当前位置:
X-MOL 学术
›
Gastroenterology
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Long-term Risk of Colorectal Cancer After Removal of Conventional Adenomas and Serrated Polyps.
Gastroenterology ( IF 29.4 ) Pub Date : 2019-07-11 , DOI: 10.1053/j.gastro.2019.06.039 Xiaosheng He 1 , Dong Hang 2 , Kana Wu 3 , Jennifer Nayor 4 , David A Drew 5 , Edward L Giovannucci 6 , Shuji Ogino 7 , Andrew T Chan 8 , Mingyang Song 9
Gastroenterology ( IF 29.4 ) Pub Date : 2019-07-11 , DOI: 10.1053/j.gastro.2019.06.039 Xiaosheng He 1 , Dong Hang 2 , Kana Wu 3 , Jennifer Nayor 4 , David A Drew 5 , Edward L Giovannucci 6 , Shuji Ogino 7 , Andrew T Chan 8 , Mingyang Song 9
Affiliation
|
BACKGROUND & AIMS
Endoscopic screening reduces incidence and mortality of colorectal cancer (CRC) because precursor lesions, such as conventional adenomas or serrated polyps, are removed. Individuals with polypectomies are advised to undergo colonoscopy surveillance to prevent CRC. However, guidelines for surveillance intervals after diagnosis of a precursor lesion, particularly for individuals with serrated polyps, vary widely, and lack sufficient supporting evidence. Consequently, some high-risk patients do not receive enough surveillance and lower-risk subjects receive excessive surveillance.
METHODS
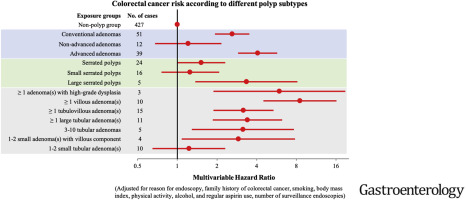
We examined the association between findings from first endoscopy and CRC risk among 122,899 participants who underwent flexible sigmoidoscopy or colonoscopy in the Nurses' Health Study 1 (1990-2012), Nurses' Health Study 2 (1989-2013), or the Health Professionals Follow-up Study (1990-2012). Endoscopic findings were categorized as no polyp, conventional adenoma, or serrated polyp (hyperplastic polyp, traditional serrated adenoma, or sessile serrated adenoma, with or without cytological dysplasia). Conventional adenomas were classified as advanced (≥10 mm, high-grade dysplasia, or tubulovillous or villous histology) or nonadvanced, and serrated polyps were assigned to categories of large (≥10 mm) or small (<10 mm). We used a Cox proportional hazards regression model to calculate the hazard ratios (HRs) of CRC incidence, after adjusting for various potential risk factors.
RESULTS
After a median follow-up period of 10 years, we documented 491 incident cases of CRC: 51 occurred in 6161 participants with conventional adenomas, 24 in 5918 participants with serrated polyps, and 427 in 112,107 participants with no polyp. Compared with participants with no polyp detected during initial endoscopy, the multivariable HR for incident CRC in individuals with an advanced adenoma was 4.07 (95% confidence interval [CI] 2.89-5.72) and the HR for CRC in individuals with a large serrated polyp was 3.35 (95% CI 1.37-8.15). In contrast, there was no significant increase in risk of CRC in patients with nonadvanced adenomas (HR 1.21; 95% CI 0.68-2.16, P = .52) or small serrated polyps (HR 1.25; 95% CI 0.76-2.08; P = .38).
CONCLUSIONS
These findings provide support for guidelines that recommend repeat lower endoscopy within 3 years of a diagnosis of advanced adenoma and large serrated polyps. In contrast, patients with nonadvanced adenoma or small serrated polyps may not require more intensive surveillance than patients without polyps.
中文翻译:

去除常规腺瘤和锯齿状息肉后结直肠癌的长期风险。
背景与目的内镜筛查可减少大肠癌(CRC)的发生率和死亡率,因为可以去除诸如常规腺瘤或锯齿状息肉之类的前体病变。建议有多视现象的人接受结肠镜检查以预防CRC。然而,诊断前体病变后,特别是对于锯齿状息肉的个体,监测间隔的指导原则差异很大,并且缺乏足够的支持证据。因此,一些高危患者没有得到足够的监视,而低危患者则受到了过度监视。方法我们在“护士健康研究1”(1990-2012年),“护士健康研究2”(1989-2013年)中,对接受柔韧性乙状结肠镜或结肠镜检查的122,899名参与者进行了首次内镜检查结果与CRC风险之间的关联性研究,或卫生专业人员跟进研究(1990-2012)。内窥镜检查结果分为无息肉,常规腺瘤或锯齿状息肉(增生性息肉,传统锯齿状腺瘤或无蒂锯齿状腺瘤,伴或不伴细胞学异常)。常规腺瘤分为晚期(≥10mm,高度不典型增生,或微管组织或绒毛组织学)或不进展,并且锯齿状息肉分为大(≥10mm)或小(<10mm)类别。在对各种潜在风险因素进行调整之后,我们使用Cox比例风险回归模型来计算CRC发生的风险比(HRs)。结果在平均随访10年后,我们记录了491例CRC病例:6161例常规腺瘤参与者中有51例发生,5918例有锯齿状息肉的参与者中有24例,112,107名参与者中没有427名,没有息肉。与在初始内窥镜检查中未发现息肉的参与者相比,晚期腺瘤患者的CRC的多变量HR为4.07(95%置信区间[CI] 2.89-5.72),而锯齿状息肉较大的患者的CRC HR为0.07(95%置信区间[CI] 2.89-5.72)。 3.35(95%CI 1.37-8.15)。相反,非晚期腺瘤(HR 1.21; 95%CI 0.68-2.16,P = .52)或细锯齿状息肉(HR 1.25; 95%CI 0.76-2.08; P = .38)。结论这些发现为指南的提出提供了支持,该指南建议在诊断为晚期腺瘤和大锯齿状息肉的3年内再次进行下内镜检查。相比之下,
更新日期:2020-03-05
中文翻译:

去除常规腺瘤和锯齿状息肉后结直肠癌的长期风险。
背景与目的内镜筛查可减少大肠癌(CRC)的发生率和死亡率,因为可以去除诸如常规腺瘤或锯齿状息肉之类的前体病变。建议有多视现象的人接受结肠镜检查以预防CRC。然而,诊断前体病变后,特别是对于锯齿状息肉的个体,监测间隔的指导原则差异很大,并且缺乏足够的支持证据。因此,一些高危患者没有得到足够的监视,而低危患者则受到了过度监视。方法我们在“护士健康研究1”(1990-2012年),“护士健康研究2”(1989-2013年)中,对接受柔韧性乙状结肠镜或结肠镜检查的122,899名参与者进行了首次内镜检查结果与CRC风险之间的关联性研究,或卫生专业人员跟进研究(1990-2012)。内窥镜检查结果分为无息肉,常规腺瘤或锯齿状息肉(增生性息肉,传统锯齿状腺瘤或无蒂锯齿状腺瘤,伴或不伴细胞学异常)。常规腺瘤分为晚期(≥10mm,高度不典型增生,或微管组织或绒毛组织学)或不进展,并且锯齿状息肉分为大(≥10mm)或小(<10mm)类别。在对各种潜在风险因素进行调整之后,我们使用Cox比例风险回归模型来计算CRC发生的风险比(HRs)。结果在平均随访10年后,我们记录了491例CRC病例:6161例常规腺瘤参与者中有51例发生,5918例有锯齿状息肉的参与者中有24例,112,107名参与者中没有427名,没有息肉。与在初始内窥镜检查中未发现息肉的参与者相比,晚期腺瘤患者的CRC的多变量HR为4.07(95%置信区间[CI] 2.89-5.72),而锯齿状息肉较大的患者的CRC HR为0.07(95%置信区间[CI] 2.89-5.72)。 3.35(95%CI 1.37-8.15)。相反,非晚期腺瘤(HR 1.21; 95%CI 0.68-2.16,P = .52)或细锯齿状息肉(HR 1.25; 95%CI 0.76-2.08; P = .38)。结论这些发现为指南的提出提供了支持,该指南建议在诊断为晚期腺瘤和大锯齿状息肉的3年内再次进行下内镜检查。相比之下,


























 京公网安备 11010802027423号
京公网安备 11010802027423号