Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
HIV incidence among women using intramuscular depot medroxyprogesterone acetate, a copper intrauterine device, or a levonorgestrel implant for contraception: a randomised, multicentre, open-label trial.
The Lancet ( IF 168.9 ) Pub Date : 2019-06-13 , DOI: 10.1016/s0140-6736(19)31288-7
The Lancet ( IF 168.9 ) Pub Date : 2019-06-13 , DOI: 10.1016/s0140-6736(19)31288-7
|
BACKGROUND
Observational and laboratory studies suggest that some hormonal contraceptive methods, particularly intramuscular depot medroxyprogesterone acetate (DMPA-IM), might increase women's susceptibility to HIV acquisition. We aimed to compare DMPA-IM, a copper intrauterine device (IUD), and a levonorgestrel (LNG) implant among African women seeking effective contraception and living in areas of high HIV incidence.
METHODS
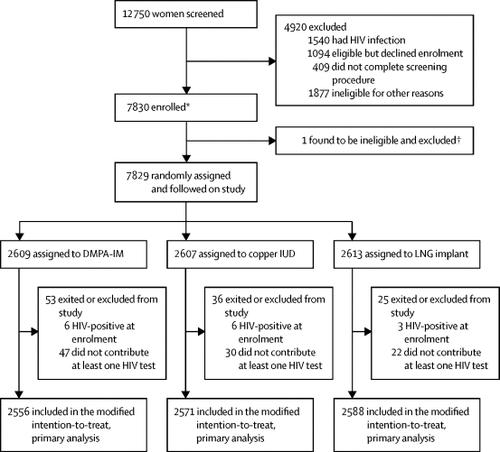
We did a randomised, multicentre, open-label trial across 12 research sites in eSwatini, Kenya, South Africa, and Zambia. We included HIV-seronegative women aged 16-35 years who were seeking effective contraception, had no medical contraindications to the trial contraceptive methods, agreed to use the assigned method for 18 months, and reported not using injectable, intrauterine, or implantable contraception for the previous 6 months. Participants were randomly assigned (1:1:1) to receive an injection of 150 mg/mL DMPA-IM every 3 months, a copper IUD, or a LNG implant with random block sizes between 15 and 30, stratified by site. Participants were assigned using an online randomisation system, which was accessed for each randomisation by study staff at each site. The primary endpoint was incident HIV infection in the modified intention-to-treat population, including all randomised participants who were HIV negative at enrolment and who contributed at least one HIV test. The primary safety endpoint was any serious adverse event or any adverse event resulting in method discontinuation, until the trial exit visit at 18 months and was assessed in all enrolled and randomly assigned women. This study is registered with ClinicalTrials.gov, number NCT02550067.
FINDINGS
Between Dec 14, 2015, and Sept 12, 2017, 7830 women were enrolled and 7829 were randomly assigned to the DMPA-IM group (n=2609), the copper IUD group (n=2607), or the LNG implant group (n=2613). 7715 (99%) participants were included in the modified intention-to-treat population (2556 in the DMPA-IM group, 2571 in the copper IUD group, and 2588 in the LNG implant group), and women used their assigned method for 9567 (92%) of 10 409 woman-years of follow-up time. 397 HIV infections occurred (incidence 3·81 per 100 woman-years [95% CI 3·45-4·21]): 143 (36%; 4·19 per 100 woman-years [3·54-4·94]) in the DMPA-IM group, 138 (35%: 3·94 per 100 woman-years [3·31-4·66]) in the copper IUD group, and 116 (29%; 3·31 per 100 woman-years [2·74-3·98]) in the LNG implant group. In the modified intention-to-treat analysis, the hazard ratios for HIV acquisition were 1·04 (96% CI 0·82-1·33, p=0·72) for DMPA-IM compared with copper IUD, 1·23 (0·95-1·59, p=0·097) for DMPA-IM compared with LNG implant, and 1·18 (0·91-1·53, p=0·19) for copper IUD compared with LNG implant. 12 women died during the study: six in the DMPA-IM group, five in the copper IUD group, and one in the LNG implant group. Serious adverse events occurred in 49 (2%) of 2609 participants in the DMPA-IM group, 92 (4%) of 2607 participants in the copper IUD group, and 78 (3%) of 2613 participants in the LNG implant group. Adverse events resulting in discontinuation of the randomly assigned method occurred in 109 (4%) women in the DMPA-IM group, 218 (8%) women in the copper IUD group, and 226 (9%) women in the LNG implant group (p<0·0001 for DMPA-IM vs copper IUD and for DMPA-IM vs LNG implant). 255 pregnancies occurred: 61 (24%) in the DMPA-IM group, 116 (45%) in the copper IUD group, and 78 (31%) in the LNG implant group. 181 (71%) pregnancies occurred after discontinuation of randomly assigned method.
INTERPRETATION
We did not find a substantial difference in HIV risk among the methods evaluated, and all methods were safe and highly effective. HIV incidence was high in this population of women seeking pregnancy prevention, emphasising the need for integration of HIV prevention within contraceptive services for African women. These results support continued and increased access to these three contraceptive methods.
FUNDING
Bill & Melinda Gates Foundation, US Agency for International Development and the President's Emergency Plan for AIDS Relief, Swedish International Development Cooperation Agency, South African Medical Research Council, and UN Population Fund. Contraceptive supplies were donated by the Government of South Africa and US Agency for International Development.
中文翻译:

使用肌内注射醋酸甲羟孕酮,子宫内铜器械或左炔诺孕酮植入物进行避孕的妇女中的艾滋病毒发生率:一项随机,多中心,开放标签的试验。
背景技术观察和实验室研究表明,某些激素避孕方法,特别是肌内注射醋酸甲羟孕酮(DMPA-IM),可能会增加女性对HIV感染的易感性。我们旨在比较寻求有效避孕并生活在艾滋病毒高发地区的非洲妇女中的DMPA-IM,子宫内铜制器械(IUD)和左炔诺孕酮(LNG)植入物。方法我们在eSwatini,肯尼亚,南非和赞比亚的12个研究地点进行了一项随机,多中心,开放标签的试验。我们纳入了16-35岁的HIV血清阴性妇女,这些妇女正在寻求有效的避孕措施,对试验性避孕方法没有医学上的禁忌症,同意使用指定的方法治疗18个月,并且报告未使用可注射的宫内节育器,或过去6个月内的可植入避孕药。参与者被随机分配(1:1:1:1),每3个月注射150 mg / mL DMPA-IM,铜制宫内节育器或LNG植入物,其随机块大小在15到30之间,并按部位分层。使用在线随机分配系统分配参与者,每个站点的研究人员均可进行每次随机分配。主要终点是经过改良的意向性治疗人群中的艾滋病毒感染事件,包括所有入选时均为HIV阴性且贡献了至少一项HIV检测的随机参与者。主要安全终点是任何严重不良事件或导致方法中断的任何不良事件,直到18个月的试验出诊时为止,并在所有入组和随机分配的妇女中进行了评估。该研究已在ClinicalTrials.gov上注册,编号为NCT02550067。结果在2015年12月14日至2017年9月12日之间,招募了7830名女性,并将7829名女性随机分为DMPA-IM组(n = 2609),铜制IUD组(n = 2607)或LNG植入组( n = 2613)。改良的意向性治疗人群中包括7715名(99%)参与者(DMPA-IM组为2556名,铜制宫内节育器组为2571名,LNG植入物组为2588名),女性使用了指定的方法治疗9567名10 409个女性年的随访时间中,有92%(92%)。发生了397例HIV感染(每100名妇女年3·81发生率[95%CI 3·45-4·21]):143(36%;每100名妇女年4·19 [3·54-4·94] )在DMPA-IM组中,铜宫内节育器组为138(35%:每100个妇女年3·94 [3·31-4·66]),在116个宫内节育器组中为116(29%;每100个妇女年3·31-年[2·74-3·98])。在改进的意向性治疗分析中,与铜制宫内节育器相比,DMPA-IM的HIV感染危险比为1·04(96%CI 0·82-1·33,p = 0·72)。与LNG植入物相比,DMPA-IM的(0·95-1·59,p = 0·097),与LNG植入物相比,铜宫内节育器的1·18(0·91-1·53,p = 0·19) 。研究期间有12名妇女死亡:DMPA-IM组中有6名妇女,铜制IUD组中有5名妇女,LNG植入组中有1名妇女。DMPA-IM组的2609名参与者中有49名(2%)发生严重不良事件,铜制IUD组的2607名参与者中有92名(4%),LNG植入组的2613名参与者中有78名(3%)。DMPA-IM组中有109名(4%)妇女,铜制IUD组中的218名妇女(4%)和LNG植入组中的226名妇女(9%)发生了导致终止随机分配方法的不良事件( p < 对于DMPA-IM与铜制宫内节育器以及对于DMPA-IM与LNG植入物,则为0·0001)。发生了255次怀孕:DMPA-IM组为61(24%),铜宫内节育器组为116(45%),LNG植入组为78(31%)。终止随机分配的方法后发生181例(71%)怀孕。解释我们在所评估的方法之间未发现HIV风险有实质性差异,并且所有方法都是安全且高效的。寻求预防怀孕的这一群体的妇女中艾滋病毒的发病率很高,强调必须将预防艾滋病毒纳入针对非洲妇女的避孕服务中。这些结果支持继续使用这三种避孕方法,并增加了使用这三种避孕方法的机会。资金Bill&Melinda Gates基金会,美国国际开发署和总统的艾滋病紧急救援计划,瑞典国际开发合作署,南非医学研究理事会和联合国人口基金。南非政府和美国国际开发署捐赠了避孕用品。
更新日期:2019-07-26
中文翻译:

使用肌内注射醋酸甲羟孕酮,子宫内铜器械或左炔诺孕酮植入物进行避孕的妇女中的艾滋病毒发生率:一项随机,多中心,开放标签的试验。
背景技术观察和实验室研究表明,某些激素避孕方法,特别是肌内注射醋酸甲羟孕酮(DMPA-IM),可能会增加女性对HIV感染的易感性。我们旨在比较寻求有效避孕并生活在艾滋病毒高发地区的非洲妇女中的DMPA-IM,子宫内铜制器械(IUD)和左炔诺孕酮(LNG)植入物。方法我们在eSwatini,肯尼亚,南非和赞比亚的12个研究地点进行了一项随机,多中心,开放标签的试验。我们纳入了16-35岁的HIV血清阴性妇女,这些妇女正在寻求有效的避孕措施,对试验性避孕方法没有医学上的禁忌症,同意使用指定的方法治疗18个月,并且报告未使用可注射的宫内节育器,或过去6个月内的可植入避孕药。参与者被随机分配(1:1:1:1),每3个月注射150 mg / mL DMPA-IM,铜制宫内节育器或LNG植入物,其随机块大小在15到30之间,并按部位分层。使用在线随机分配系统分配参与者,每个站点的研究人员均可进行每次随机分配。主要终点是经过改良的意向性治疗人群中的艾滋病毒感染事件,包括所有入选时均为HIV阴性且贡献了至少一项HIV检测的随机参与者。主要安全终点是任何严重不良事件或导致方法中断的任何不良事件,直到18个月的试验出诊时为止,并在所有入组和随机分配的妇女中进行了评估。该研究已在ClinicalTrials.gov上注册,编号为NCT02550067。结果在2015年12月14日至2017年9月12日之间,招募了7830名女性,并将7829名女性随机分为DMPA-IM组(n = 2609),铜制IUD组(n = 2607)或LNG植入组( n = 2613)。改良的意向性治疗人群中包括7715名(99%)参与者(DMPA-IM组为2556名,铜制宫内节育器组为2571名,LNG植入物组为2588名),女性使用了指定的方法治疗9567名10 409个女性年的随访时间中,有92%(92%)。发生了397例HIV感染(每100名妇女年3·81发生率[95%CI 3·45-4·21]):143(36%;每100名妇女年4·19 [3·54-4·94] )在DMPA-IM组中,铜宫内节育器组为138(35%:每100个妇女年3·94 [3·31-4·66]),在116个宫内节育器组中为116(29%;每100个妇女年3·31-年[2·74-3·98])。在改进的意向性治疗分析中,与铜制宫内节育器相比,DMPA-IM的HIV感染危险比为1·04(96%CI 0·82-1·33,p = 0·72)。与LNG植入物相比,DMPA-IM的(0·95-1·59,p = 0·097),与LNG植入物相比,铜宫内节育器的1·18(0·91-1·53,p = 0·19) 。研究期间有12名妇女死亡:DMPA-IM组中有6名妇女,铜制IUD组中有5名妇女,LNG植入组中有1名妇女。DMPA-IM组的2609名参与者中有49名(2%)发生严重不良事件,铜制IUD组的2607名参与者中有92名(4%),LNG植入组的2613名参与者中有78名(3%)。DMPA-IM组中有109名(4%)妇女,铜制IUD组中的218名妇女(4%)和LNG植入组中的226名妇女(9%)发生了导致终止随机分配方法的不良事件( p < 对于DMPA-IM与铜制宫内节育器以及对于DMPA-IM与LNG植入物,则为0·0001)。发生了255次怀孕:DMPA-IM组为61(24%),铜宫内节育器组为116(45%),LNG植入组为78(31%)。终止随机分配的方法后发生181例(71%)怀孕。解释我们在所评估的方法之间未发现HIV风险有实质性差异,并且所有方法都是安全且高效的。寻求预防怀孕的这一群体的妇女中艾滋病毒的发病率很高,强调必须将预防艾滋病毒纳入针对非洲妇女的避孕服务中。这些结果支持继续使用这三种避孕方法,并增加了使用这三种避孕方法的机会。资金Bill&Melinda Gates基金会,美国国际开发署和总统的艾滋病紧急救援计划,瑞典国际开发合作署,南非医学研究理事会和联合国人口基金。南非政府和美国国际开发署捐赠了避孕用品。


























 京公网安备 11010802027423号
京公网安备 11010802027423号