当前位置:
X-MOL 学术
›
Prostate Cancer Prostatic. Dis.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Temporal trends and social barriers for inpatient palliative care delivery in metastatic prostate cancer patients receiving critical care therapies.
Prostate Cancer and Prostatic Diseases ( IF 4.8 ) Pub Date : 2019-11-04 , DOI: 10.1038/s41391-019-0183-9 Elio Mazzone 1, 2, 3 , Francesco A Mistretta 1, 4 , Sophie Knipper 1, 5 , Zhe Tian 1 , Carlotta Palumbo 1, 6 , Giorgio Gandaglia 2, 3 , Nicola Fossati 2, 3 , Shahrokh F Shariat 7 , Fred Saad 1, 8 , Francesco Montorsi 2, 3 , Markus Graefen 5 , Alberto Briganti 2, 3 , Pierre I Karakiewicz 1, 8
Prostate Cancer and Prostatic Diseases ( IF 4.8 ) Pub Date : 2019-11-04 , DOI: 10.1038/s41391-019-0183-9 Elio Mazzone 1, 2, 3 , Francesco A Mistretta 1, 4 , Sophie Knipper 1, 5 , Zhe Tian 1 , Carlotta Palumbo 1, 6 , Giorgio Gandaglia 2, 3 , Nicola Fossati 2, 3 , Shahrokh F Shariat 7 , Fred Saad 1, 8 , Francesco Montorsi 2, 3 , Markus Graefen 5 , Alberto Briganti 2, 3 , Pierre I Karakiewicz 1, 8
Affiliation
|
BACKGROUND
Use of inpatient palliative care (IPC) in advanced cancer patients represents a well-established guideline recommendation. A recent analysis demonstrated that genitourinary (GU) cancer patients benefited of IPC at the second lowest rate within the four examined primaries, namely lung, breast, colorectal, and GU. Based on this observation, we examined temporal trends and predictors of IPC use in metastatic prostate cancer patients receiving critical care therapies (CCT).
MATERIALS AND METHODS
We identified mPCa patients receiving CCT within the Nationwide Inpatient Sample database (2004-2015). IPC use rates were evaluated using univariable estimated annual percentage changes analyses. Multivariable logistic regression (MLR) models were used after adjustment for clustering at hospital level.
RESULTS
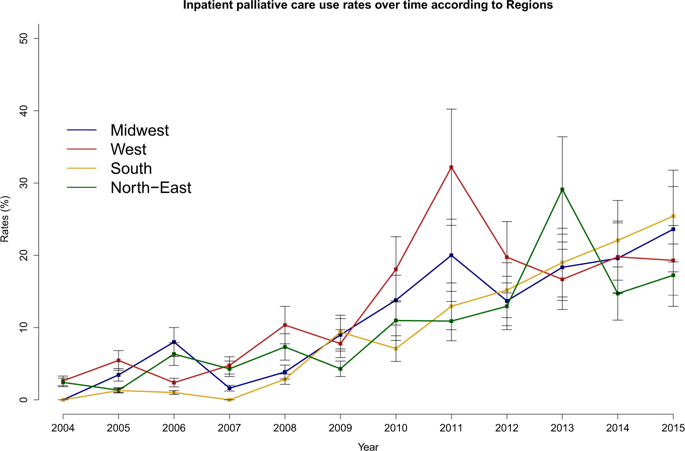
Of 4168 mPCa patients receiving CCT, 449 (11.3%) received IPC. IPC use increased from 1.2 to 22.3% (EAPC: +19.6%, p < 0.001). After stratification according to regions, race, and teaching status, the highest increase of IPC use was recorded in the South (from 0 to 25.4 %, EAPC: +27.6%), in Caucasians (from 1.5 to 24.4 %, EAPC: +19.8%; p < 0.001) and in teaching hospitals (from 0.9 to 26.2 %, EAPC: +19.6%; p < 0.001). In MLR models, teaching status (Odds ratio [OR]: 1.74, p < 0.001) and contemporary year interval (OR: 4.63, p < 0.001) were associated with higher IPC rates. Conversely, African American race (OR: 0.66, p < 0.001) and primary diagnosis of GU disorders (OR: 0.49, p < 0.001) and gastrointestinal (GI) disorders at admission (OR: 0.61, p = 0.02) were associated with lower IPC rates.
CONCLUSIONS
IPC use rate in mPCa patients receiving CCT sharply increased between 2004 and 2015. The highest increase of IPC use across time was recorded in the South, in Caucasian race, and in teaching hospitals. African-American race and nonteaching status were identified as independent predictors of lower IPC use and represent targets for efforts aimed at improving IPC delivery in mPCa patients receiving CCT.
中文翻译:

在接受重症监护治疗的转移性前列腺癌患者中,姑息治疗分娩的时间趋势和社会障碍。
背景技术在晚期癌症患者中使用住院姑息治疗(IPC)代表了已确立的指南推荐。最近的一项分析表明,泌尿生殖道(GU)癌症患者受益于IPC的IPC率在四个被检查的主要肺脏,乳腺癌,结肠直肠癌和GU中为次低。基于此观察,我们检查了接受重症监护疗法(CCT)的转移性前列腺癌患者的IPC使用的时间趋势和预测因素。材料与方法我们在全国住院患者样本数据库(2004-2015年)中确定了接受CCT的mPCa患者。使用单变量估计的年度百分比变化分析来评估IPC使用率。在医院级别进行聚类调整后,使用多变量logistic回归(MLR)模型。结果4168名接受CCT的mPCa患者中,449个(11.3%)获得了IPC。IPC使用率从1.2%增加到22.3%(EAPC:+ 19.6%,p <0.001)。根据地区,种族和教学状况进行分层后,在南部地区,使用IPC的增长最高(从0增至25.4%,EAPC:+ 27.6%),在白种人中(从1.5增至24.4%,EAPC:+19.8) %; p <0.001)和教学医院(从0.9到26.2%,EAPC:+ 19.6%; p <0.001)。在MLR模型中,教学状态(几率[OR]:1.74,p <0.001)和当代年间隔(OR:4.63,p <0.001)与较高的IPC率相关。相反,入院时非裔美国人种族(OR:0.66,p <0.001)和GU疾病的初步诊断(OR:0.49,p <0.001)和胃肠道(GI)疾病(OR:0.61,p = 0.02)与低血脂症相关IPC费率。结论2004年至2015年间,接受CCT的mPCa患者的IPC使用率急剧上升。在南方,高加索人种和教学医院中,IPC使用率随时间的增长最高。非裔美国人的种族和非教学状况被确定为IPC使用率降低的独立预测因素,并且代表着旨在改善接受CCT的mPCa患者IPC递送的努力目标。
更新日期:2019-11-04
中文翻译:

在接受重症监护治疗的转移性前列腺癌患者中,姑息治疗分娩的时间趋势和社会障碍。
背景技术在晚期癌症患者中使用住院姑息治疗(IPC)代表了已确立的指南推荐。最近的一项分析表明,泌尿生殖道(GU)癌症患者受益于IPC的IPC率在四个被检查的主要肺脏,乳腺癌,结肠直肠癌和GU中为次低。基于此观察,我们检查了接受重症监护疗法(CCT)的转移性前列腺癌患者的IPC使用的时间趋势和预测因素。材料与方法我们在全国住院患者样本数据库(2004-2015年)中确定了接受CCT的mPCa患者。使用单变量估计的年度百分比变化分析来评估IPC使用率。在医院级别进行聚类调整后,使用多变量logistic回归(MLR)模型。结果4168名接受CCT的mPCa患者中,449个(11.3%)获得了IPC。IPC使用率从1.2%增加到22.3%(EAPC:+ 19.6%,p <0.001)。根据地区,种族和教学状况进行分层后,在南部地区,使用IPC的增长最高(从0增至25.4%,EAPC:+ 27.6%),在白种人中(从1.5增至24.4%,EAPC:+19.8) %; p <0.001)和教学医院(从0.9到26.2%,EAPC:+ 19.6%; p <0.001)。在MLR模型中,教学状态(几率[OR]:1.74,p <0.001)和当代年间隔(OR:4.63,p <0.001)与较高的IPC率相关。相反,入院时非裔美国人种族(OR:0.66,p <0.001)和GU疾病的初步诊断(OR:0.49,p <0.001)和胃肠道(GI)疾病(OR:0.61,p = 0.02)与低血脂症相关IPC费率。结论2004年至2015年间,接受CCT的mPCa患者的IPC使用率急剧上升。在南方,高加索人种和教学医院中,IPC使用率随时间的增长最高。非裔美国人的种族和非教学状况被确定为IPC使用率降低的独立预测因素,并且代表着旨在改善接受CCT的mPCa患者IPC递送的努力目标。



























 京公网安备 11010802027423号
京公网安备 11010802027423号