Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Laparoscopic supracervical hysterectomy versus endometrial ablation for women with heavy menstrual bleeding (HEALTH): a parallel-group, open-label, randomised controlled trial.
The Lancet ( IF 168.9 ) Pub Date : 2019-09-12 , DOI: 10.1016/s0140-6736(19)31790-8 Kevin Cooper 1 , Suzanne Breeman 2 , Neil W Scott 3 , Graham Scotland 4 , Justin Clark 5 , Jed Hawe 6 , Robert Hawthorn 7 , Kevin Phillips 8 , Graeme MacLennan 2 , Samantha Wileman 2 , Kirsty McCormack 2 , Rodolfo Hernández 9 , John Norrie 10 , Siladitya Bhattacharya 11 ,
The Lancet ( IF 168.9 ) Pub Date : 2019-09-12 , DOI: 10.1016/s0140-6736(19)31790-8 Kevin Cooper 1 , Suzanne Breeman 2 , Neil W Scott 3 , Graham Scotland 4 , Justin Clark 5 , Jed Hawe 6 , Robert Hawthorn 7 , Kevin Phillips 8 , Graeme MacLennan 2 , Samantha Wileman 2 , Kirsty McCormack 2 , Rodolfo Hernández 9 , John Norrie 10 , Siladitya Bhattacharya 11 ,
Affiliation
|
BACKGROUND
Heavy menstrual bleeding affects 25% of women in the UK, many of whom require surgery to treat it. Hysterectomy is effective but has more complications than endometrial ablation, which is less invasive but ultimately leads to hysterectomy in 20% of women. We compared laparoscopic supracervical hysterectomy with endometrial ablation in women seeking surgical treatment for heavy menstrual bleeding.
METHODS
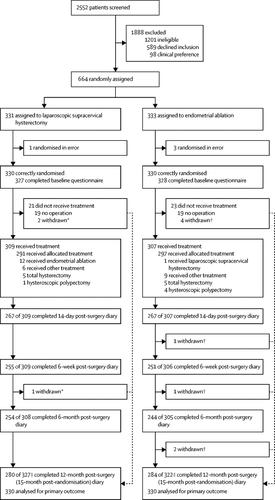
In this parallel-group, multicentre, open-label, randomised controlled trial in 31 hospitals in the UK, women younger than 50 years who were referred to a gynaecologist for surgical treatment of heavy menstrual bleeding and who were eligible for endometrial ablation were randomly allocated (1:1) to either laparoscopic supracervical hysterectomy or second generation endometrial ablation. Women were randomly assigned by either an interactive voice response telephone system or an internet-based application with a minimisation algorithm based on centre and age group (<40 years vs ≥40 years). Laparoscopic supracervical hysterectomy involves laparoscopic (keyhole) surgery to remove the upper part of the uterus (the body) containing the endometrium. Endometrial ablation aims to treat heavy menstrual bleeding by destroying the endometrium, which is responsible for heavy periods. The co-primary clinical outcomes were patient satisfaction and condition-specific quality of life, measured with the menorrhagia multi-attribute quality of life scale (MMAS), assessed at 15 months after randomisation. Our analysis was based on the intention-to-treat principle. The trial was registered with the ISRCTN registry, number ISRCTN49013893.
FINDINGS
Between May 21, 2014, and March 28, 2017, we enrolled and randomly assigned 660 women (330 in each group). 616 (93%) of 660 women were operated on within the study period, 588 (95%) of whom received the allocated procedure and 28 (5%) of whom had an alternative surgery. At 15 months after randomisation, more women allocated to laparoscopic supracervical hysterectomy were satisfied with their operation compared with those in the endometrial ablation group (270 [97%] of 278 women vs 244 [87%] of 280 women; adjusted percentage difference 9·8, 95% CI 5·1-14·5; adjusted odds ratio [OR] 2·53, 95% CI 1·83-3·48; p<0·0001). Women randomly assigned to laparoscopic supracervical hysterectomy were also more likely to have the best possible MMAS score of 100 than women assigned to endometrial ablation (180 [69%] of 262 women vs 146 [54%] of 268 women; adjusted percentage difference 13·3, 95% CI 3·8-22·8; adjusted OR 1·87, 95% CI 1·31-2·67; p=0·00058). 14 (5%) of 309 women in the laparoscopic supracervical hysterectomy group and 11 (4%) of 307 women in the endometrial ablation group had at least one serious adverse event (adjusted OR 1·30, 95% CI 0·56-3·02; p=0·54).
INTERPRETATION
Laparoscopic supracervical hysterectomy is superior to endometrial ablation in terms of clinical effectiveness and has a similar proportion of complications, but takes longer to perform and is associated with a longer recovery.
FUNDING
UK National Institute for Health Research Health Technology Assessment Programme.
中文翻译:

腹腔镜宫颈上子宫切除术与子宫内膜消融术治疗月经过多的女性(健康):一项平行组、开放标签、随机对照试验。
背景 严重的月经出血影响了英国 25% 的女性,其中许多人需要手术治疗。子宫切除术是有效的,但比子宫内膜切除术有更多的并发症,子宫内膜切除术侵入性较小,但最终导致 20% 的女性进行子宫切除术。我们比较了腹腔镜宫颈上子宫切除术和子宫内膜切除术在因月经过多而寻求手术治疗的女性中的效果。方法 在这项在英国 31 家医院进行的平行组、多中心、开放标签、随机对照试验中,50 岁以下被转诊至妇科医生接受大量月经出血手术治疗且符合子宫内膜切除术条件的女性被随机分组分配 (1:1) 至腹腔镜宫颈上子宫切除术或第二代子宫内膜切除术。女性通过交互式语音应答电话系统或基于互联网的应用程序随机分配,该应用程序具有基于中心和年龄组(<40 岁 vs ≥40 岁)的最小化算法。腹腔镜宫颈上子宫切除术涉及腹腔镜(锁孔)手术,以切除包含子宫内膜的子宫(身体)上部。子宫内膜消融术旨在通过破坏导致月经过多的子宫内膜来治疗月经过多。共同主要临床结果是患者满意度和特定条件下的生活质量,使用月经过多多属性生活质量量表 (MMAS) 测量,在随机分组后 15 个月进行评估。我们的分析基于意向治疗原则。该试验已在 ISRCTN 登记处注册,编号为 ISRCTN49013893。2014 年 5 月 21 日至 2017 年 3 月 28 日期间,我们招募并随机分配了 660 名女性(每组 330 名)。660 名女性中有 616 名 (93%) 在研究期间接受了手术,其中 588 名 (95%) 接受了分配的手术,28 名 (5%) 接受了替代手术。随机分组后 15 个月,与子宫内膜切除术组相比,分配到腹腔镜宫颈上子宫切除术的更多女性对其手术感到满意(278 名女性中的 270 [97%] vs 280 名女性中的 244 [87%];调整后的百分比差异 9· 8,95% CI 5·1-14·5;调整后的比值比 [OR] 2·53,95% CI 1·83-3·48;p<0·0001)。被随机分配到腹腔镜宫颈上子宫切除术的女性也比分配到子宫内膜切除术的女性更有可能获得 100 分的最佳 MMAS 评分(262 名女性中的 180 [69%] vs 268 名女性中的 146 [54%];调整后的百分比差异 13· 3,95% CI 3·8-22·8;调整后 OR 1·87,95% CI 1·31-2·67;p=0·00058)。腹腔镜宫颈上子宫切除术组 309 名女性中的 14 名 (5%) 和子宫内膜切除术组 307 名女性中的 11 名 (4%) 至少发生一次严重不良事件(调整后的 OR 1·30,95% CI 0·56-3 ·02;p=0·54)。解释 腹腔镜宫颈上子宫切除术在临床有效性方面优于子宫内膜切除术,并发症的比例相似,但执行时间更长,恢复时间也更长。
更新日期:2019-10-17
中文翻译:

腹腔镜宫颈上子宫切除术与子宫内膜消融术治疗月经过多的女性(健康):一项平行组、开放标签、随机对照试验。
背景 严重的月经出血影响了英国 25% 的女性,其中许多人需要手术治疗。子宫切除术是有效的,但比子宫内膜切除术有更多的并发症,子宫内膜切除术侵入性较小,但最终导致 20% 的女性进行子宫切除术。我们比较了腹腔镜宫颈上子宫切除术和子宫内膜切除术在因月经过多而寻求手术治疗的女性中的效果。方法 在这项在英国 31 家医院进行的平行组、多中心、开放标签、随机对照试验中,50 岁以下被转诊至妇科医生接受大量月经出血手术治疗且符合子宫内膜切除术条件的女性被随机分组分配 (1:1) 至腹腔镜宫颈上子宫切除术或第二代子宫内膜切除术。女性通过交互式语音应答电话系统或基于互联网的应用程序随机分配,该应用程序具有基于中心和年龄组(<40 岁 vs ≥40 岁)的最小化算法。腹腔镜宫颈上子宫切除术涉及腹腔镜(锁孔)手术,以切除包含子宫内膜的子宫(身体)上部。子宫内膜消融术旨在通过破坏导致月经过多的子宫内膜来治疗月经过多。共同主要临床结果是患者满意度和特定条件下的生活质量,使用月经过多多属性生活质量量表 (MMAS) 测量,在随机分组后 15 个月进行评估。我们的分析基于意向治疗原则。该试验已在 ISRCTN 登记处注册,编号为 ISRCTN49013893。2014 年 5 月 21 日至 2017 年 3 月 28 日期间,我们招募并随机分配了 660 名女性(每组 330 名)。660 名女性中有 616 名 (93%) 在研究期间接受了手术,其中 588 名 (95%) 接受了分配的手术,28 名 (5%) 接受了替代手术。随机分组后 15 个月,与子宫内膜切除术组相比,分配到腹腔镜宫颈上子宫切除术的更多女性对其手术感到满意(278 名女性中的 270 [97%] vs 280 名女性中的 244 [87%];调整后的百分比差异 9· 8,95% CI 5·1-14·5;调整后的比值比 [OR] 2·53,95% CI 1·83-3·48;p<0·0001)。被随机分配到腹腔镜宫颈上子宫切除术的女性也比分配到子宫内膜切除术的女性更有可能获得 100 分的最佳 MMAS 评分(262 名女性中的 180 [69%] vs 268 名女性中的 146 [54%];调整后的百分比差异 13· 3,95% CI 3·8-22·8;调整后 OR 1·87,95% CI 1·31-2·67;p=0·00058)。腹腔镜宫颈上子宫切除术组 309 名女性中的 14 名 (5%) 和子宫内膜切除术组 307 名女性中的 11 名 (4%) 至少发生一次严重不良事件(调整后的 OR 1·30,95% CI 0·56-3 ·02;p=0·54)。解释 腹腔镜宫颈上子宫切除术在临床有效性方面优于子宫内膜切除术,并发症的比例相似,但执行时间更长,恢复时间也更长。



























 京公网安备 11010802027423号
京公网安备 11010802027423号