Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Planned early delivery or expectant management for late preterm pre-eclampsia (PHOENIX): a randomised controlled trial.
The Lancet ( IF 168.9 ) Pub Date : 2019-08-28 , DOI: 10.1016/s0140-6736(19)31963-4 Lucy C Chappell 1 , Peter Brocklehurst 2 , Marcus E Green 3 , Rachael Hunter 4 , Pollyanna Hardy 2 , Edmund Juszczak 5 , Louise Linsell 5 , Virginia Chiocchia 5 , Melanie Greenland 5 , Anna Placzek 5 , John Townend 5 , Neil Marlow 6 , Jane Sandall 1 , Andrew Shennan 1 ,
The Lancet ( IF 168.9 ) Pub Date : 2019-08-28 , DOI: 10.1016/s0140-6736(19)31963-4 Lucy C Chappell 1 , Peter Brocklehurst 2 , Marcus E Green 3 , Rachael Hunter 4 , Pollyanna Hardy 2 , Edmund Juszczak 5 , Louise Linsell 5 , Virginia Chiocchia 5 , Melanie Greenland 5 , Anna Placzek 5 , John Townend 5 , Neil Marlow 6 , Jane Sandall 1 , Andrew Shennan 1 ,
Affiliation
|
BACKGROUND
In women with late preterm pre-eclampsia, the optimal time to initiate delivery is unclear because limitation of maternal disease progression needs to be balanced against infant complications. The aim of this trial was to determine whether planned earlier initiation of delivery reduces maternal adverse outcomes without substantial worsening of neonatal or infant outcomes, compared with expectant management (usual care) in women with late preterm pre-eclampsia.
METHODS
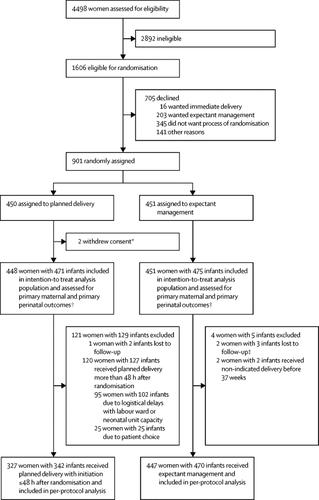
In this parallel-group, non-masked, multicentre, randomised controlled trial done in 46 maternity units across England and Wales, we compared planned delivery versus expectant management (usual care) with individual randomisation in women with late preterm pre-eclampsia from 34 to less than 37 weeks' gestation and a singleton or dichorionic diamniotic twin pregnancy. The co-primary maternal outcome was a composite of maternal morbidity or recorded systolic blood pressure of at least 160 mm Hg with a superiority hypothesis. The co-primary perinatal outcome was a composite of perinatal deaths or neonatal unit admission up to infant hospital discharge with a non-inferiority hypothesis (non-inferiority margin of 10% difference in incidence). Analyses were by intention to treat, together with a per-protocol analysis for the perinatal outcome. The trial was prospectively registered with the ISRCTN registry, ISRCTN01879376. The trial is closed to recruitment but follow-up is ongoing.
FINDINGS
Between Sept 29, 2014, and Dec 10, 2018, 901 women were recruited. 450 women (448 women and 471 infants analysed) were allocated to planned delivery and 451 women (451 women and 475 infants analysed) to expectant management. The incidence of the co-primary maternal outcome was significantly lower in the planned delivery group (289 [65%] women) compared with the expectant management group (338 [75%] women; adjusted relative risk 0·86, 95% CI 0·79-0·94; p=0·0005). The incidence of the co-primary perinatal outcome by intention to treat was significantly higher in the planned delivery group (196 [42%] infants) compared with the expectant management group (159 [34%] infants; 1·26, 1·08-1·47; p=0·0034). The results from the per-protocol analysis were similar. There were nine serious adverse events in the planned delivery group and 12 in the expectant management group.
INTERPRETATION
There is strong evidence to suggest that planned delivery reduces maternal morbidity and severe hypertension compared with expectant management, with more neonatal unit admissions related to prematurity but no indicators of greater neonatal morbidity. This trade-off should be discussed with women with late preterm pre-eclampsia to allow shared decision making on timing of delivery.
FUNDING
National Institute for Health Research Health Technology Assessment Programme.
中文翻译:

计划性早产或晚期子痫前期子痫的预期治疗(PHOENIX):一项随机对照试验。
背景技术在患有早产先兆子痫的妇女中,开始分娩的最佳时间尚不清楚,因为需要平衡母体疾病发展的局限性与婴儿并发症。该试验的目的是确定与早产先兆子痫的妇女进行预期管理(常规护理)相比,计划较早开始分娩是否能在不显着恶化新生儿或婴儿结局的情况下降低母亲的不良结局。方法在这项横跨英格兰和威尔士的46个产妇单位进行的平行,非掩盖,多中心,随机对照试验中,我们比较了计划分娩与预期管理(常规护理)与晚期早产先兆子痫女性的随机分组(34岁)妊娠少于37周,以及单胎或二甲双羊膜双胎妊娠。母婴共存的主要结局是母婴发病率或至少有160 mm Hg的收缩压记录,并具有优越性假设。围产期的主要预后结果是围产期死亡或新生儿入院直至婴儿出院的综合结果,该假设具有非劣效性假设(非劣效性发生率差异为10%)。分析是根据意向进行治疗的,以及对围产期结局的按方案分析。该试验已预先在ISRCTN注册中心ISRCTN01879376注册。该试验尚未招募,但后续行动仍在进行中。调查结果2014年9月29日至2018年12月10日,共招募901名女性。将450名妇女(分析的448名妇女和471名婴儿)分配给计划分娩,并将451名妇女(分析的451名妇女和475名婴儿)分配给孕妇。与预期管理组(338 [75%]名妇女相比,计划分娩组(289名[65%]妇女)的初次孕产妇结局的发生率显着降低;校正后的相对风险0·86,95%CI 0 ·79-0·94; p = 0·0005)。计划分娩组(196 [42%]婴儿)与预期管理组(159 [34%]婴儿; 1·26、1·08)相比,按计划分娩的初次围产期结局预后发生率显着更高-1·47; p = 0·0034)。按协议分析的结果是相似的。计划分娩组中有9例严重不良事件,预期管理组中有12例严重不良事件。解释有强有力的证据表明,与预期管理相比,计划分娩可降低孕产妇发病率和严重高血压,与早产有关的新生儿入院率更高,但没有更高的新生儿发病率指标。应该与早产先兆子痫的妇女讨论这种权衡,以便在分娩时机上共同决策。资助国立卫生研究院健康技术评估计划。
更新日期:2019-09-26
中文翻译:

计划性早产或晚期子痫前期子痫的预期治疗(PHOENIX):一项随机对照试验。
背景技术在患有早产先兆子痫的妇女中,开始分娩的最佳时间尚不清楚,因为需要平衡母体疾病发展的局限性与婴儿并发症。该试验的目的是确定与早产先兆子痫的妇女进行预期管理(常规护理)相比,计划较早开始分娩是否能在不显着恶化新生儿或婴儿结局的情况下降低母亲的不良结局。方法在这项横跨英格兰和威尔士的46个产妇单位进行的平行,非掩盖,多中心,随机对照试验中,我们比较了计划分娩与预期管理(常规护理)与晚期早产先兆子痫女性的随机分组(34岁)妊娠少于37周,以及单胎或二甲双羊膜双胎妊娠。母婴共存的主要结局是母婴发病率或至少有160 mm Hg的收缩压记录,并具有优越性假设。围产期的主要预后结果是围产期死亡或新生儿入院直至婴儿出院的综合结果,该假设具有非劣效性假设(非劣效性发生率差异为10%)。分析是根据意向进行治疗的,以及对围产期结局的按方案分析。该试验已预先在ISRCTN注册中心ISRCTN01879376注册。该试验尚未招募,但后续行动仍在进行中。调查结果2014年9月29日至2018年12月10日,共招募901名女性。将450名妇女(分析的448名妇女和471名婴儿)分配给计划分娩,并将451名妇女(分析的451名妇女和475名婴儿)分配给孕妇。与预期管理组(338 [75%]名妇女相比,计划分娩组(289名[65%]妇女)的初次孕产妇结局的发生率显着降低;校正后的相对风险0·86,95%CI 0 ·79-0·94; p = 0·0005)。计划分娩组(196 [42%]婴儿)与预期管理组(159 [34%]婴儿; 1·26、1·08)相比,按计划分娩的初次围产期结局预后发生率显着更高-1·47; p = 0·0034)。按协议分析的结果是相似的。计划分娩组中有9例严重不良事件,预期管理组中有12例严重不良事件。解释有强有力的证据表明,与预期管理相比,计划分娩可降低孕产妇发病率和严重高血压,与早产有关的新生儿入院率更高,但没有更高的新生儿发病率指标。应该与早产先兆子痫的妇女讨论这种权衡,以便在分娩时机上共同决策。资助国立卫生研究院健康技术评估计划。



























 京公网安备 11010802027423号
京公网安备 11010802027423号