当前位置:
X-MOL 学术
›
Prostate Cancer Prostatic. Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Prospective study to define the clinical utility and benefit of Decipher testing in men following prostatectomy.
Prostate Cancer and Prostatic Diseases ( IF 4.8 ) Pub Date : 2019-11-12 , DOI: 10.1038/s41391-019-0185-7 Joseph Marascio 1 , Daniel E Spratt 2 , Jingbin Zhang 3 , Edouard J Trabulsi 4 , Tiffany Le 3 , Worlanyo Sosu Sedzorme 3 , Whitney H Beeler 2 , Elai Davicioni 3 , Bashar Dabbas 3 , Daniel W Lin 5 , John L Gore 5 , Matthew Bloom 1 , Mark Mann 4 , J Ryan Mark 4 , Anne Calvaresi 4 , James L Godwin 6 , Peter McCue 7 , Mark D Hurwitz 1 , W Kevin Kelly 6 , Costas D Lallas 4 , Karen E Knudsen 8 , Leonard G Gomella 4 , Adam P Dicker 1 , Robert B Den 1, 4, 8
Prostate Cancer and Prostatic Diseases ( IF 4.8 ) Pub Date : 2019-11-12 , DOI: 10.1038/s41391-019-0185-7 Joseph Marascio 1 , Daniel E Spratt 2 , Jingbin Zhang 3 , Edouard J Trabulsi 4 , Tiffany Le 3 , Worlanyo Sosu Sedzorme 3 , Whitney H Beeler 2 , Elai Davicioni 3 , Bashar Dabbas 3 , Daniel W Lin 5 , John L Gore 5 , Matthew Bloom 1 , Mark Mann 4 , J Ryan Mark 4 , Anne Calvaresi 4 , James L Godwin 6 , Peter McCue 7 , Mark D Hurwitz 1 , W Kevin Kelly 6 , Costas D Lallas 4 , Karen E Knudsen 8 , Leonard G Gomella 4 , Adam P Dicker 1 , Robert B Den 1, 4, 8
Affiliation
|
BACKGROUND
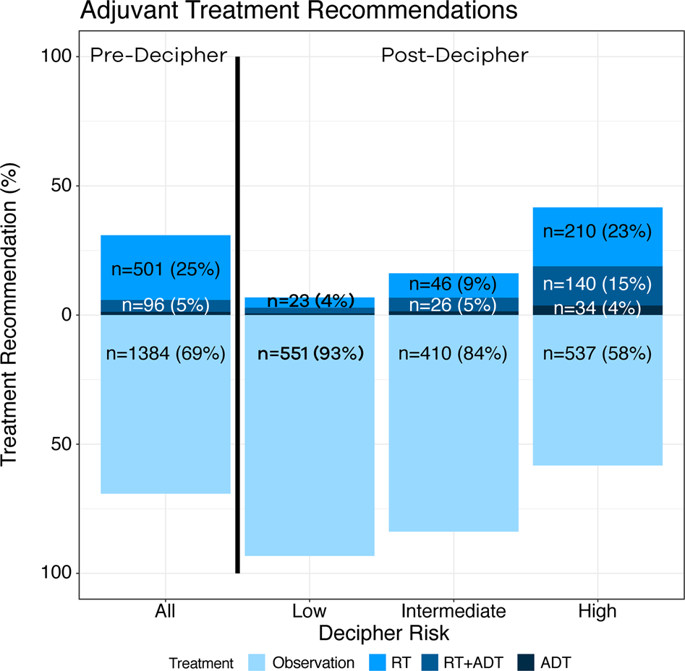
Genomic classifiers (GC) have been shown to improve risk stratification post prostatectomy. However, their clinical benefit has not been prospectively demonstrated. We sought to determine the impact of GC testing on postoperative management in men with prostate cancer post prostatectomy.
METHODS
Two prospective registries of prostate cancer patients treated between 2014 and 2019 were included. All men underwent Decipher tumor testing for adverse features post prostatectomy (Decipher Biosciences, San Diego, CA). The clinical utility cohort, which measured the change in treatment decision-making, captured pre- and postgenomic treatment recommendations from urologists across diverse practice settings (n = 3455). The clinical benefit cohort, which examined the difference in outcome, was from a single academic institution whose tumor board predefined "best practices" based on GC results (n = 135).
RESULTS
In the clinical utility cohort, providers' recommendations pregenomic testing were primarily observation (69%). GC testing changed recommendations for 39% of patients, translating to a number needed to test of 3 to change one treatment decision. In the clinical benefit cohort, 61% of patients had genomic high-risk tumors; those who received the recommended adjuvant radiation therapy (ART) had 2-year PSA recurrence of 3 vs. 25% for those who did not (HR 0.1 [95% CI 0.0-0.6], p = 0.013). For the genomic low/intermediate-risk patients, 93% followed recommendations for observation, with similar 2-year PSA recurrence rates compared with those who received ART (p = 0.93).
CONCLUSIONS
The use of GC substantially altered treatment decision-making, with a number needed to test of only 3. Implementing best practices to routinely recommend ART for genomic-high patients led to larger than expected improvements in early biochemical endpoints, without jeopardizing outcomes for genomic-low/intermediate-risk patients.
中文翻译:

前瞻性研究定义了前列腺切除术后男性的解密检查的临床效用和益处。
背景技术已经证明基因组分类器(GC)可改善前列腺切除术后的危险分层。但是,其临床益处尚未得到前瞻性证明。我们试图确定GC检测对前列腺癌术后前列腺癌男性患者术后管理的影响。方法包括2014年至2019年期间接受治疗的两个前列腺癌患者的前瞻性登记册。所有男性均在前列腺切除术后进行了Decepher肿瘤测试,以了解其不良特征(加利福尼亚州圣地亚哥,Decipher Biosciences)。该临床实用程序队列测量了治疗决策的变化,并从泌尿科医师的不同实践环境中获取了基因组治疗前后的建议(n = 3455)。临床受益队列研究了结局的差异,来自一家学术机构,该机构的肿瘤董事会根据GC结果预定义了“最佳做法”(n = 135)。结果在临床应用队列中,提供者建议的基因组学前测试主要是观察(69%)。GC测试改变了对39%的患者的建议,转化为3个测试以改变一项治疗决策所需的数字。在临床受益人群中,有61%的患者患有基因组高危肿瘤。接受推荐辅助放疗(ART)的患者2年PSA复发为3,而未接受PSA复发的患者为25%(HR 0.1 [95%CI 0.0-0.6],p = 0.013)。对于基因组低/中度风险患者,有93%遵循了观察建议,与接受ART的患者相比,其2年PSA复发率相似(p = 0.93)。
更新日期:2019-11-12
中文翻译:

前瞻性研究定义了前列腺切除术后男性的解密检查的临床效用和益处。
背景技术已经证明基因组分类器(GC)可改善前列腺切除术后的危险分层。但是,其临床益处尚未得到前瞻性证明。我们试图确定GC检测对前列腺癌术后前列腺癌男性患者术后管理的影响。方法包括2014年至2019年期间接受治疗的两个前列腺癌患者的前瞻性登记册。所有男性均在前列腺切除术后进行了Decepher肿瘤测试,以了解其不良特征(加利福尼亚州圣地亚哥,Decipher Biosciences)。该临床实用程序队列测量了治疗决策的变化,并从泌尿科医师的不同实践环境中获取了基因组治疗前后的建议(n = 3455)。临床受益队列研究了结局的差异,来自一家学术机构,该机构的肿瘤董事会根据GC结果预定义了“最佳做法”(n = 135)。结果在临床应用队列中,提供者建议的基因组学前测试主要是观察(69%)。GC测试改变了对39%的患者的建议,转化为3个测试以改变一项治疗决策所需的数字。在临床受益人群中,有61%的患者患有基因组高危肿瘤。接受推荐辅助放疗(ART)的患者2年PSA复发为3,而未接受PSA复发的患者为25%(HR 0.1 [95%CI 0.0-0.6],p = 0.013)。对于基因组低/中度风险患者,有93%遵循了观察建议,与接受ART的患者相比,其2年PSA复发率相似(p = 0.93)。



























 京公网安备 11010802027423号
京公网安备 11010802027423号