undergoing TAVR with a third-generation self-expandable device were analyzed with regard to the method used to assess the ID as follows: arithmetic mean, the arithmetic mean of the measured distances from the noncoronary cusp and the left coronary cusp to the distal prosthesis end; noncoronary cusp distance, the distance from the noncoronary cusp to the distal prosthesis end; and deepest edge, the deepest edge of the distal prosthesis end.
RESULTS
Regardless of the measurement method, the optimal ID (OID) was reached in <30% (arithmetic mean, 25.4%; noncoronary cusp distance, 28.4%; deepest edge, 20.5%; p = 0.008). The deepest edge method is the most stringent to differentiate the relevant outcome parameters, such as the need for permanent pacemaker implantation (OID 3.7% vs. no OID 14.6%; p = 0.033). The hemodynamic outcome (i.e., mean pressure gradient reduction after TAVR: OID 7.4 ± 3.4 mm Hg vs. no OID 8.3 ± 4.0 mm Hg; p = 0.093) was not affected.
CONCLUSIONS
The OID was reached in <30% of TAVR procedures. The various methods applied for ID calculation significantly influence the outcome reporting and do not allow a uniform perception of the ID. (Multi Modal Cardiac Imaging Prior Transcatheter Aortic Valve Implantation; NCT01805739).
中文翻译:

在日常临床实践中,使用自扩展TAVR设备浏览“最佳植入深度”。
目的本研究试图预测在使用自扩张装置经导管主动脉瓣置换术(TAVR)的患者中,不同的计算植入深度(ID)的方法是否会影响临床和血液动力学结果报告。背景技术存在不同的方法来计算ID,这可能影响统一和可靠的报告,因为更新的Valve学术研究协会(VARC-2)标准未提供特定的说明。方法对258例接受第三代自扩张式装置TAVR的患者的临床和血液动力学结果进行了分析,其评估ID的方法如下:算术平均值,距非冠状动脉尖的测量距离的算术平均值和左冠状动脉尖到假体远端;非冠状牙尖距离 从非冠状尖端到假体远端的距离;最深的边缘,即远端假体末端的最深边缘。结果无论采用哪种测量方法,均达到最佳ID(OID)的<30%(算术平均值为25.4%;非冠状牙尖距离为28.4%;最深边缘为20.5%; p = 0.008)。最深的边缘方法是区分相关结果参数的最严格方法,例如需要永久性起搏器植入(OID 3.7%对比无OID 14.6%; p = 0.033)。血流动力学结果(即TAVR后平均压力梯度降低:OID 7.4±3.4 mm Hg与无OID 8.3±4.0 mm Hg; p = 0.093)不受影响。结论在TAVR程序的<30%内达到了OID。用于ID计算的各种方法会显着影响结果报告,并且不能统一理解ID。(多模态心脏成像在先行导管主动脉瓣植入; NCT01805739)。
更新日期:2019-12-11
中文翻译:

在日常临床实践中,使用自扩展TAVR设备浏览“最佳植入深度”。
目的本研究试图预测在使用自扩张装置经导管主动脉瓣置换术(TAVR)的患者中,不同的计算植入深度(ID)的方法是否会影响临床和血液动力学结果报告。背景技术存在不同的方法来计算ID,这可能影响统一和可靠的报告,因为更新的Valve学术研究协会(VARC-2)标准未提供特定的说明。方法对258例接受第三代自扩张式装置TAVR的患者的临床和血液动力学结果进行了分析,其评估ID的方法如下:算术平均值,距非冠状动脉尖的测量距离的算术平均值和左冠状动脉尖到假体远端;非冠状牙尖距离 从非冠状尖端到假体远端的距离;最深的边缘,即远端假体末端的最深边缘。结果无论采用哪种测量方法,均达到最佳ID(OID)的<30%(算术平均值为25.4%;非冠状牙尖距离为28.4%;最深边缘为20.5%; p = 0.008)。最深的边缘方法是区分相关结果参数的最严格方法,例如需要永久性起搏器植入(OID 3.7%对比无OID 14.6%; p = 0.033)。血流动力学结果(即TAVR后平均压力梯度降低:OID 7.4±3.4 mm Hg与无OID 8.3±4.0 mm Hg; p = 0.093)不受影响。结论在TAVR程序的<30%内达到了OID。用于ID计算的各种方法会显着影响结果报告,并且不能统一理解ID。(多模态心脏成像在先行导管主动脉瓣植入; NCT01805739)。



























 京公网安备 11010802027423号
京公网安备 11010802027423号