Gastroenterology ( IF 29.4 ) Pub Date : 2023-05-27 , DOI: 10.1053/j.gastro.2023.05.028 Dóra Czapári 1 , Alex Váradi 2 , Nelli Farkas 3 , Gergely Nyári 4 , Katalin Márta 5 , Szilárd Váncsa 6 , Rita Nagy 7 , Brigitta Teutsch 1 , Stefania Bunduc 8 , Bálint Erőss 6 , László Czakó 9 , Áron Vincze 10 , Ferenc Izbéki 11 , Mária Papp 12 , Béla Merkely 13 , Andrea Szentesi 14 , Péter Hegyi 15 ,
|
Background & Aims
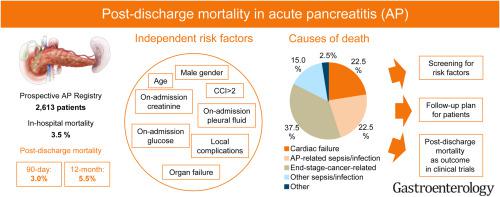
The in-hospital survival of patients suffering from acute pancreatitis (AP) is 95% to 98%. However, there is growing evidence that patients discharged after AP may be at risk of serious morbidity and mortality. Here, we aimed to investigate the risk, causes, and predictors of the most severe consequence of the post-AP period: mortality.
Methods
A total of 2613 well-characterized patients from 25 centers were included and followed by the Hungarian Pancreatic Study Group between 2012 and 2021. A general and a hospital-based population was used as the control group.
Results
After an AP episode, patients have an approximately threefold higher incidence rate of mortality than the general population (0.0404 vs 0.0130 person-years). First-year mortality after discharge was almost double than in-hospital mortality (5.5% vs 3.5%), with 3.0% occurring in the first 90-day period. Age, comorbidities, and severity were the most significant independent risk factors for death following AP. Furthermore, multivariate analysis identified creatinine, glucose, and pleural fluid on admission as independent risk factors associated with post-discharge mortality. In the first 90-day period, cardiac failure and AP-related sepsis were among the main causes of death following discharge, and cancer-related cachexia and non–AP-related infection were the key causes in the later phase.
Conclusion
Almost as many patients in our cohort died in the first 90-day period after discharge as during their hospital stay. Evaluation of cardiovascular status, follow-up of local complications, and cachexia-preventing oncological care should be an essential part of post-AP patient care. Future study protocols in AP must include at least a 90-day follow-up period after discharge.
中文翻译:

急性胰腺炎出院后死亡率的详细特征
背景与目标
急性胰腺炎(AP)患者的院内生存率为 95% 至 98%。然而,越来越多的证据表明,AP 后出院的患者可能面临严重发病和死亡的风险。在这里,我们的目的是调查 AP 后时期最严重后果:死亡率的风险、原因和预测因素。
方法
匈牙利胰腺研究组在 2012 年至 2021 年间共纳入了来自 25 个中心的 2613 名特征明确的患者。普通人群和医院人群被用作对照组。
结果
AP 发作后,患者的死亡率大约是普通人群的三倍(0.0404 人年 vs 0.0130 人年)。出院后第一年死亡率几乎是住院死亡率的两倍(5.5% vs 3.5%),其中 3.0% 发生在前 90 天。年龄、合并症和严重程度是 AP 后死亡的最重要的独立危险因素。此外,多变量分析确定入院时的肌酐、葡萄糖和胸腔积液是与出院后死亡率相关的独立危险因素。在前90天内,心力衰竭和AP相关脓毒症是出院后死亡的主要原因,而癌症相关恶病质和非AP相关感染是后期的主要原因。
结论
我们队列中的患者在出院后 90 天内死亡的人数几乎与住院期间死亡的人数一样多。心血管状况的评估、局部并发症的随访以及预防恶病质的肿瘤护理应该是 AP 后患者护理的重要组成部分。AP 未来的研究方案必须包括出院后至少 90 天的随访期。



























 京公网安备 11010802027423号
京公网安备 11010802027423号