当前位置:
X-MOL 学术
›
Nat. Rev. Clin. Oncol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Combining epigenetic drugs with other therapies for solid tumours - past lessons and future promise.
Nature Reviews Clinical Oncology ( IF 78.8 ) Pub Date : 2019-09-30 , DOI: 10.1038/s41571-019-0267-4 Daphné Morel 1 , Daniel Jeffery 2 , Sandrine Aspeslagh 3 , Geneviève Almouzni 2 , Sophie Postel-Vinay 1, 4
Nature Reviews Clinical Oncology ( IF 78.8 ) Pub Date : 2019-09-30 , DOI: 10.1038/s41571-019-0267-4 Daphné Morel 1 , Daniel Jeffery 2 , Sandrine Aspeslagh 3 , Geneviève Almouzni 2 , Sophie Postel-Vinay 1, 4
Affiliation
|
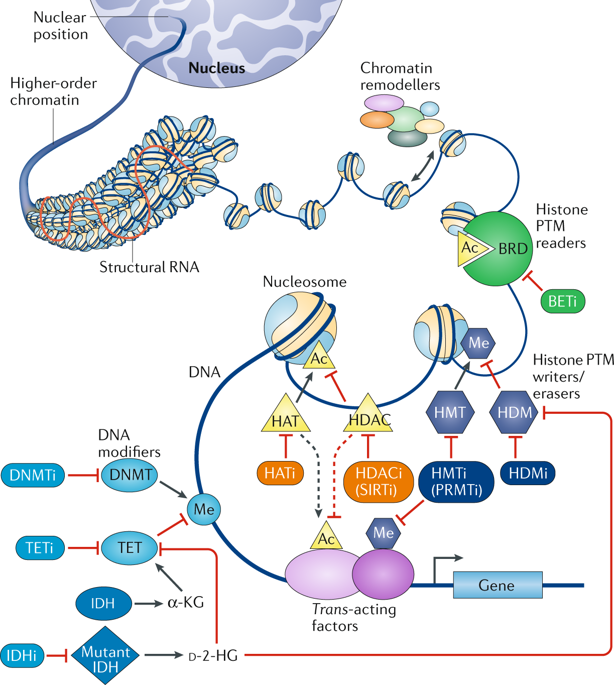
Epigenetic dysregulation has long been recognized as a key factor contributing to tumorigenesis and tumour maintenance that can influence all of the recognized hallmarks of cancer. Despite regulatory approvals for the treatment of certain haematological malignancies, the efficacy of the first generation of epigenetic drugs (epi-drugs) in patients with solid tumours has been disappointing; however, successes have now been achieved in selected solid tumour subtypes, thanks to the development of novel compounds and a better understanding of cancer biology that have enabled precision medicine approaches. Several lines of evidence support that, beyond their potential as monotherapies, epigenetic drugs could have important roles in synergy with other anticancer therapies or in reversing acquired therapy resistance. Herein, we review the mechanisms by which epi-drugs can modulate the sensitivity of cancer cells to other forms of anticancer therapy, including chemotherapy, radiation therapy, hormone therapy, molecularly targeted therapy and immunotherapy. We provide a critical appraisal of the preclinical rationale, completed clinical studies and ongoing clinical trials relating to combination therapies incorporating epi-drugs. Finally, we propose and discuss rational clinical trial designs and drug development strategies, considering key factors including patient selection, tumour biomarker evaluation, drug scheduling and response assessment and study end points, with the aim of optimizing the development of such combinations.
中文翻译:

将表观遗传药物与其他实体瘤疗法相结合——过去的教训和未来的希望。
长期以来,表观遗传失调一直被认为是导致肿瘤发生和肿瘤维持的关键因素,可以影响所有公认的癌症特征。尽管治疗某些血液系统恶性肿瘤获得了监管部门的批准,但第一代表观遗传药物(epi-drugs)在实体瘤患者中的疗效一直令人失望;然而,由于新化合物的开发和对癌症生物学的更好理解,使得精准医学方法成为可能,因此现在在选定的实体瘤亚型中取得了成功。有几条证据支持,除了作为单一疗法的潜力外,表观遗传药物在与其他抗癌疗法的协同作用或逆转获得性疗法抗性方面可能具有重要作用。在此处,我们回顾了表观药物可以调节癌细胞对其他形式的抗癌疗法的敏感性的机制,包括化学疗法、放射疗法、激素疗法、分子靶向疗法和免疫疗法。我们对包含表观药物的联合疗法的临床前基本原理、已完成的临床研究和正在进行的临床试验进行了严格的评估。最后,我们提出并讨论了合理的临床试验设计和药物开发策略,考虑了患者选择、肿瘤生物标志物评估、药物调度和反应评估以及研究终点等关键因素,旨在优化此类组合的开发。激素疗法、分子靶向疗法和免疫疗法。我们对包含表观药物的联合疗法的临床前基本原理、已完成的临床研究和正在进行的临床试验进行了严格的评估。最后,我们提出并讨论了合理的临床试验设计和药物开发策略,考虑了患者选择、肿瘤生物标志物评估、药物调度和反应评估以及研究终点等关键因素,旨在优化此类组合的开发。激素疗法、分子靶向疗法和免疫疗法。我们对包含表观药物的联合疗法的临床前基本原理、已完成的临床研究和正在进行的临床试验进行了严格的评估。最后,我们提出并讨论了合理的临床试验设计和药物开发策略,考虑了患者选择、肿瘤生物标志物评估、药物调度和反应评估以及研究终点等关键因素,旨在优化此类组合的开发。
更新日期:2019-09-30
中文翻译:

将表观遗传药物与其他实体瘤疗法相结合——过去的教训和未来的希望。
长期以来,表观遗传失调一直被认为是导致肿瘤发生和肿瘤维持的关键因素,可以影响所有公认的癌症特征。尽管治疗某些血液系统恶性肿瘤获得了监管部门的批准,但第一代表观遗传药物(epi-drugs)在实体瘤患者中的疗效一直令人失望;然而,由于新化合物的开发和对癌症生物学的更好理解,使得精准医学方法成为可能,因此现在在选定的实体瘤亚型中取得了成功。有几条证据支持,除了作为单一疗法的潜力外,表观遗传药物在与其他抗癌疗法的协同作用或逆转获得性疗法抗性方面可能具有重要作用。在此处,我们回顾了表观药物可以调节癌细胞对其他形式的抗癌疗法的敏感性的机制,包括化学疗法、放射疗法、激素疗法、分子靶向疗法和免疫疗法。我们对包含表观药物的联合疗法的临床前基本原理、已完成的临床研究和正在进行的临床试验进行了严格的评估。最后,我们提出并讨论了合理的临床试验设计和药物开发策略,考虑了患者选择、肿瘤生物标志物评估、药物调度和反应评估以及研究终点等关键因素,旨在优化此类组合的开发。激素疗法、分子靶向疗法和免疫疗法。我们对包含表观药物的联合疗法的临床前基本原理、已完成的临床研究和正在进行的临床试验进行了严格的评估。最后,我们提出并讨论了合理的临床试验设计和药物开发策略,考虑了患者选择、肿瘤生物标志物评估、药物调度和反应评估以及研究终点等关键因素,旨在优化此类组合的开发。激素疗法、分子靶向疗法和免疫疗法。我们对包含表观药物的联合疗法的临床前基本原理、已完成的临床研究和正在进行的临床试验进行了严格的评估。最后,我们提出并讨论了合理的临床试验设计和药物开发策略,考虑了患者选择、肿瘤生物标志物评估、药物调度和反应评估以及研究终点等关键因素,旨在优化此类组合的开发。


























 京公网安备 11010802027423号
京公网安备 11010802027423号