当前位置:
X-MOL 学术
›
Int. J. Oral Sci.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Periodontitis-induced systemic inflammation exacerbates atherosclerosis partly via endothelial-mesenchymal transition in mice.
International Journal of Oral Science ( IF 14.9 ) Pub Date : 2019-07-01 , DOI: 10.1038/s41368-019-0054-1 Jin Sook Suh 1 , Sol Kim 1 , Kristina I Boström 2 , Cun-Yu Wang 3, 4, 5 , Reuben H Kim 1, 4 , No-Hee Park 1, 2, 4
International Journal of Oral Science ( IF 14.9 ) Pub Date : 2019-07-01 , DOI: 10.1038/s41368-019-0054-1 Jin Sook Suh 1 , Sol Kim 1 , Kristina I Boström 2 , Cun-Yu Wang 3, 4, 5 , Reuben H Kim 1, 4 , No-Hee Park 1, 2, 4
Affiliation
|
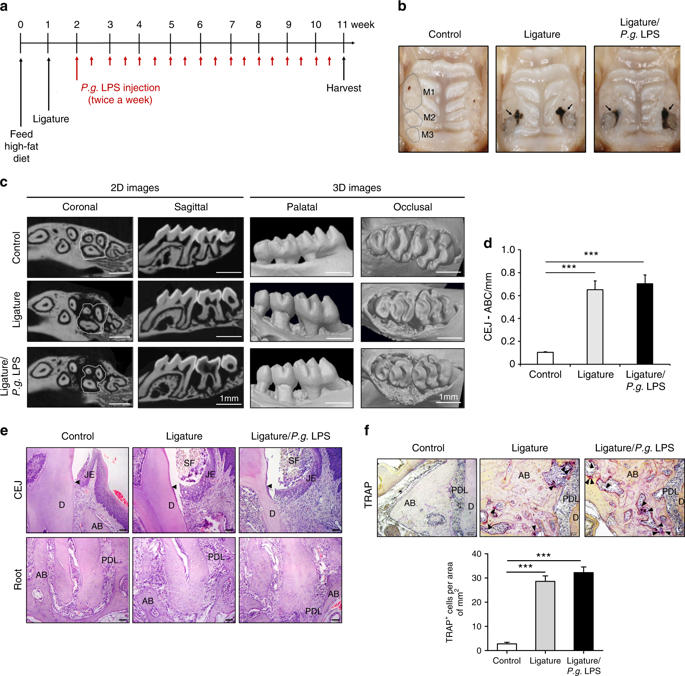
Growing evidence suggests close associations between periodontitis and atherosclerosis. To further understand the pathological relationships of these associations, we developed periodontitis with ligature placement around maxillary molars or ligature placement in conjunction with Porphyromonas gingivalis lipopolysaccharide injection at the ligature sites (ligature/P.g. LPS) in Apolipoprotein E knock out mice and studied the atherogenesis process in these animals. The mice were fed with high fat diet for 11 weeks and sacrificed for analyzing periodontitis, systemic inflammation, and atherosclerosis. Controls did not develop periodontitis or systemic inflammation and had minimal lipid deposition in the aortas, but mice receiving ligature or ligature/P.g. LPS showed severe periodontitis, systemic inflammation, and aortic plaque formation. The aortic plaque contained abundant macrophages and cells expressing both endothelial and mesenchymal cell markers. The severity of periodontitis was slightly higher in mice receiving ligature/P.g. LPS than ligature alone, and the magnitude of systemic inflammation and aortic plaque formation were also notably greater in the mice with ligature/P.g. LPS. These observations indicate that the development of atherosclerosis is due to systemic inflammation caused by severe periodontitis. In vitro, P.g. LPS enhanced the secretion of pro-inflammatory cytokines from macrophages and increased the adhesion of monocytes to endothelial cells by upregulating the expression of adhesion molecules from endothelial cells. Moreover, secretory proteins, such as TNF-α, from macrophages induced endothelial-mesenchymal transitions of the endothelial cells. Taken together, systemic inflammation induced by severe periodontitis might exacerbate atherosclerosis via, in part, causing aberrant functions of vascular endothelial cells and the activation of macrophages in mice.
中文翻译:

牙周炎引起的全身炎症在小鼠中部分通过内皮-间质转化加剧动脉粥样硬化。
越来越多的证据表明牙周炎和动脉粥样硬化之间存在密切关联。为了进一步了解这些关联的病理关系,我们在载脂蛋白 E 敲除小鼠的结扎部位(结扎/Pg LPS)开发了牙周炎,并在上颌磨牙周围结扎或结扎并结合牙龈卟啉单胞菌脂多糖注射液,并研究了动脉粥样硬化形成过程在这些动物中。小鼠被喂食高脂肪饮食 11 周,然后处死以分析牙周炎、全身炎症和动脉粥样硬化。对照组没有发生牙周炎或全身性炎症,主动脉中的脂质沉积最少,但接受结扎或结扎/Pg LPS 的小鼠表现出严重的牙周炎、全身性炎症和主动脉斑块形成。主动脉斑块含有丰富的巨噬细胞和表达内皮细胞和间充质细胞标记物的细胞。接受结扎/Pg LPS 的小鼠牙周炎的严重程度略高于仅接受结扎的小鼠,全身炎症和主动脉斑块形成的严重程度在接受结扎/Pg LPS 的小鼠中也明显更大。这些观察表明,动脉粥样硬化的发展是由于严重的牙周炎引起的全身炎症。在体外,Pg LPS 通过上调内皮细胞粘附分子的表达,增强巨噬细胞促炎细胞因子的分泌,并增加单核细胞对内皮细胞的粘附。此外,来自巨噬细胞的分泌蛋白,如 TNF-α,可诱导内皮细胞的内皮-间质转化。
更新日期:2019-07-01
中文翻译:

牙周炎引起的全身炎症在小鼠中部分通过内皮-间质转化加剧动脉粥样硬化。
越来越多的证据表明牙周炎和动脉粥样硬化之间存在密切关联。为了进一步了解这些关联的病理关系,我们在载脂蛋白 E 敲除小鼠的结扎部位(结扎/Pg LPS)开发了牙周炎,并在上颌磨牙周围结扎或结扎并结合牙龈卟啉单胞菌脂多糖注射液,并研究了动脉粥样硬化形成过程在这些动物中。小鼠被喂食高脂肪饮食 11 周,然后处死以分析牙周炎、全身炎症和动脉粥样硬化。对照组没有发生牙周炎或全身性炎症,主动脉中的脂质沉积最少,但接受结扎或结扎/Pg LPS 的小鼠表现出严重的牙周炎、全身性炎症和主动脉斑块形成。主动脉斑块含有丰富的巨噬细胞和表达内皮细胞和间充质细胞标记物的细胞。接受结扎/Pg LPS 的小鼠牙周炎的严重程度略高于仅接受结扎的小鼠,全身炎症和主动脉斑块形成的严重程度在接受结扎/Pg LPS 的小鼠中也明显更大。这些观察表明,动脉粥样硬化的发展是由于严重的牙周炎引起的全身炎症。在体外,Pg LPS 通过上调内皮细胞粘附分子的表达,增强巨噬细胞促炎细胞因子的分泌,并增加单核细胞对内皮细胞的粘附。此外,来自巨噬细胞的分泌蛋白,如 TNF-α,可诱导内皮细胞的内皮-间质转化。


























 京公网安备 11010802027423号
京公网安备 11010802027423号