当前位置:
X-MOL 学术
›
npj Prim. Care Respir. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
The impact of integrated disease management in high-risk COPD patients in primary care.
npj Primary Care Respiratory Medicine ( IF 3.1 ) Pub Date : 2019-03-28 , DOI: 10.1038/s41533-019-0119-9 Madonna Ferrone 1, 2 , Marcello G Masciantonio 1, 3 , Natalie Malus 1, 3 , Larry Stitt 4 , Tim O'Callahan 5 , Zofe Roberts 1 , Laura Johnson 6 , Jim Samson 7 , Lisa Durocher 7 , Mark Ferrari 8 , Margo Reilly 9 , Kelly Griffiths 10 , Christopher J Licskai 1, 3, 4 ,
npj Primary Care Respiratory Medicine ( IF 3.1 ) Pub Date : 2019-03-28 , DOI: 10.1038/s41533-019-0119-9 Madonna Ferrone 1, 2 , Marcello G Masciantonio 1, 3 , Natalie Malus 1, 3 , Larry Stitt 4 , Tim O'Callahan 5 , Zofe Roberts 1 , Laura Johnson 6 , Jim Samson 7 , Lisa Durocher 7 , Mark Ferrari 8 , Margo Reilly 9 , Kelly Griffiths 10 , Christopher J Licskai 1, 3, 4 ,
Affiliation
|
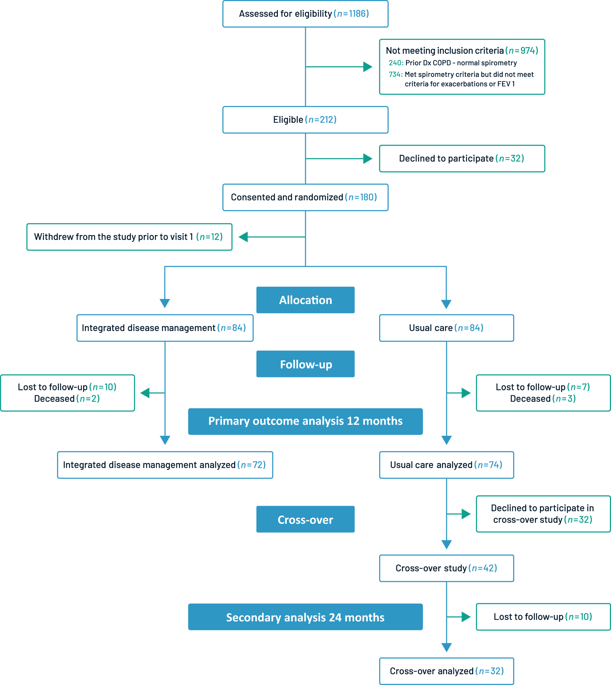
Patients with chronic obstructive pulmonary disease (COPD) have a reduced quality of life (QoL) and exacerbations that drive health service utilization (HSU). A majority of patients with COPD are managed in primary care. Our objective was to evaluate an integrated disease management, self-management, and structured follow-up intervention (IDM) for high-risk patients with COPD in primary care. This was a one-year multi-center randomized controlled trial. High-risk, exacerbation-prone COPD patients were randomized to IDM provided by a certified respiratory educator and physician, or usual physician care. IDM received case management, self-management education, and skills training. The primary outcome, COPD-related QoL, was measured using the COPD Assessment Test (CAT). Of 180 patients randomized from 8 sites, 81.1% completed the study. Patients were 53.6% women, mean age 68.2 years, post-bronchodilator FEV1 52.8% predicted, and 77.4% were Global Initiative for Obstructive Lung Disease Stage D. QoL-CAT scores improved in IDM patients, 22.6 to 14.8, and worsened in usual care, 19.3 to 22.0, adjusted difference 9.3 (p < 0.001). Secondary outcomes including the Clinical COPD Questionnaire, Bristol Knowledge Questionnaire, and FEV1 demonstrated differential improvements in favor of IDM of 1.29 (p < 0.001), 29.6% (p < 0.001), and 100 mL, respectively (p = 0.016). Compared to usual care, significantly fewer IDM patients had a severe exacerbation, -48.9% (p < 0.001), required an urgent primary care visit for COPD, -30.2% (p < 0.001), or had an emergency department visit, -23.6% (p = 0.001). We conclude that IDM self-management and structured follow-up substantially improved QoL, knowledge, FEV1, reduced severe exacerbations, and HSU, in a high-risk primary care COPD population. Clinicaltrials.gov NCT02343055.
中文翻译:

综合疾病管理对初级保健中高风险COPD患者的影响。
患有慢性阻塞性肺疾病(COPD)的患者的生活质量(QoL)降低,病情加重,推动了医疗服务的利用(HSU)。大多数COPD患者在初级保健中接受治疗。我们的目标是评估针对初级保健中COPD高危患者的综合疾病管理,自我管理和结构化的后续干预(IDM)。这是一项为期一年的多中心随机对照试验。高危,易发作的COPD患者被随机分配到由认证的呼吸教育者和医师提供的IDM或常规医师的护理。IDM接受了案例管理,自我管理教育和技能培训。使用COPD评估测试(CAT)测量了主要结局,即COPD相关的QoL。从8个地点随机分配的180名患者中,有81.1%完成了研究。患者为53.6%的女性,平均年龄为68.2岁,预计支气管扩张剂后FEV1为52.8%,全球阻塞性肺疾病D期倡议为77.4%。IDM患者的QoL-CAT评分提高了,从22.6降低到14.8,在常规护理中恶化了,从19.3到22.0,调整后的差值为9.3(p <0.001)。次要结果包括临床COPD问卷,Bristol知识问卷和FEV1,分别显示IDM的差异有所改善,IDM分别为1.29(p <0.001),29.6%(p <0.001)和100 mL(p = 0.016)。与常规护理相比,严重加重病的IDM患者明显减少,为-48.9%(p <0.001),需要进行COPD的紧急初级护理就诊,为-30.2%(p <0.001),或者有急诊就诊,为-23.6 %(p = 0.001)。我们得出的结论是,在高风险的初级保健COPD人群中,IDM的自我管理和结构化的随访大大改善了QoL,知识,FEV1,减轻了严重加重和HSU。Clinicaltrials.gov NCT02343055。
更新日期:2019-11-18
中文翻译:

综合疾病管理对初级保健中高风险COPD患者的影响。
患有慢性阻塞性肺疾病(COPD)的患者的生活质量(QoL)降低,病情加重,推动了医疗服务的利用(HSU)。大多数COPD患者在初级保健中接受治疗。我们的目标是评估针对初级保健中COPD高危患者的综合疾病管理,自我管理和结构化的后续干预(IDM)。这是一项为期一年的多中心随机对照试验。高危,易发作的COPD患者被随机分配到由认证的呼吸教育者和医师提供的IDM或常规医师的护理。IDM接受了案例管理,自我管理教育和技能培训。使用COPD评估测试(CAT)测量了主要结局,即COPD相关的QoL。从8个地点随机分配的180名患者中,有81.1%完成了研究。患者为53.6%的女性,平均年龄为68.2岁,预计支气管扩张剂后FEV1为52.8%,全球阻塞性肺疾病D期倡议为77.4%。IDM患者的QoL-CAT评分提高了,从22.6降低到14.8,在常规护理中恶化了,从19.3到22.0,调整后的差值为9.3(p <0.001)。次要结果包括临床COPD问卷,Bristol知识问卷和FEV1,分别显示IDM的差异有所改善,IDM分别为1.29(p <0.001),29.6%(p <0.001)和100 mL(p = 0.016)。与常规护理相比,严重加重病的IDM患者明显减少,为-48.9%(p <0.001),需要进行COPD的紧急初级护理就诊,为-30.2%(p <0.001),或者有急诊就诊,为-23.6 %(p = 0.001)。我们得出的结论是,在高风险的初级保健COPD人群中,IDM的自我管理和结构化的随访大大改善了QoL,知识,FEV1,减轻了严重加重和HSU。Clinicaltrials.gov NCT02343055。



























 京公网安备 11010802027423号
京公网安备 11010802027423号