当前位置:
X-MOL 学术
›
Lancet Diabetes Endocrinol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Gastric bypass versus sleeve gastrectomy in patients with type 2 diabetes (Oseberg): a single-centre, triple-blind, randomised controlled trial.
The Lancet Diabetes & Endocrinology ( IF 44.5 ) Pub Date : 2019-10-31 , DOI: 10.1016/s2213-8587(19)30344-4 Dag Hofsø 1 , Farhat Fatima 2 , Heidi Borgeraas 1 , Kåre Inge Birkeland 3 , Hanne Løvdal Gulseth 4 , Jens Kristoffer Hertel 1 , Line Kristin Johnson 1 , Morten Lindberg 5 , Njord Nordstrand 1 , Milada Cvancarova Småstuen 6 , Darko Stefanovski 7 , Marius Svanevik 8 , Tone Gretland Valderhaug 9 , Rune Sandbu 10 , Jøran Hjelmesæth 11
The Lancet Diabetes & Endocrinology ( IF 44.5 ) Pub Date : 2019-10-31 , DOI: 10.1016/s2213-8587(19)30344-4 Dag Hofsø 1 , Farhat Fatima 2 , Heidi Borgeraas 1 , Kåre Inge Birkeland 3 , Hanne Løvdal Gulseth 4 , Jens Kristoffer Hertel 1 , Line Kristin Johnson 1 , Morten Lindberg 5 , Njord Nordstrand 1 , Milada Cvancarova Småstuen 6 , Darko Stefanovski 7 , Marius Svanevik 8 , Tone Gretland Valderhaug 9 , Rune Sandbu 10 , Jøran Hjelmesæth 11
Affiliation
|
BACKGROUND
For patients with obesity and type 2 diabetes, weight loss improves insulin sensitivity and β-cell function, and can induce remission of diabetes. The comparative efficacy of various bariatric procedures for the remission of type 2 diabetes has not been fully elucidated. We aimed to compare the effects of the two most common bariatric procedures, gastric bypass and sleeve gastrectomy, on remission of diabetes and β-cell function.
METHODS
We conducted a single-centre, triple-blind, randomised trial at Vestfold Hospital Trust (Tønsberg, Norway), in which patients (aged ≥18 years) with type 2 diabetes and obesity were randomly assigned (1:1) to receive gastric bypass or sleeve gastrectomy (the Oseberg study). Randomisation was performed with a computerised random number generator and a block size of 10. Treatment allocation was masked from participants, study personnel, and outcome assessors and was concealed with sealed opaque envelopes. Surgeons used identical skin incisions during both surgeries and were not involved in patient follow-up. The primary clinical outcome was the proportion of participants with complete remission of type 2 diabetes (HbA1c of ≤6·0% [42 mmol/mol] without the use of glucose-lowering medication) at 1 year after surgery. The primary physiological outcome was disposition index (a measure of β-cell function) at 1 year after surgery, as assessed by an intravenous glucose tolerance test. Primary outcomes were analysed in the intention-to-treat and per-protocol populations. This trial is ongoing and closed to recruitment, and is registered with ClinicalTrials.gov, NCT01778738.
FINDINGS
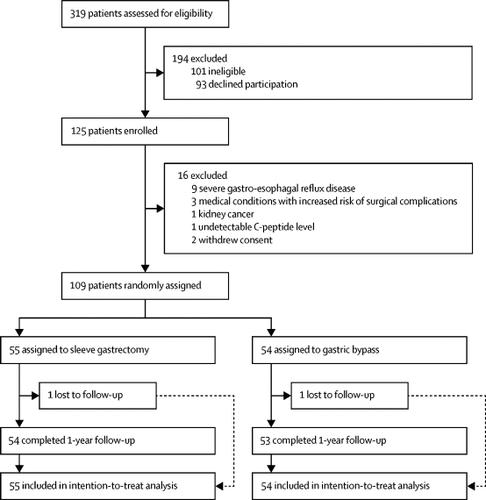
Between Oct 15, 2012, and Sept 1, 2017, 1305 patients who were preparing for bariatric surgery were screened, of whom 319 consecutive patients with type 2 diabetes were assessed for eligibility. 109 patients were enrolled and randomly assigned to gastric bypass (n=54) or sleeve gastrectomy (n=55). 107 (98%) of 109 patients completed 1-year follow-up, with one patient in each group withdrawing after surgery (per-protocol population). In the intention-to-treat population, diabetes remission rates were higher in the gastric bypass group than in the sleeve gastrectomy group (risk difference 27% [95% CI 10 to 44]; relative risk [RR] 1·57 [1·14 to 2·16], p=0·0054); results were similar in the per-protocol population (risk difference 27% [95% CI 10 to 45]; RR 1·57 [1·14 to 2·15], p=0·0036). In the intention-to-treat population, disposition index increased in both groups (between-group difference 55 [-111 to 220], p=0·52); results were similar in the per-protocol population (between-group difference 21 [-214 to 256], p=0.86). In the gastric bypass group, ten of 54 participants had early complications and 17 of 53 had late side-effects. In the sleeve gastrectomy group, eight of 55 participants had early complications and 22 of 54 had late side-effects. No deaths occurred in either group.
INTERPRETATION
Gastric bypass was found to be superior to sleeve gastrectomy for remission of type 2 diabetes at 1 year after surgery, and the two procedures had a similar beneficial effect on β-cell function. The use of gastric bypass as the preferred bariatric procedure for patients with obesity and type 2 diabetes could improve diabetes care and reduce related societal costs.
FUNDING
Morbid Obesity Centre, Vestfold Hospital Trust.
中文翻译:

2型糖尿病患者的胃旁路搭桥术与袖式胃切除术(Oseberg):一项单中心,三盲,随机对照试验。
背景技术对于肥胖症和2型糖尿病患者,减肥可以改善胰岛素敏感性和β细胞功能,并可以诱导糖尿病的缓解。各种减肥手术缓解2型糖尿病的相对疗效尚未完全阐明。我们旨在比较两种最常见的减肥手术(胃旁路手术和袖式胃切除术)对糖尿病缓解和β细胞功能的影响。方法我们在Vestfold Hospital Trust(挪威Tønsberg)进行了单中心,三盲,随机试验,其中将年龄≥18岁的2型糖尿病和肥胖患者随机分配(1:1)接受胃旁路或袖式胃切除术(Oseberg研究)。随机化是通过计算机随机数生成器进行的,块大小为10。参与者,研究人员和结果评估者都掩盖了治疗方案,并用密封的不透明信封掩盖了治疗方案。外科医生在两次手术中均使用了相同的皮肤切口,并且未参与患者的随访。主要的临床结局是术后1年完全缓解2型糖尿病(HbA1c≤6·0%[42 mmol / mol]且未使用降糖药)的参与者比例。主要的生理结果是手术后1年的处置指数(衡量β细胞功能),通过静脉糖耐量试验评估。在意向性治疗和按方案人群中分析了主要结局。该试验正在进行中,尚未招募,已在ClinicalTrials.gov上注册,编号NCT01778738。调查结果:2012年10月15日至9月1日 2017年,对准备减肥手术的1305例患者进行了筛查,其中319例连续的2型糖尿病患者被纳入资格评估。109例患者被纳入研究并随机分配到胃旁路术(n = 54)或套管胃切除术(n = 55)。109位患者中有107位(98%)完成了1年的随访,每组中有1位患者在手术后退出(按协议人群)。在意向性治疗人群中,胃旁路手术组的糖尿病缓解率高于套管胃切除术组(风险差异27%[95%CI 10至44];相对风险[RR] 1·57 [1· 14至2·16],p = 0·0054);按协议人群的结果相似(风险差异27%[95%CI 10至45]; RR 1·57 [1·14至2·15],p = 0·0036)。在意向治疗人群中,两组的处置指数均增加(组间差异55 [-111至220],p = 0·52);每个协议人群的结果相似(组间差异21 [-214至256],p = 0.86)。在胃旁路手术组中,有54名参与者中有10名有早期并发症,有53名参与者中有17名有较晚的副作用。在袖式胃切除术组中,55位参与者中有8位早期并发症,54位参与者中有22位副作用较晚。两组均未发生死亡。解释术后1年,胃旁路术在2型糖尿病缓解方面优于套管胃切除术,并且两种手术对β细胞功能具有相似的有益作用。对于肥胖症和2型糖尿病患者,使用胃旁路作为首选的减肥方法可以改善糖尿病护理并降低相关的社会成本。
更新日期:2019-11-20
中文翻译:

2型糖尿病患者的胃旁路搭桥术与袖式胃切除术(Oseberg):一项单中心,三盲,随机对照试验。
背景技术对于肥胖症和2型糖尿病患者,减肥可以改善胰岛素敏感性和β细胞功能,并可以诱导糖尿病的缓解。各种减肥手术缓解2型糖尿病的相对疗效尚未完全阐明。我们旨在比较两种最常见的减肥手术(胃旁路手术和袖式胃切除术)对糖尿病缓解和β细胞功能的影响。方法我们在Vestfold Hospital Trust(挪威Tønsberg)进行了单中心,三盲,随机试验,其中将年龄≥18岁的2型糖尿病和肥胖患者随机分配(1:1)接受胃旁路或袖式胃切除术(Oseberg研究)。随机化是通过计算机随机数生成器进行的,块大小为10。参与者,研究人员和结果评估者都掩盖了治疗方案,并用密封的不透明信封掩盖了治疗方案。外科医生在两次手术中均使用了相同的皮肤切口,并且未参与患者的随访。主要的临床结局是术后1年完全缓解2型糖尿病(HbA1c≤6·0%[42 mmol / mol]且未使用降糖药)的参与者比例。主要的生理结果是手术后1年的处置指数(衡量β细胞功能),通过静脉糖耐量试验评估。在意向性治疗和按方案人群中分析了主要结局。该试验正在进行中,尚未招募,已在ClinicalTrials.gov上注册,编号NCT01778738。调查结果:2012年10月15日至9月1日 2017年,对准备减肥手术的1305例患者进行了筛查,其中319例连续的2型糖尿病患者被纳入资格评估。109例患者被纳入研究并随机分配到胃旁路术(n = 54)或套管胃切除术(n = 55)。109位患者中有107位(98%)完成了1年的随访,每组中有1位患者在手术后退出(按协议人群)。在意向性治疗人群中,胃旁路手术组的糖尿病缓解率高于套管胃切除术组(风险差异27%[95%CI 10至44];相对风险[RR] 1·57 [1· 14至2·16],p = 0·0054);按协议人群的结果相似(风险差异27%[95%CI 10至45]; RR 1·57 [1·14至2·15],p = 0·0036)。在意向治疗人群中,两组的处置指数均增加(组间差异55 [-111至220],p = 0·52);每个协议人群的结果相似(组间差异21 [-214至256],p = 0.86)。在胃旁路手术组中,有54名参与者中有10名有早期并发症,有53名参与者中有17名有较晚的副作用。在袖式胃切除术组中,55位参与者中有8位早期并发症,54位参与者中有22位副作用较晚。两组均未发生死亡。解释术后1年,胃旁路术在2型糖尿病缓解方面优于套管胃切除术,并且两种手术对β细胞功能具有相似的有益作用。对于肥胖症和2型糖尿病患者,使用胃旁路作为首选的减肥方法可以改善糖尿病护理并降低相关的社会成本。



























 京公网安备 11010802027423号
京公网安备 11010802027423号