当前位置:
X-MOL 学术
›
JAMA Surg.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Association of Practitioner Interfacility Triage Performance With Outcomes for Severely Injured Patients With Fee-for-Service Medicare Insurance.
JAMA Surgery ( IF 16.9 ) Pub Date : 2019-12-18 , DOI: 10.1001/jamasurg.2019.3944 Deepika Mohan 1, 2 , David J Wallace 1, 3 , Samantha J Kerti 1 , Derek C Angus 1 , Matthew R Rosengart 1, 2 , Amber E Barnato 4 , Donald M Yealy 3 , Baruch Fischhoff 5 , Chung-Chou Chang 1 , Jeremy M Kahn 1
JAMA Surgery ( IF 16.9 ) Pub Date : 2019-12-18 , DOI: 10.1001/jamasurg.2019.3944 Deepika Mohan 1, 2 , David J Wallace 1, 3 , Samantha J Kerti 1 , Derek C Angus 1 , Matthew R Rosengart 1, 2 , Amber E Barnato 4 , Donald M Yealy 3 , Baruch Fischhoff 5 , Chung-Chou Chang 1 , Jeremy M Kahn 1
Affiliation
|
Importance
Despite evidence that treatment of severely injured patients at trauma centers is associated with reduced mortality, nearly half of all such patients are treated at nontrauma centers (undertriaged). Little is known about whether interfacility undertriage occurs because of practitioner decision-making or institutional and regional factors.
Objectives
To assess the associations between variation in triage practitioners at nontrauma centers and between practitioner-level variation and patient outcomes after injury.
Design, Setting, and Participants
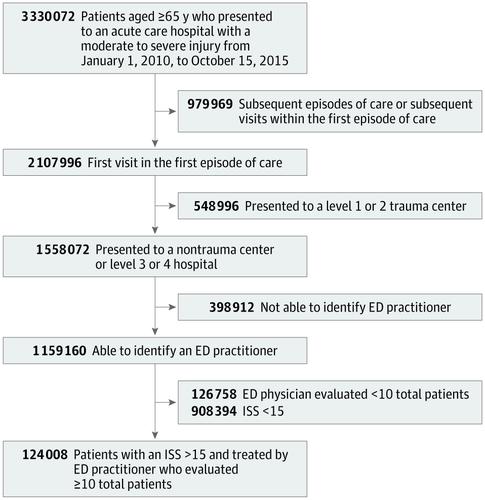
This retrospective cohort study used Medicare claims data from severely injured patients presenting to nontrauma centers and the practitioners who evaluated them in the emergency department from January 1, 2010, to October 15, 2015. Data analysis was performed from January 15, 2018, to March 21, 2019.
Main Outcomes and Measures
Proportion of variation in undertriage associated with practitioners, practitioner rates of undertriage, practitioner characteristics associated with undertriage, and 30-day case-fatality rate.
Results
A total of 124 008 severely injured patients (mean [SD] age, 81 [8.4] years; 67 253 [54.2%] female) and the 25 376 practitioners (5564 [21.9%] female) who evaluated the patients in the emergency department of nontrauma centers were included in the study. Undertriage occurred among 85 403 patients (68.9%), with 40.6% of total variation associated with practitioners, 37.8% with hospitals, and 6.7% with regions. Compared with physicians with National Provider Identification (NPI) enumeration before 2007, those with an NPI enumerated between 2007 and 2010 had an undertriage risk ratio (RR) of 0.98 (95% CI, 0.97-0.99), and those with an NPI enumerated after 2010 had an undertriage RR of 0.96 (95% CI, 0.94-0.99). Hospitals with neurosurgeons had an undertriage RR of 1.51 (95% CI, 1.45-1.57) compared with those that did not; hospitals with spine surgeons had an undertriage RR of 1.10 (95% CI, 1.06-1.13); hospitals with general surgeons had an undertriage RR of 1.13 (95% CI, 1.09-1.17). Compared with practitioners who undertriaged 25% or less of patients, a statistically significant increase was found in the odds of death for patients treated by practitioners with a triage rate of less than 25% to 50% (odds ratio [OR], 1.08; 95% CI, 1.05-1.20) and less than 50% to 75% undertriage (OR, 1.12; 95% CI, 1.09-1.26) but not undertriage at greater than 75% (OR, 1.03, 95% CI, 1.00-1.18). In sensitivity analyses to adjust for unmeasured confounding, the association between triage practices and the case fatality rate became monotonic; compared with patients treated by practitioners with an undertriage rate of 25% or less, the odds of case fatality were 1.13 (95% CI, 1.05-1.21; P = .001) among patients treated by practitioners with undertriage rates less than 25% to 50%, 1.22 (95% CI, 1.13-1.32; P < .001) for patients treated by practitioners with undertriage rates less than 50% to 75%, and 1.20 (95% CI, 1.10-1.30; P < .001) for patients treated by practitioners with undertriage rates greater than 75%.
Conclusions and Relevance
The findings suggest that individual practitioner practices are an important source of variation in triage and represent a potential locus of intervention to reduce preventable deaths after injury.
中文翻译:

患有按服务付费医疗保险的重伤患者的从业人员分流能力与结局的关联。
重要性尽管有证据表明在创伤中心治疗重伤患者会降低死亡率,但所有此类患者中有近一半是在非创伤中心治疗的(未足额的)。关于是否因从业者的决策或机构和地区因素而导致设施不足的分类问题知之甚少。目的评估非创伤中心分诊从业者之间的差异,以及从业者水平上的差异与受伤后患者预后之间的关联。设计,背景和参与者这项回顾性队列研究使用了2010年1月1日至2015年10月15日在非创伤中心就诊的重伤患者的医疗保险数据以及在急诊室对其进行评估的从业人员。数据分析从1月进行。 2018年15月15日,截止到2019年3月21日。主要结果和衡量方法与从业人员相关的未成年人分类的变化率,从业人员的未成年人分类率,与未成年人分类相关的从业人员特征以及30天病死率。结果总共有124 008名重伤患者(平均[SD]年龄,81 [8.4]岁; 67 253 [54.2%]女性)和25 376名从业者(5564 [21.9%]女性)对紧急情况进行了评估这项研究包括非创伤中心的部门。85 403例患者中发生了不足分类,占68.9%,其中从业者中占40.6%,在医院中占37.8%,在地区中占6.7%。与2007年之前采用NPI枚举的医师相比,2007年至2010年枚举NPI的医师的未成年人患病风险比(RR)为0.98(95%CI,0.97-0.99),以及在2010年后枚举的NPI的未成年人分类RR为0.96(95%CI,0.94-0.99)。与没有神经外科医生的医院相比,神经衰弱的医院的分类不足RR为1.51(95%CI,1.45-1.57)。脊柱外科医生的医院的分类不足RR为1.10(95%CI,1.06-1.13);拥有普通外科医师的医院的分类不足RR为1.13(95%CI,1.09-1.17)。与年龄不足25%或更少的患者相比,分诊率低于25%至50%的从业者治疗的患者的死亡几率有统计学上的显着增加(赔率[OR],1.08; 95) CI的百分比(1.05-1.20)和不足发生率的50%至75%以下(OR,1.12; 95%CI,1.09-1.26),但超过75%的不足发生率(OR,1.03,95%CI,1.00-1.18) 。在进行敏感性分析以调整无法衡量的混杂因素时,分诊手法与病死率之间的联系变得单调。与低于25%或更低的未成年人流失率的患者相比,未成年人的未成年人流失率是1.13(95%CI,1.05-1.21; P = .001)。对于从业者的未成年人不足率低于50%至75%的患者,分别为50%,1.22(95%CI,1.13-1.32; P <.001)和1.20(95%CI,1.10-1.30; P <.001)对于未成年人分类率超过75%的从业者治疗的患者。结论与相关性研究结果表明,个体执业医师的实践是分诊差异的重要来源,并且是减少伤害后可预防死亡的潜在干预手段。
更新日期:2019-12-19
中文翻译:

患有按服务付费医疗保险的重伤患者的从业人员分流能力与结局的关联。
重要性尽管有证据表明在创伤中心治疗重伤患者会降低死亡率,但所有此类患者中有近一半是在非创伤中心治疗的(未足额的)。关于是否因从业者的决策或机构和地区因素而导致设施不足的分类问题知之甚少。目的评估非创伤中心分诊从业者之间的差异,以及从业者水平上的差异与受伤后患者预后之间的关联。设计,背景和参与者这项回顾性队列研究使用了2010年1月1日至2015年10月15日在非创伤中心就诊的重伤患者的医疗保险数据以及在急诊室对其进行评估的从业人员。数据分析从1月进行。 2018年15月15日,截止到2019年3月21日。主要结果和衡量方法与从业人员相关的未成年人分类的变化率,从业人员的未成年人分类率,与未成年人分类相关的从业人员特征以及30天病死率。结果总共有124 008名重伤患者(平均[SD]年龄,81 [8.4]岁; 67 253 [54.2%]女性)和25 376名从业者(5564 [21.9%]女性)对紧急情况进行了评估这项研究包括非创伤中心的部门。85 403例患者中发生了不足分类,占68.9%,其中从业者中占40.6%,在医院中占37.8%,在地区中占6.7%。与2007年之前采用NPI枚举的医师相比,2007年至2010年枚举NPI的医师的未成年人患病风险比(RR)为0.98(95%CI,0.97-0.99),以及在2010年后枚举的NPI的未成年人分类RR为0.96(95%CI,0.94-0.99)。与没有神经外科医生的医院相比,神经衰弱的医院的分类不足RR为1.51(95%CI,1.45-1.57)。脊柱外科医生的医院的分类不足RR为1.10(95%CI,1.06-1.13);拥有普通外科医师的医院的分类不足RR为1.13(95%CI,1.09-1.17)。与年龄不足25%或更少的患者相比,分诊率低于25%至50%的从业者治疗的患者的死亡几率有统计学上的显着增加(赔率[OR],1.08; 95) CI的百分比(1.05-1.20)和不足发生率的50%至75%以下(OR,1.12; 95%CI,1.09-1.26),但超过75%的不足发生率(OR,1.03,95%CI,1.00-1.18) 。在进行敏感性分析以调整无法衡量的混杂因素时,分诊手法与病死率之间的联系变得单调。与低于25%或更低的未成年人流失率的患者相比,未成年人的未成年人流失率是1.13(95%CI,1.05-1.21; P = .001)。对于从业者的未成年人不足率低于50%至75%的患者,分别为50%,1.22(95%CI,1.13-1.32; P <.001)和1.20(95%CI,1.10-1.30; P <.001)对于未成年人分类率超过75%的从业者治疗的患者。结论与相关性研究结果表明,个体执业医师的实践是分诊差异的重要来源,并且是减少伤害后可预防死亡的潜在干预手段。


























 京公网安备 11010802027423号
京公网安备 11010802027423号