JACC: Cardiovascular Interventions ( IF 11.3 ) Pub Date : 2019-12-02 , DOI: 10.1016/j.jcin.2019.08.039 Jurrien M Ten Berg 1 , Anne de Veer 1 , Jonas Oldgren 2 , Philippe Gabriel Steg 3 , Dmitry A Zateyshchikov 4 , Petr Jansky 5 , Ki-Bae Seung 6 , Stefan H Hohnloser 7 , Gregory Y H Lip 8 , Matias Nordaby 9 , Eva Kleine 9 , Deepak L Bhatt 10 , Christopher P Cannon 10 ,
|
Objectives
The aim of this study was to assess if prior oral anticoagulant agent (OAC) use modifies the lower bleeding risk observed with dabigatran dual therapy (dabigatran twice daily plus a P2Y12 inhibitor) versus warfarin triple therapy (warfarin plus a P2Y12 inhibitor plus aspirin) in patients with atrial fibrillation who underwent percutaneous coronary intervention (PCI).
Background
In the RE-DUAL PCI (Randomized Evaluation of Dual Antithrombotic Therapy With Dabigatran Versus Triple Therapy With Warfarin in Patients With Nonvalvular Atrial Fibrillation Undergoing Percutaneous Coronary Intervention) trial, the primary outcome of major bleeding or clinically relevant nonmajor bleeding was lower with dabigatran dual therapy versus warfarin triple therapy in patients with atrial fibrillation who underwent PCI.
Methods
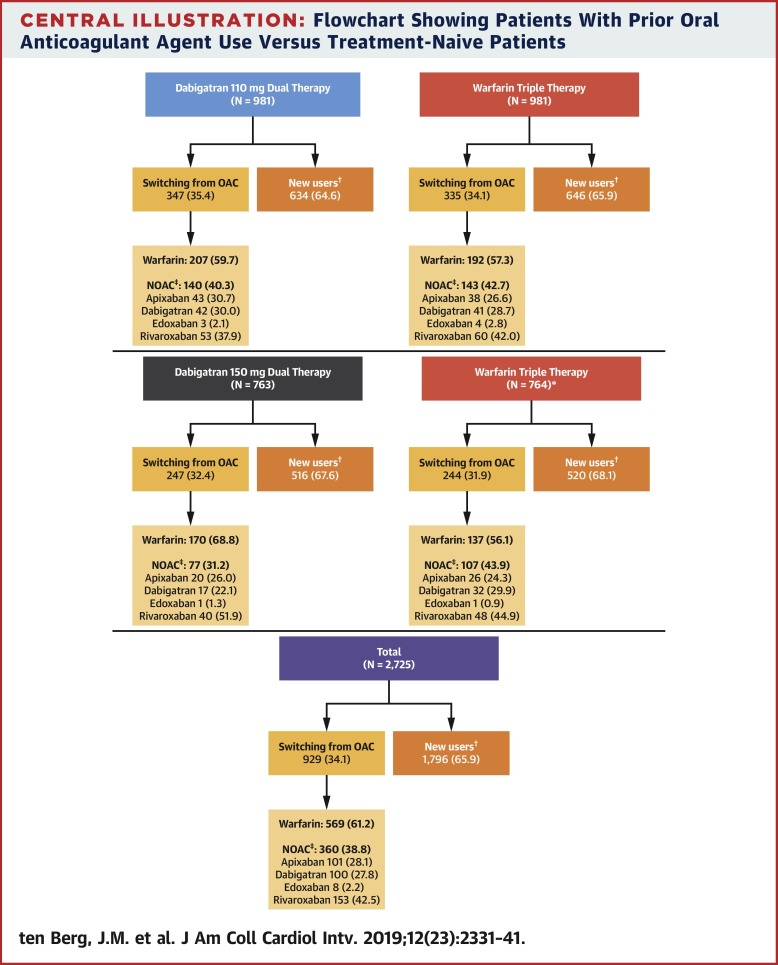
A total of 2,725 patients were randomized to dual therapy with dabigatran (110 or 150 mg twice daily) plus clopidogrel or ticagrelor or triple therapy with warfarin plus aspirin and clopidogrel or ticagrelor. Subgroup analysis compared risk for major bleeding or clinically relevant nonmajor bleeding and a composite thromboembolic endpoint in patients with prior OAC use and in those who were OAC treatment naive.
Results
Risk for major bleeding or clinically relevant nonmajor bleeding was reduced with both dabigatran dual therapies compared with warfarin triple therapy in both the prior OAC use group (hazard ratios: 0.58 [95% confidence interval (CI): 0.42 to 0.81] and 0.61 [95% CI: 0.41 to 0.92] with 110 and 150 mg dabigatran, respectively) and the OAC-naive group (hazard ratios: 0.49 [95% CI: 0.38 to 0.63] and 0.76 [95% CI: 0.59 to 0.97] with 110 and 150 mg dabigatran) (p for interaction = 0.42 and 0.37, 110 and 150 mg dabigatran, respectively). The risk for thromboembolic events seemed similar with dabigatran dual therapy (both doses) and warfarin triple therapy across subgroups.
Conclusions
Bleeding risk was reduced with dabigatran dual therapy versus warfarin triple therapy in patients with atrial fibrillation after PCI, regardless of whether they were prior OAC users or OAC treatment naive. These results suggest that it is also safe to switch patients on OAC pre-PCI to dabigatran dual therapy post-PCI.
中文翻译:

房颤患者PCI后口服抗凝治疗的切换:RE-DUAL PCI试验亚分析。
目标
这项研究的目的是评估与口服华法林三联疗法(华法林加P2Y 12抑制剂加阿司匹林)相比,先前使用口服抗凝剂(OAC)是否可以改善达比加群双重疗法(达比加群每天两次,加P2Y 12抑制剂)观察到的较低出血风险。经皮冠状动脉介入治疗(PCI)的房颤患者。
背景
在RE-DUAL PCI(达比加群酯双重抗凝治疗与华法林三联疗法对非瓣膜性房颤患者行经皮冠状动脉介入治疗的随机评估)试验中,达比加群酯双重治疗对主要出血或临床相关的非主要出血的主要结局较低与华法林三联疗法对接受PCI的房颤患者的疗效比较。
方法
总计2,725例患者被随机分配到接受达比加群(110或150 mg每天两次)加氯吡格雷或替卡格雷的双重治疗或华法林加阿司匹林和氯吡格雷或替卡格雷的三联治疗。亚组分析比较了先前使用过OAC的患者和未接受过OAC治疗的患者发生大出血或临床相关的非大出血风险以及复合血栓栓塞终点的风险。
结果
在既往的OAC使用组中,达比加群双重疗法与华法林三次疗法相比,两种达比加群双重疗法均降低了重大出血或临床相关非重大出血的风险(危险比:0.58 [95%置信区间(CI):0.42至0.81]和0.61 [95]分别含110和150 mg达比加群的CI百分比:0.41至0.92)和未使用OAC的组(危险比:分别为110和110的0.49 [95%CI:0.38至0.63]和0.76 [95%CI:0.59至0.97]。 150 mg达比加群)(相互作用的p分别为0.42和0.37、110和150 mg达比加群)。达比加群双重疗法(两种剂量)和华法林三次疗法在各亚组中发生血栓栓塞事件的风险似乎相似。
结论
与PCI术后房颤患者相比,达比加群双重疗法与华法林三次疗法相比出血风险降低,无论他们以前是OAC使用者还是单纯使用OAC的患者。这些结果表明,将PCI前的OAC患者转为PCI后的达比加群双重治疗也是安全的。



























 京公网安备 11010802027423号
京公网安备 11010802027423号