当前位置:
X-MOL 学术
›
Nat. Rev. Nephrol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Reappraising the spectrum of AKI and hepatorenal syndrome in patients with cirrhosis.
Nature Reviews Nephrology ( IF 41.5 ) Pub Date : 2019-11-13 , DOI: 10.1038/s41581-019-0218-4 Juan Carlos Q Velez 1, 2 , George Therapondos 3 , Luis A Juncos 4, 5
Nature Reviews Nephrology ( IF 41.5 ) Pub Date : 2019-11-13 , DOI: 10.1038/s41581-019-0218-4 Juan Carlos Q Velez 1, 2 , George Therapondos 3 , Luis A Juncos 4, 5
Affiliation
|
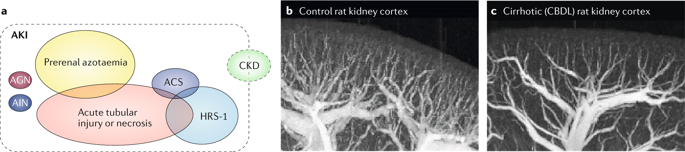
The occurrence of acute kidney injury (AKI) in patients with end-stage liver disease constitutes one of the most challenging clinical scenarios in in-hospital and critical care medicine. Hepatorenal syndrome type 1 (HRS-1), which is a specific type of AKI that occurs in the context of advanced cirrhosis and portal hypertension, is associated with particularly high mortality. The pathogenesis of HRS-1 is largely viewed as a functional derangement that ultimately affects renal vasculature tone. However, new insights suggest that non-haemodynamic tubulo-toxic factors, such as endotoxins and bile acids, might mediate parenchymal renal injury in patients with cirrhosis, suggesting that concurrent mechanisms, including those traditionally associated with HRS-1 and non-traditional factors, might contribute to the development of AKI in patients with cirrhosis. Moreover, histological evidence of morphological abnormalities in the kidneys of patients with cirrhosis and renal dysfunction has prompted the functional nature of HRS-1 to be re-examined. From a clinical perspective, a diagnosis of HRS-1 guides utilization of vasoconstrictive therapy and decisions regarding renal replacement therapy. Patients with cirrhosis are at risk of AKI owing to a wide range of factors. However, the tools currently available to ascertain the diagnosis of HRS-1 and guide therapy are suboptimal. Short of liver transplantation, goal-directed haemodynamically targeted pharmacotherapy remains the cornerstone of treatment for this condition; improved understanding of the underlying pathogenic mechanisms might lead to better clinical outcomes. Here, we examine our current understanding of the pathophysiology of HRS-1 and existing challenges in its diagnosis and treatment.
中文翻译:

重新评估肝硬化患者 AKI 和肝肾综合征的谱系。
终末期肝病患者发生急性肾损伤 (AKI) 是住院和重症监护医学中最具挑战性的临床情况之一。1 型肝肾综合征 (HRS-1) 是一种特定类型的 AKI,发生在晚期肝硬化和门静脉高压症的背景下,与极高的死亡率相关。HRS-1 的发病机制在很大程度上被视为最终影响肾血管张力的功能紊乱。然而,新的见解表明,非血液动力学肾小管毒性因素,如内毒素和胆汁酸,可能介导肝硬化患者的实质肾损伤,这表明并发机制,包括那些传统上与 HRS-1 和非传统因素相关的机制,可能有助于肝硬化患者发生 AKI。此外,肝硬化和肾功能不全患者肾脏形态异常的组织学证据促使重新审视 HRS-1 的功能性质。从临床角度来看,HRS-1 的诊断指导血管收缩疗法的利用和有关肾脏替代疗法的决策。由于多种因素,肝硬化患者有发生 AKI 的风险。然而,目前可用于确定 HRS-1 诊断和指导治疗的工具并不理想。除了肝移植,目标导向的血流动力学靶向药物治疗仍然是这种疾病治疗的基石;更好地了解潜在的致病机制可能会导致更好的临床结果。这里,
更新日期:2019-11-14
中文翻译:

重新评估肝硬化患者 AKI 和肝肾综合征的谱系。
终末期肝病患者发生急性肾损伤 (AKI) 是住院和重症监护医学中最具挑战性的临床情况之一。1 型肝肾综合征 (HRS-1) 是一种特定类型的 AKI,发生在晚期肝硬化和门静脉高压症的背景下,与极高的死亡率相关。HRS-1 的发病机制在很大程度上被视为最终影响肾血管张力的功能紊乱。然而,新的见解表明,非血液动力学肾小管毒性因素,如内毒素和胆汁酸,可能介导肝硬化患者的实质肾损伤,这表明并发机制,包括那些传统上与 HRS-1 和非传统因素相关的机制,可能有助于肝硬化患者发生 AKI。此外,肝硬化和肾功能不全患者肾脏形态异常的组织学证据促使重新审视 HRS-1 的功能性质。从临床角度来看,HRS-1 的诊断指导血管收缩疗法的利用和有关肾脏替代疗法的决策。由于多种因素,肝硬化患者有发生 AKI 的风险。然而,目前可用于确定 HRS-1 诊断和指导治疗的工具并不理想。除了肝移植,目标导向的血流动力学靶向药物治疗仍然是这种疾病治疗的基石;更好地了解潜在的致病机制可能会导致更好的临床结果。这里,



























 京公网安备 11010802027423号
京公网安备 11010802027423号