当前位置:
X-MOL 学术
›
JACC Heart Fail.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Prescribing Patterns of Heart Failure-Exacerbating Medications Following a Heart Failure Hospitalization.
JACC: Heart Failure ( IF 13.0 ) Pub Date : 2019-11-06 , DOI: 10.1016/j.jchf.2019.08.007 Parag Goyal 1 , Jerard Kneifati-Hayek 2 , Alexi Archambault 3 , Krisha Mehta 4 , Emily B Levitan 5 , Ligong Chen 5 , Ivan Diaz 6 , James Hollenberg 3 , Joseph T Hanlon 7 , Mark S Lachs 8 , Mathew S Maurer 9 , Monika M Safford 3
JACC: Heart Failure ( IF 13.0 ) Pub Date : 2019-11-06 , DOI: 10.1016/j.jchf.2019.08.007 Parag Goyal 1 , Jerard Kneifati-Hayek 2 , Alexi Archambault 3 , Krisha Mehta 4 , Emily B Levitan 5 , Ligong Chen 5 , Ivan Diaz 6 , James Hollenberg 3 , Joseph T Hanlon 7 , Mark S Lachs 8 , Mathew S Maurer 9 , Monika M Safford 3
Affiliation
|
OBJECTIVES
This study sought to describe the patterns of heart failure (HF)-exacerbating medications used among older adults hospitalized for HF and to examine determinants of HF-exacerbating medication use.
BACKGROUND
HF-exacerbating medications can potentially contribute to adverse outcomes and could represent an important target for future strategies to improve post-hospitalization outcomes.
METHODS
Medicare beneficiaries ≥65 years of age with an adjudicated HF hospitalization between 2003 and 2014 were derived from the geographically diverse REGARDS (Reasons for Geographic and Racial Difference in Stroke) cohort study. Major HF-exacerbating medications, defined as those listed on the 2016 American Heart Association Scientific Statement listing medications that can precipitate or induce HF, were examined. Patterns of prescribing medications at hospital admission and at discharge were examined, as well as changes that occurred between admission and discharge; and a multivariable logistic regression analysis was conducted to identify determinants of harmful prescribing practices following HF hospitalization (defined as either the continuation of an HF-exacerbating medications or an increase in the number of HF-exacerbating medications between hospital admission and discharge).
RESULTS
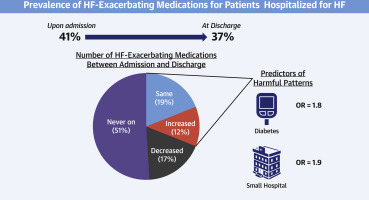
Among 558 unique individuals, 18% experienced a decrease in the number of HF-exacerbating medications between admission and discharge, 19% remained at the same number, and 12% experienced an increase. Multivariable logistic regression analysis revealed that diabetes (odds ratio [OR]: 1.80; 95% confidence interval [CI]: 1.18 to 2.75]) and small hospital size (OR: 1.93; 95% CI: 1.18 to 3.16) were the strongest, independently associated determinants of harmful prescribing practices.
CONCLUSIONS
HF-exacerbating medication regimens are often continued or started following an HF hospitalization. These findings highlight an ongoing need to develop strategies to improve safe prescribing practices in this vulnerable population.
中文翻译:

心力衰竭住院后心力衰竭加重药物的处方模式。
目标 本研究旨在描述因 HF 住院的老年人使用的加重心力衰竭 (HF) 药物的模式,并检查加重 HF 药物使用的决定因素。背景 心衰加重药物可能会导致不良结局,并可能成为未来改善住院后结局策略的重要目标。方法 在 2003 年至 2014 年期间,年龄≥65 岁且经判定 HF 住院的医疗保险受益人来自地理上不同的 REGARDS(卒中的地理和种族差异的原因)队列研究。主要的心力衰竭加重药物,定义为 2016 年美国心脏协会科学声明中列出的可诱发或诱发心力衰竭的药物,已接受检查。检查入院时和出院时的处方药模式,以及入院和出院之间发生的变化;并进行了多变量逻辑回归分析以确定 HF 住院后有害处方做法的决定因素(定义为继续使用 HF 加重药物或在入院和出院之间增加 HF 加重药物的数量)。结果 在 558 名独特的个体中,18% 的人在入院和出院之间经历了 HF 加重药物数量的减少,19% 的人保持相同的数量,12% 的人经历了增加。多变量逻辑回归分析显示糖尿病(比值比 [OR]:1.80;95% 置信区间 [CI]:1.18 至 2.75])和小医院规模(OR:1.93;95% CI:1.18 至 3.16)是有害处方行为的最强、独立相关的决定因素。结论 在 HF 住院后,通常会继续或开始使用会加重 HF 的药物治疗方案。这些发现强调了持续需要制定策略来改善这一弱势群体的安全处方实践。
更新日期:2019-11-07
中文翻译:

心力衰竭住院后心力衰竭加重药物的处方模式。
目标 本研究旨在描述因 HF 住院的老年人使用的加重心力衰竭 (HF) 药物的模式,并检查加重 HF 药物使用的决定因素。背景 心衰加重药物可能会导致不良结局,并可能成为未来改善住院后结局策略的重要目标。方法 在 2003 年至 2014 年期间,年龄≥65 岁且经判定 HF 住院的医疗保险受益人来自地理上不同的 REGARDS(卒中的地理和种族差异的原因)队列研究。主要的心力衰竭加重药物,定义为 2016 年美国心脏协会科学声明中列出的可诱发或诱发心力衰竭的药物,已接受检查。检查入院时和出院时的处方药模式,以及入院和出院之间发生的变化;并进行了多变量逻辑回归分析以确定 HF 住院后有害处方做法的决定因素(定义为继续使用 HF 加重药物或在入院和出院之间增加 HF 加重药物的数量)。结果 在 558 名独特的个体中,18% 的人在入院和出院之间经历了 HF 加重药物数量的减少,19% 的人保持相同的数量,12% 的人经历了增加。多变量逻辑回归分析显示糖尿病(比值比 [OR]:1.80;95% 置信区间 [CI]:1.18 至 2.75])和小医院规模(OR:1.93;95% CI:1.18 至 3.16)是有害处方行为的最强、独立相关的决定因素。结论 在 HF 住院后,通常会继续或开始使用会加重 HF 的药物治疗方案。这些发现强调了持续需要制定策略来改善这一弱势群体的安全处方实践。



























 京公网安备 11010802027423号
京公网安备 11010802027423号