The Lancet Psychiatry ( IF 64.3 ) Pub Date : 2019-12-08 , DOI: 10.1016/s2215-0366(19)30404-3 Senthil Amudhan 1 , Gopalkrishna Gururaj 1 , Mathew Varghese 2 , Vivek Benegal 2 , Girish Nagaraja Rao 1 , David Vincent Sheehan 3 , Arun Mahadeo Kokane 4 , Bir Singh Chavan 5 , Pronob Kumar Dalal 6 , Daya Ram 7 , Kangkan Pathak 8 , Raj Kumar Lenin Singh 9 , Lokesh Kumar Singh 10 , Pradeep Sharma 11 , Pradeep Kumar Saha 12 , Chellamuthu Ramasubramanian 13 , Ritambhara Yeshwant Mehta 14 , Theerthankara Meethal Shibukumar 15
|
Background
India accounts for 18% of the global population and 26·6% of global suicide deaths. However, robust population-based, nationally representative data on suicidality are not readily available to plan and implement suicide prevention programmes in India. We aimed to investigate the prevalence and sociodemographic differentials of suicidality using data from the National Mental Health Survey (NMHS) of India, 2015–16.
Methods
Trained field data collectors from the NMHS obtained information on suicidality (during the past month) from a community sample of adults aged 18 years and older using the suicidality module of the Mini-International Neuropsychiatric Interview (version 6.0). Suicidality was categorised as low, moderate, high, and overall (representing any suicidality), and examined for sociodemographic differentials using normalised sampling weights. For each of the 12 surveyed states, we calculated the age-standardised suicidality prevalence for men and women, men-to-women ratio of weighted suicidality prevalence, ratio of suicidality to suicide deaths, and ratio of suicide attempts to suicide deaths. We used logistic regression analysis to examine the association between sociodemographic factors and overall suicidality and severity.
Findings
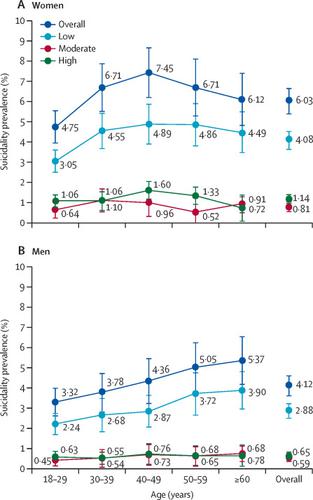
Among 34 748 participants with complete interviews, 5·1% (95% CI 4·7–5·6) had some level of suicidality, and 0·3% (0·2–0·4) had at least one suicide attempt in the past month. The prevalence of overall suicidality was higher in women (6·0% [5·4–6·6]) than in men (4·1% [3·7–4·6]). The prevalence of overall suicidality was highest in those aged 40–49 years among women and in those aged 60 years or older among men. Compared with their counterparts, individuals with lower educational attainment, individuals residing in urban metropolitan cities, individuals who were widowed, separated, or divorced, and unemployed individuals had a higher prevalence of overall suicidality. The men-to-women ratio of overall suicidality prevalence for India was 0·68 (range 0·55–0·85). For every death by suicide in India, there were more than 200 people with suicidality and more than 15 suicide attempts. We found variations for various severities of suicidality. We found an increased risk for overall suicidality in women versus men (odds ratio [OR] 1·54 [95% CI 1·31–1·81]; p<0·0001) and in individuals residing in urban metropolitan cities versus those residing in rural areas (1·75 [1·30–2·35]; p=0·0002). Individuals belonging to the lowest income quintile (reference group with OR <1·00 and p<0·05 for other income quintiles), those with depressive disorders (28·78 [20·04–41·33]; p<0.0001) and those with alcohol use disorders (6·52 [3·83–11·10]; p<0.0001) had an increased risk for high suicidality, compared with their corresponding counterparts.
Interpretation
A national suicide prevention strategy that is comprehensive, using multisectoral approaches, is required to address the prevailing sociodemographic and other risk factors for reducing suicidality and suicide deaths in India. This study also has implications for other low-income and middle-income countries in south Asia, where sociodemographic factors play a crucial role for suicide prevention.
Funding
Ministry of Health and Family Welfare, Government of India.
中文翻译:

基于自杀性及其相关性的基于人口的分析:2015-16年印度国家心理健康调查的结果。
背景
印度占全球人口的18%,占全球自杀死亡人数的26·6%。但是,在印度尚无法获得关于自杀的强有力的以人口为基础的,具有国家代表性的数据,以计划和实施自杀预防计划。我们旨在使用2015–16年印度国家心理健康调查(NMHS)的数据调查自杀性的患病率和社会人口统计学差异。
方法
来自NMHS的经过培训的现场数据收集者使用迷你国际神经精神病学访谈(版本6.0)的自杀模块从18岁及以上成年人的社区样本中获得了自杀的信息(过去一个月)。自杀性分为低,中,高和总体(代表任何自杀性),并使用归一化的抽样权重检查了社会人口统计学差异。对于12个接受调查的州中的每个州,我们计算了男女的标准化年龄自杀率,加权自杀率的男女比例,自杀率与自杀死亡率的比值以及自杀企图与自杀死亡率的比值。我们使用逻辑回归分析检查了社会人口统计学因素与总体自杀和严重程度之间的关联。
发现
在34 748名接受了完整访谈的参与者中,5·1%(95%CI 4·7-5·6)有一定程度的自杀倾向,0·3%(0·2-0·4)至少有一次自杀企图。在过去的一个月中。女性(6·0%[5·4-6·6])的总体自杀倾向高于男性(4·1%[3·7-4·6])。在40-49岁的女性中,男性自杀率最高,在60岁或60岁以上的男性中,自杀率最高。与同龄人相比,受教育程度较低的人,居住在大城市的人,丧偶,分居或离婚的人以及失业的人的总体自杀率较高。印度总体自杀率的男女比为0·68(范围为0·55-0.85)。印度每因自杀死亡,自杀人数超过200人,自杀企图超过15次。我们发现了各种严重程度的自杀倾向。我们发现女性与男性的整体自杀倾向风险增加(比值比[OR] 1·54 [95%CI 1·31-1-1·81]; p <0·0001)以及居住在城市大都市中的个体与男性相比居住在农村地区(1·75 [1·30-2·35]; p = 0·0002)。属于最低收入五分位数的人(参考组,OR <1·00,其他收入五分位数的人为p <0·05),患有抑郁症的人(28·78 [20·04-41·33]; p <0.0001)与那些有酒精使用障碍的人(6·52 [3·83-11·10]; p <0.0001)相比,相应的人有更高的自杀倾向。我们发现女性与男性的整体自杀倾向风险增加(比值比[OR] 1·54 [95%CI 1·31-1-1·81]; p <0·0001)以及居住在城市大都市中的个体与男性相比居住在农村地区(1·75 [1·30-2·35]; p = 0·0002)。属于最低收入五分位数的人(参考组,OR <1·00,其他收入五分位数的人为p <0·05),患有抑郁症的人(28·78 [20·04-41·33]; p <0.0001)与那些有酒精使用障碍的人(6·52 [3·83-11·10]; p <0.0001)相比,相应的人有更高的自杀倾向。我们发现,女性与男性的整体自杀倾向风险增加(比值比[OR] 1·54 [95%CI 1·31-1-1·81]; p <0·0001)以及居住在城市大都市中的个体与男性相比居住在农村地区(1·75 [1·30-2·35]; p = 0·0002)。属于最低收入五分位数的人(参考组,OR <1·00,其他收入五分位数的人为p <0·05),患有抑郁症的人(28·78 [20·04-41·33]; p <0.0001)与那些有酒精使用障碍的人(6·52 [3·83-11·10]; p <0.0001)相比,相应的人有更高的自杀倾向。
解释
需要采用多部门方法的,全面的国家自杀预防策略,以解决当前印度减少人口自杀和自杀死亡的社会人口统计学及其他风险因素。这项研究对南亚的其他低收入和中等收入国家也有影响,在这些国家中,社会人口因素在预防自杀中起着至关重要的作用。
资金
印度政府卫生和家庭福利部。



























 京公网安备 11010802027423号
京公网安备 11010802027423号