当前位置:
X-MOL 学术
›
JACC Cardiovasc. Inte.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Outcomes Following Percutaneous Coronary Intervention in Saphenous Vein Grafts With and Without Embolic Protection Devices.
JACC: Cardiovascular Interventions ( IF 11.3 ) Pub Date : 2019-11-18 , DOI: 10.1016/j.jcin.2019.08.037 Ahmad Shoaib 1 , Tim Kinnaird 2 , Nick Curzen 3 , Peter Ludman 4 , David Smith 5 , Chee W Khoo 6 , Evangelos Kontopantelis 7 , Muhammad Rashid 1 , Mohamed Mohamed 1 , James Nolan 1 , Azfar Zaman 8 , Mamas A Mamas 1 , ,
JACC: Cardiovascular Interventions ( IF 11.3 ) Pub Date : 2019-11-18 , DOI: 10.1016/j.jcin.2019.08.037 Ahmad Shoaib 1 , Tim Kinnaird 2 , Nick Curzen 3 , Peter Ludman 4 , David Smith 5 , Chee W Khoo 6 , Evangelos Kontopantelis 7 , Muhammad Rashid 1 , Mohamed Mohamed 1 , James Nolan 1 , Azfar Zaman 8 , Mamas A Mamas 1 , ,
Affiliation
|
OBJECTIVES
The aim of this study was to describe the early (inpatient and 30-day) and late (1-year) outcomes of percutaneous coronary intervention (PCI) in saphenous vein grafts (SVGs), with and without the use of embolic protection devices (EPD), in a large, contemporary, unselected national cohort from the database of the British Cardiovascular Intervention Society.
BACKGROUND
There are limited, and discrepant, data on the clinical benefits of the adjunctive use of EPDs during PCI to SVGs in the contemporary era.
METHODS
A longitudinal cohort of patients (2007 to 2014, n = 20,642) who underwent PCI to SVGs in the British Cardiovascular Intervention Society database was formed. Clinical, demographic, procedural, and outcome data were analyzed by dividing into 2 groups: no EPD (PCI to SVGs without EPDs, n = 17,730) and EPD (PCI to SVGs with EPDs, n = 2,912).
RESULTS
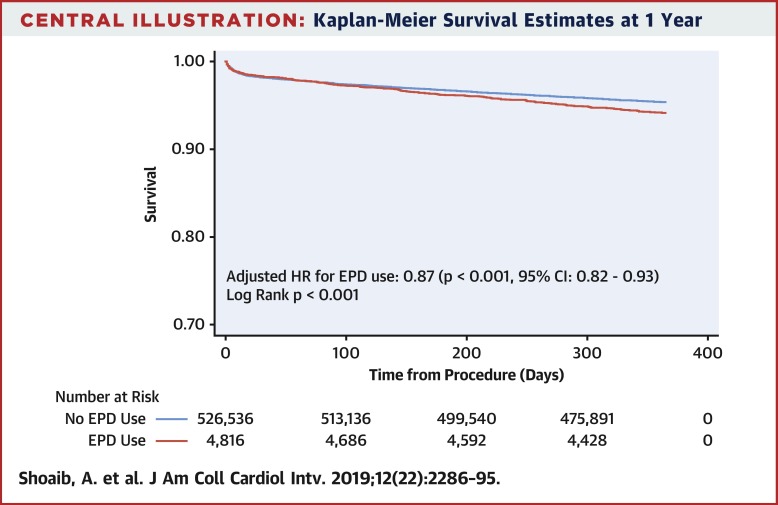
Patients in the EPD group were older, had more comorbidities, and had a higher prevalence of moderate to severe left ventricular systolic dysfunction. Mortality was lower in the EPD group during hospital admission (0.70% vs. 1.29%; p = 0.008) and at 30 days (1.44% vs. 2.01%; p = 0.04) but similar at 1 year (6.22% vs. 6.01%; p = 0.67). Following multivariate analyses, no significant difference in mortality was observed during index admission (odds ratio [OR]: 0.71; 95% confidence interval [CI]: 0.42 to 1.19; p = 0.19), at 30 days (OR: 0.87; 95% CI: 0.60 to 1.25; p = 0.45), and at 1 year (OR: 0.92; 95% CI: 0.77 to 1.11; p = 0.41), along with similar rates of in-hospital major adverse cardiovascular events (OR: 1.16; 95% CI: 0.83 to 1.62; p = 0.39) and stroke (OR: 0.68; 95% CI: 0.20 to 2.35; p = 0.54). In propensity score-matched analyses, lower inpatient mortality was observed in the EPD group (OR: 0.46; 95% CI: 0.13 to 0.80; p = 0.002), although the adjusted risk for the periprocedural no-reflow or slow-flow phenomenon was higher in patients in whom EPDs were used (OR: 2.16; 95% CI: 1.71 to 2.73; p < 0.001).
CONCLUSIONS
In this contemporary cohort, EPDs were used more commonly in higher risk patients but were associated with similar clinical outcomes in multivariate analyses. Lower inpatient mortality was observed in the EPD group in univariate and propensity score-matched analyses.
中文翻译:

在有或没有栓塞保护装置的大隐静脉移植物中经皮冠状动脉介入治疗后的结果。
目的本研究的目的是描述在使用和不使用栓塞保护装置的情况下,大隐静脉移植物(SVG)的经皮冠状动脉介入治疗(PCI)的早期(住院和30天)和晚期(1年)结局。 (EPD),来自英国心血管介入学会数据库中的一个大型,未选择的当代国家队列。背景技术在当代时代,在PCI到SVG期间辅助使用EPD的临床益处的数据有限且相互矛盾。方法在英国心血管介入学会数据库中,对接受PCI至SVGs治疗的患者(2007年至2014年,n = 20,642)进行纵向队列研究。将临床,人口统计学,程序和结果数据分为两组:无EPD(无EPD的PCI至SVG,n = 17,730)和EPD(有EPD的PCI至SVG,n = 2,912)。结果EPD组的患者年龄较大,合并症更多,中度至重度左心室收缩功能障碍的患病率更高。EPD组住院期间的死亡率较低(0.70%vs. 1.29%; p = 0.008)和30天时(1.44%vs. 2.01%; p = 0.04),但在1年时死亡率相似(6.22%vs. 6.01%) ; p = 0.67)。经过多变量分析,在第30天时,进入指数期间的死亡率无显着差异(优势比[OR]:0.71; 95%置信区间[CI]:0.42至1.19; p = 0.19)(OR:0.87; 95%) CI:0.60至1.25; p = 0.45)和1年时(OR:0.92; 95%CI:0.77至1.11; p = 0.41),以及院内主要不良心血管事件发生率相似(OR:1.16; 95%CI:0.83至1.62; p = 0.39)和中风(OR:0.68; 95%CI:0.20至2.35; p = 0.54)。在倾向评分匹配的分析中,尽管调整后的围手术期无再流或慢流现象的风险是,EPD组的住院死亡率较低(OR:0.46; 95%CI:0.13至0.80; p = 0.002)。在使用EPD的患者中更高(OR:2.16; 95%CI:1.71至2.73; p <0.001)。结论在这一当代人群中,EPD在较高风险的患者中更常见,但在多变量分析中与相似的临床结局相关。在单因素和倾向得分匹配的分析中,EPD组的住院死亡率较低。1.71至2.73;p <0.001)。结论在这一当代人群中,EPD在较高风险的患者中更常见,但在多变量分析中与相似的临床结局相关。在单因素和倾向得分匹配的分析中,EPD组的住院死亡率较低。1.71至2.73;p <0.001)。结论在这一当代人群中,EPD在较高风险的患者中更常见,但在多变量分析中与相似的临床结局相关。在单因素和倾向得分匹配的分析中,EPD组的住院死亡率较低。
更新日期:2019-11-18
中文翻译:

在有或没有栓塞保护装置的大隐静脉移植物中经皮冠状动脉介入治疗后的结果。
目的本研究的目的是描述在使用和不使用栓塞保护装置的情况下,大隐静脉移植物(SVG)的经皮冠状动脉介入治疗(PCI)的早期(住院和30天)和晚期(1年)结局。 (EPD),来自英国心血管介入学会数据库中的一个大型,未选择的当代国家队列。背景技术在当代时代,在PCI到SVG期间辅助使用EPD的临床益处的数据有限且相互矛盾。方法在英国心血管介入学会数据库中,对接受PCI至SVGs治疗的患者(2007年至2014年,n = 20,642)进行纵向队列研究。将临床,人口统计学,程序和结果数据分为两组:无EPD(无EPD的PCI至SVG,n = 17,730)和EPD(有EPD的PCI至SVG,n = 2,912)。结果EPD组的患者年龄较大,合并症更多,中度至重度左心室收缩功能障碍的患病率更高。EPD组住院期间的死亡率较低(0.70%vs. 1.29%; p = 0.008)和30天时(1.44%vs. 2.01%; p = 0.04),但在1年时死亡率相似(6.22%vs. 6.01%) ; p = 0.67)。经过多变量分析,在第30天时,进入指数期间的死亡率无显着差异(优势比[OR]:0.71; 95%置信区间[CI]:0.42至1.19; p = 0.19)(OR:0.87; 95%) CI:0.60至1.25; p = 0.45)和1年时(OR:0.92; 95%CI:0.77至1.11; p = 0.41),以及院内主要不良心血管事件发生率相似(OR:1.16; 95%CI:0.83至1.62; p = 0.39)和中风(OR:0.68; 95%CI:0.20至2.35; p = 0.54)。在倾向评分匹配的分析中,尽管调整后的围手术期无再流或慢流现象的风险是,EPD组的住院死亡率较低(OR:0.46; 95%CI:0.13至0.80; p = 0.002)。在使用EPD的患者中更高(OR:2.16; 95%CI:1.71至2.73; p <0.001)。结论在这一当代人群中,EPD在较高风险的患者中更常见,但在多变量分析中与相似的临床结局相关。在单因素和倾向得分匹配的分析中,EPD组的住院死亡率较低。1.71至2.73;p <0.001)。结论在这一当代人群中,EPD在较高风险的患者中更常见,但在多变量分析中与相似的临床结局相关。在单因素和倾向得分匹配的分析中,EPD组的住院死亡率较低。1.71至2.73;p <0.001)。结论在这一当代人群中,EPD在较高风险的患者中更常见,但在多变量分析中与相似的临床结局相关。在单因素和倾向得分匹配的分析中,EPD组的住院死亡率较低。



























 京公网安备 11010802027423号
京公网安备 11010802027423号