当前位置:
X-MOL 学术
›
Am. J. Transplant.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
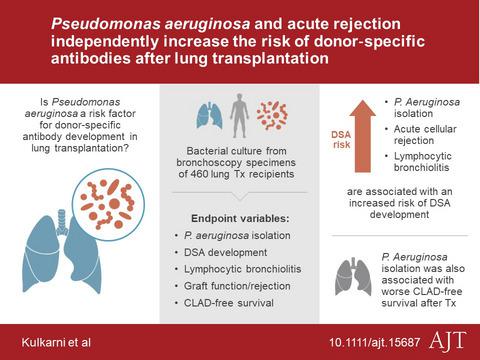
Pseudomonas aeruginosa and acute rejection independently increase the risk of donor-specific antibodies after lung transplantation.
American Journal of Transplantation ( IF 8.8 ) Pub Date : 2019-12-24 , DOI: 10.1111/ajt.15687 Hrishikesh S Kulkarni 1 , Kevin Tsui 2 , Suraj Sunder 1 , Alex Ganninger 1 , Laneshia K Tague 1 , Chad A Witt 1 , Derek E Byers 1 , Elbert P Trulock 1 , Ruben Nava 3 , Varun Puri 3 , Daniel Kreisel 3 , Thalachallour Mohanakumar 4 , Andrew E Gelman 3, 5 , Ramsey R Hachem 1
American Journal of Transplantation ( IF 8.8 ) Pub Date : 2019-12-24 , DOI: 10.1111/ajt.15687 Hrishikesh S Kulkarni 1 , Kevin Tsui 2 , Suraj Sunder 1 , Alex Ganninger 1 , Laneshia K Tague 1 , Chad A Witt 1 , Derek E Byers 1 , Elbert P Trulock 1 , Ruben Nava 3 , Varun Puri 3 , Daniel Kreisel 3 , Thalachallour Mohanakumar 4 , Andrew E Gelman 3, 5 , Ramsey R Hachem 1
Affiliation
|
Factors contributing to donor-specific HLA antibody (DSA) development after lung transplantation have not been systematically evaluated. We hypothesized that the isolation of Pseudomonas aeruginosa in respiratory specimens would increase the risk of DSA development. Our objective was to determine the risk of DSA development associated with the isolation of Pseudomonas aeruginosa after lung transplantation. We conducted a single-center retrospective cohort study of primary lung transplant recipients and examined risk factors for DSA development using Cox regression models. Of 460 recipients, 205 (45%) developed DSA; the majority developed Class II DSA (n = 175, 85%), and 145 of 205 (71%) developed DSA to HLA-DQ alleles. Univariate time-dependent analyses revealed that isolation of Pseudomonas from respiratory specimens, acute cellular rejection, and lymphocytic bronchiolitis are associated with an increased risk of DSA development. In multivariable analyses, Pseudomonas isolation, acute cellular rejection, and lymphocytic bronchiolitis remained independent risk factors for DSA development. Additionally, there was a direct association between the number of positive Pseudomonas cultures and the risk of DSA development. Our findings suggest that pro-inflammatory events including acute cellular rejection, lymphocytic bronchiolitis, and Pseudomonas isolation after transplantation are associated with an increased risk of DSA development.
中文翻译:

铜绿假单胞菌和急性排斥反应独立增加肺移植后供体特异性抗体的风险。
肺移植后促成供体特异性 HLA 抗体 (DSA) 发展的因素尚未得到系统评估。我们假设在呼吸道标本中分离出铜绿假单胞菌会增加 DSA 发展的风险。我们的目标是确定与肺移植后铜绿假单胞菌分离相关的 DSA 发展风险。我们对原发性肺移植受者进行了一项单中心回顾性队列研究,并使用 Cox 回归模型检查了 DSA 发展的危险因素。在 460 名接受者中,205 名 (45%) 发展为 DSA;大多数人发展为 II 类 DSA(n = 175,85%),205 人中有 145 人(71%)发展为 HLA-DQ 等位基因的 DSA。单变量时间相关分析表明,从呼吸道标本中分离出假单胞菌、急性细胞排斥反应、和淋巴细胞性细支气管炎与 DSA 发展的风险增加有关。在多变量分析中,假单胞菌分离、急性细胞排斥反应和淋巴细胞性细支气管炎仍然是 DSA 发展的独立危险因素。此外,阳性假单胞菌培养物的数量与 DSA 发展的风险之间存在直接关联。我们的研究结果表明,促炎事件(包括急性细胞排斥反应、淋巴细胞性细支气管炎和移植后的假单胞菌分离)与 DSA 发展的风险增加有关。阳性假单胞菌培养物的数量与 DSA 发展的风险之间存在直接关联。我们的研究结果表明,促炎事件(包括急性细胞排斥反应、淋巴细胞性细支气管炎和移植后的假单胞菌分离)与 DSA 发展的风险增加有关。阳性假单胞菌培养物的数量与 DSA 发展的风险之间存在直接关联。我们的研究结果表明,促炎事件(包括急性细胞排斥反应、淋巴细胞性细支气管炎和移植后的假单胞菌分离)与 DSA 发展的风险增加有关。
更新日期:2019-12-24
中文翻译:

铜绿假单胞菌和急性排斥反应独立增加肺移植后供体特异性抗体的风险。
肺移植后促成供体特异性 HLA 抗体 (DSA) 发展的因素尚未得到系统评估。我们假设在呼吸道标本中分离出铜绿假单胞菌会增加 DSA 发展的风险。我们的目标是确定与肺移植后铜绿假单胞菌分离相关的 DSA 发展风险。我们对原发性肺移植受者进行了一项单中心回顾性队列研究,并使用 Cox 回归模型检查了 DSA 发展的危险因素。在 460 名接受者中,205 名 (45%) 发展为 DSA;大多数人发展为 II 类 DSA(n = 175,85%),205 人中有 145 人(71%)发展为 HLA-DQ 等位基因的 DSA。单变量时间相关分析表明,从呼吸道标本中分离出假单胞菌、急性细胞排斥反应、和淋巴细胞性细支气管炎与 DSA 发展的风险增加有关。在多变量分析中,假单胞菌分离、急性细胞排斥反应和淋巴细胞性细支气管炎仍然是 DSA 发展的独立危险因素。此外,阳性假单胞菌培养物的数量与 DSA 发展的风险之间存在直接关联。我们的研究结果表明,促炎事件(包括急性细胞排斥反应、淋巴细胞性细支气管炎和移植后的假单胞菌分离)与 DSA 发展的风险增加有关。阳性假单胞菌培养物的数量与 DSA 发展的风险之间存在直接关联。我们的研究结果表明,促炎事件(包括急性细胞排斥反应、淋巴细胞性细支气管炎和移植后的假单胞菌分离)与 DSA 发展的风险增加有关。阳性假单胞菌培养物的数量与 DSA 发展的风险之间存在直接关联。我们的研究结果表明,促炎事件(包括急性细胞排斥反应、淋巴细胞性细支气管炎和移植后的假单胞菌分离)与 DSA 发展的风险增加有关。



























 京公网安备 11010802027423号
京公网安备 11010802027423号