Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Supervised injection facility use and all-cause mortality among people who inject drugs in Vancouver, Canada: A cohort study.
PLOS Medicine ( IF 15.8 ) Pub Date : 2019-11-26 , DOI: 10.1371/journal.pmed.1002964 Mary Clare Kennedy 1, 2 , Kanna Hayashi 1, 3 , M-J Milloy 1, 2 , Evan Wood 1, 2 , Thomas Kerr 1, 2
PLOS Medicine ( IF 15.8 ) Pub Date : 2019-11-26 , DOI: 10.1371/journal.pmed.1002964 Mary Clare Kennedy 1, 2 , Kanna Hayashi 1, 3 , M-J Milloy 1, 2 , Evan Wood 1, 2 , Thomas Kerr 1, 2
Affiliation
|
BACKGROUND
People who inject drugs (PWID) experience elevated rates of premature mortality. Although previous studies have demonstrated the role of supervised injection facilities (SIFs) in reducing various harms associated with injection drug use, including accidental overdose death, the possible impact of SIF use on all-cause mortality is unknown. Therefore, we examined the relationship between frequent SIF use and all-cause mortality among PWID in Vancouver, Canada.
METHODS AND FINDINGS
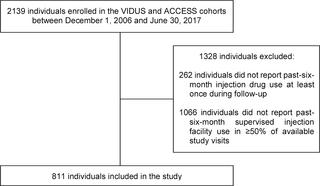
Data were derived from 2 prospective cohort studies of PWID in Vancouver, Canada, between December 2006 and June 2017. Every 6 months, participants completed questionnaires that elicited information regarding sociodemographic characteristics, substance use patterns, social-structural exposures, and use of health services including SIFs. These data were confidentially linked to the provincial vital statistics database to ascertain mortality rates and causes of death. We used multivariable extended Cox regression analyses to estimate the independent association between frequent (i.e., at least weekly) SIF use and all-cause mortality. Of 811 participants, 278 (34.3%) were women, and the median age was 39 years (IQR 33-46) at baseline. In total, 432 (53.3%) participants reported frequent SIF use at baseline, and 379 (46.7%) did not. At baseline, frequent SIF users were on average younger than nonfrequent users, and a higher proportion of frequent SIF users than nonfrequent users were unstably housed, resided in the Downtown Eastside neighbourhood, injected in public, had a recent non-fatal overdose, used prescription opioids at least daily, injected heroin at least daily, injected cocaine at least daily, and injected crystal methamphetamine at least daily. A lower proportion of frequent SIF users than nonfrequent users were HIV positive and enrolled in addiction treatment at baseline. The median duration of follow-up among study participants was 72 months (IQR 24-123). In total, 112 participants (13.8%) died during the study period, yielding a crude mortality rate of 22.7 (95% CI 18.7-27.4) deaths per 1,000 person-years. The median years of potential life lost per death was 34 (IQR 27-42) years. In a time-updated multivariable model, frequent SIF use was inversely associated with risk of all-cause mortality after adjusting for potential confounders, including age, sex, HIV seropositivity, unstable housing, at least daily cocaine injection, public injection, incarceration, enrolment in addiction treatment, and calendar year of interview (adjusted hazard ratio 0.46, 95% CI 0.26-0.80, p = 0.006). The main study limitations are the limited generalizability of findings due to non-random sampling, the potential for reporting biases due to reliance on some self-reported information, and the possibility that residual confounding influenced findings.
CONCLUSIONS
We observed a high burden of premature mortality among a community-recruited cohort of PWID. Frequent SIF use was associated with a lower risk of death, independent of relevant confounders. These findings support efforts to enhance access to SIFs as a strategy to reduce mortality among PWID. Further analyses of individual-level data are needed to determine estimates of, and potential causal pathways underlying, associations between SIF use and specific causes of death.
中文翻译:

在加拿大温哥华进行的有监督注射设施的使用和所有注射毒品的人的全因死亡率:一项队列研究。
背景技术注射药物(PWID)的人过早死亡的发生率升高。尽管以前的研究已经证明了有监督注射设施(SIF)在减少与注射毒品使用相关的各种伤害(包括意外的过量死亡)中的作用,但使用SIF对全因死亡率的可能影响尚不清楚。因此,我们研究了加拿大温哥华PWID中频繁使用SIF与全因死亡率之间的关系。方法和结果数据来自2006年12月至2017年6月在加拿大温哥华进行的2项PWID前瞻性队列研究。参与者每6个月完成一次问卷调查,以获取有关社会人口统计学特征,物质使用模式,社会结构暴露和使用情况的信息。包括SIF在内的医疗服务。这些数据被秘密地链接到省生命统计数据库,以确定死亡率和死亡原因。我们使用多变量扩展Cox回归分析来估计频繁(即至少每周一次)使用SIF与全因死亡率之间的独立关联。在811名参与者中,有278名(34.3%)是女性,基线时的中位年龄为39岁(IQR 33-46)。共有432名(53.3%)参与者报告了在基线时频繁使用SIF,而没有379名(46.7%)。基线时,SIF频繁使用者的平均年龄要比非频繁使用者年轻,并且居住在市区东区居民区的不稳定SIF使用者比例比不经常使用的使用者更高,这些人最近公开接受非致命性过量使用处方至少每天一次阿片类药物,至少每天一次注射海洛因,至少每天注射一次可卡因,每天至少注射一次甲基苯丙胺晶体。经常感染SIF的使用者中,艾滋病毒呈阳性且参加基线成瘾治疗的比例要低于不经常使用的使用者。研究参与者的中位随访时间为72个月(IQR 24-123)。在研究期间,总共有112名参与者(13.8%)死亡,每千人年死亡的总死亡率为22.7(95%CI 18.7-27.4)。每次死亡所导致的潜在生命损失的中位数年限是34(IQR 27-42)年。在时间更新的多变量模型中,在校正了可能的混杂因素(包括年龄,性别,HIV血清反应阳性,不稳定的住房,至少每天可卡因注射,公共注射,监禁,入学)后,频繁使用SIF与全因死亡率风险成反比在成瘾治疗中 和访谈的日历年(调整后的危险比为0.46,95%CI为0.26-0.80,p = 0.006)。主要的研究局限性是由于非随机抽样而导致的研究结果的局限性,由于依赖某些自我报告的信息而可能导致报告偏倚的可能性以及残留的混杂因素影响研究结果的可能性。结论我们观察到社区招募的PWID人群中过早死亡的负担很高。独立于相关混杂因素,频繁使用SIF与较低的死亡风险相关。这些发现支持了增加获取SIF的努力,以此作为降低PWID死亡率的策略。需要对个人数据进行进一步分析,以确定SIF使用与特定死亡原因之间的关联以及潜在的因果关系估计。
更新日期:2019-12-03
中文翻译:

在加拿大温哥华进行的有监督注射设施的使用和所有注射毒品的人的全因死亡率:一项队列研究。
背景技术注射药物(PWID)的人过早死亡的发生率升高。尽管以前的研究已经证明了有监督注射设施(SIF)在减少与注射毒品使用相关的各种伤害(包括意外的过量死亡)中的作用,但使用SIF对全因死亡率的可能影响尚不清楚。因此,我们研究了加拿大温哥华PWID中频繁使用SIF与全因死亡率之间的关系。方法和结果数据来自2006年12月至2017年6月在加拿大温哥华进行的2项PWID前瞻性队列研究。参与者每6个月完成一次问卷调查,以获取有关社会人口统计学特征,物质使用模式,社会结构暴露和使用情况的信息。包括SIF在内的医疗服务。这些数据被秘密地链接到省生命统计数据库,以确定死亡率和死亡原因。我们使用多变量扩展Cox回归分析来估计频繁(即至少每周一次)使用SIF与全因死亡率之间的独立关联。在811名参与者中,有278名(34.3%)是女性,基线时的中位年龄为39岁(IQR 33-46)。共有432名(53.3%)参与者报告了在基线时频繁使用SIF,而没有379名(46.7%)。基线时,SIF频繁使用者的平均年龄要比非频繁使用者年轻,并且居住在市区东区居民区的不稳定SIF使用者比例比不经常使用的使用者更高,这些人最近公开接受非致命性过量使用处方至少每天一次阿片类药物,至少每天一次注射海洛因,至少每天注射一次可卡因,每天至少注射一次甲基苯丙胺晶体。经常感染SIF的使用者中,艾滋病毒呈阳性且参加基线成瘾治疗的比例要低于不经常使用的使用者。研究参与者的中位随访时间为72个月(IQR 24-123)。在研究期间,总共有112名参与者(13.8%)死亡,每千人年死亡的总死亡率为22.7(95%CI 18.7-27.4)。每次死亡所导致的潜在生命损失的中位数年限是34(IQR 27-42)年。在时间更新的多变量模型中,在校正了可能的混杂因素(包括年龄,性别,HIV血清反应阳性,不稳定的住房,至少每天可卡因注射,公共注射,监禁,入学)后,频繁使用SIF与全因死亡率风险成反比在成瘾治疗中 和访谈的日历年(调整后的危险比为0.46,95%CI为0.26-0.80,p = 0.006)。主要的研究局限性是由于非随机抽样而导致的研究结果的局限性,由于依赖某些自我报告的信息而可能导致报告偏倚的可能性以及残留的混杂因素影响研究结果的可能性。结论我们观察到社区招募的PWID人群中过早死亡的负担很高。独立于相关混杂因素,频繁使用SIF与较低的死亡风险相关。这些发现支持了增加获取SIF的努力,以此作为降低PWID死亡率的策略。需要对个人数据进行进一步分析,以确定SIF使用与特定死亡原因之间的关联以及潜在的因果关系估计。



























 京公网安备 11010802027423号
京公网安备 11010802027423号