JAMA Neurology ( IF 29.0 ) Pub Date : 2020-03-01 , DOI: 10.1001/jamaneurol.2019.3854 Yoann Launey 1, 2 , Tim D Fryer 3 , Young T Hong 3 , Luzius A Steiner 1, 4, 5 , Jurgens Nortje 1, 6 , Tonny V Veenith 1, 7 , Peter J Hutchinson 8 , Ari Ercole 1 , Arun K Gupta 1 , Franklin I Aigbirhio 3 , John D Pickard 8 , Jonathan P Coles 1 , David K Menon 1
|
Importance Ischemia is an important pathophysiological mechanism after traumatic brain injury (TBI), but its incidence and spatiotemporal patterns are poorly characterized.
Objective To comprehensively characterize the spatiotemporal changes in cerebral physiology after TBI.
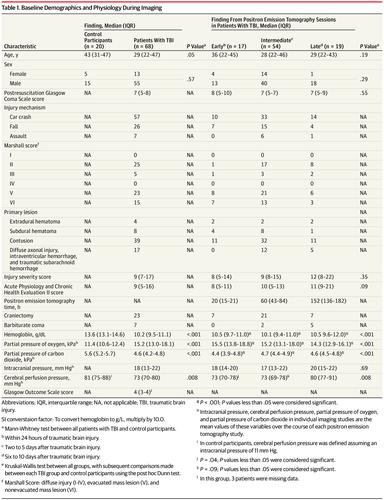
Design, Setting, and Participants This single-center cohort study uses 15oxygen positron emission tomography data obtained in a neurosciences critical care unit from February 1998 through July 2014 and analyzed from April 2018 through August 2019. Patients with TBI requiring intracranial pressure monitoring and control participants were recruited.
Exposures Cerebral blood flow (CBF), cerebral blood volume (CBV), cerebral oxygen metabolism (CMRO2), and oxygen extraction fraction.
Main Outcomes and Measures Ratios (CBF/CMRO2 and CBF/CBV) were calculated. Ischemic brain volume was compared with jugular venous saturation and brain tissue oximetry.
Results A total of 68 patients with TBI and 27 control participants were recruited. Results from 1 patient with TBI and 7 health volunteers were excluded. Sixty-eight patients with TBI (13 female [19%]; median [interquartile range (IQR)] age, 29 [22-47] years) underwent 90 studies at early (day 1 [n = 17]), intermediate (days 2-5 [n = 54]), and late points (days 6-10 [n = 19]) and were compared with 20 control participants (5 female [25%]; median [IQR] age, 43 [31-47] years). The global CBF and CMRO2 findings for patients with TBI were less than the ranges for control participants at all stages (median [IQR]: CBF, 26 [22-30] mL/100 mL/min vs 38 [29-49] mL/100 mL/min; P < .001; CMRO2, 62 [55-71] μmol/100 mL/min vs 131 [101-167] μmol/100 mL/min; P < .001). Early CBF reductions showed a trend of high oxygen extraction fraction (suggesting classical ischemia), but this was inconsistent at later phases. Ischemic brain volume was elevated even in the absence of intracranial hypertension and highest at less than 24 hours after TBI (median [IQR], 36 [10-82] mL), but many patients showed later increases (median [IQR] 6-10 days after TBI, 24 [4-42] mL; across all points: patients, 10 [5-39] mL vs control participants, 1 [0-3] mL; P < 001). Ischemic brain volume was a poor indicator of jugular venous saturation and brain tissue oximetry. Patients’ CBF/CMRO2 ratio was higher than controls (median [IQR], 0.42 [0.35-0.49] vs 0.3 [0.28-0.33]; P < .001) and their CBF/CBV ratio lower (median [IQR], 7.1 [6.4-7.9] vs 12.3 [11.0-14.0]; P < .001), suggesting abnormal flow-metabolism coupling and vascular reactivity. Patients’ CBV was higher than controls (median [IQR], 3.7 [3.4-4.1] mL/100 mL vs 3.0 [2.7-3.6] mL/100 mL; P < .001); although values were lower in patients with intracranial hypertension, these were still greater than controls (median [IQR], 3.7 [3.2-4.0] vs 3.0 [2.7-3.6] mL/100 mL; P = .002), despite more profound reductions in partial pressure of carbon dioxide (median [IQR], 4.3 [4.1-4.6] kPa vs 4.7 [4.3-4.9] kPa; P = .001).
Conclusions and Relevance Ischemia is common early, detectable up to 10 days after TBI, possible without intracranial hypertension, and inconsistently detected by jugular or brain tissue oximetry. There is substantial between-patient and within-patient pathophysiological heterogeneity; ischemia and hyperemia commonly coexist, possibly reflecting abnormalities in flow-metabolism coupling. Increased CBV may contribute to intracranial hypertension but can coexist with abnormal CBF/CBV ratios. These results emphasize the need to consider cerebrovascular pathophysiological complexity when managing patients with TBI.
中文翻译:

颅脑创伤后局部缺血的时空模式和血管功能异常。
重要性 缺血是脑外伤(TBI)后的重要病理生理机制,但其发生率和时空模式尚不明确。
目的 全面探讨TBI后脑部生理变化的时空变化。
设计,设置和参加者 这项单中心队列研究使用了1998年2月至2014年7月在神经科学重症监护室获得的15个氧正电子发射断层扫描数据,并于2018年4月至2019年8月进行了分析。TBI患者需要颅内压监测和控制参与者被招募。
暴露 脑血流量(CBF),脑血容量(CBV),脑氧代谢(CMRO 2)和氧提取分数。
计算了主要结果和测量 比率(CBF / CMRO 2和CBF / CBV)。将缺血性脑容量与颈静脉饱和度和脑组织血氧饱和度进行比较。
结果 共招募了68例TBI患者和27名对照参与者。排除了1名TBI患者和7名健康志愿者的结果。68例TBI患者(13名女性[19%];中位[四分位间距(IQR)]年龄,29 [22-47]岁)在早期(第1天[n = 17])和中级(第7天)接受了90项研究2-5岁[n = 54])和晚点(6-10天[n = 19]天)与20名对照组参与者(5名女性[25%];中位[IQR]年龄为43岁[31-47])进行了比较] 年)。在所有阶段,TBI患者的总体CBF和CMRO 2结果均小于对照参与者的范围(中位数[IQR]:CBF,26 [22-30] mL / 100 mL / min与38 [29-49] mL / 100毫升/分钟; P <0.001; CMRO 2,62 [55-71]微摩尔/ 100毫升/分钟VS 131 [101-167]微摩尔/ 100毫升/分钟;P <.001)。早期CBF降低显示出较高的氧气提取率(建议经典缺血),但在后期则不一致。缺血性脑容量甚至在没有颅内高压的情况下也升高,并且在TBI后不到24小时达到最高(中位数[IQR],36 [10-82] mL),但是许多患者显示出稍后的增加(中位数[IQR] 6-10 TBI后天数为24 [4-42] mL;在所有方面:患者为10 [5-39] mL,而对照组为1 [0-3] mL;P <001)。缺血性脑容量不足以指示颈静脉饱和度和脑组织血氧饱和度。患者的CBF / CMRO 2比值高于对照组(中位[IQR],0.42 [0.35-0.49]和0.3 [0.28-0.33];P <.001)和他们的CBF / CBV比降低(中位数[IQR],7.1 [6.4-7.9]与12.3 [11.0-14.0];P <.001),表明异常的血流-代谢耦合和血管反应性。患者的CBV高于对照组(中位[IQR],分别为3.7 [3.4-4.1] mL / 100 mL和3.0 [2.7-3.6] mL / 100 mL;P <.001);尽管颅内高压患者的血脂水平降低,但仍较对照组大(中位数[IQR],3.7 [3.2-4.0] vs 3.0 [2.7-3.6] mL / 100 mL;P = .002),尽管降低幅度更大二氧化碳的分压(中位数[IQR],4.3 [4.1-4.6] kPa与4.7 [4.3-4.9] kPa;P = .001)。
结论与相关性 缺血是早期常见的疾病,在TBI后最多10天可检测到,可能没有颅内高压,并且通过颈静脉或脑组织血氧饱和度检测也不一致。患者之间和患者内部的病理生理差异很大。缺血和充血通常并存,可能反映了血流-代谢耦合异常。CBV升高可能导致颅内高压,但可以与异常的CBF / CBV比率共存。这些结果强调在处理TBI患者时需要考虑脑血管病理生理的复杂性。



























 京公网安备 11010802027423号
京公网安备 11010802027423号